WO2001097843A2 - Methods for enhancing antibody-induced cell lysis and treating cancer - Google Patents
Methods for enhancing antibody-induced cell lysis and treating cancer Download PDFInfo
- Publication number
- WO2001097843A2 WO2001097843A2 PCT/US2001/020154 US0120154W WO0197843A2 WO 2001097843 A2 WO2001097843 A2 WO 2001097843A2 US 0120154 W US0120154 W US 0120154W WO 0197843 A2 WO0197843 A2 WO 0197843A2
- Authority
- WO
- WIPO (PCT)
- Prior art keywords
- nucleic acid
- antibody
- cancer
- cell
- lymphoma
- Prior art date
Links
Classifications
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
- C07K16/28—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants
- C07K16/2896—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants against molecules with a "CD"-designation, not provided for elsewhere
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/395—Antibodies; Immunoglobulins; Immune serum, e.g. antilymphocytic serum
- A61K39/39533—Antibodies; Immunoglobulins; Immune serum, e.g. antilymphocytic serum against materials from animals
- A61K39/39541—Antibodies; Immunoglobulins; Immune serum, e.g. antilymphocytic serum against materials from animals against normal tissues, cells
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P35/00—Antineoplastic agents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P35/00—Antineoplastic agents
- A61P35/02—Antineoplastic agents specific for leukemia
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P35/00—Antineoplastic agents
- A61P35/04—Antineoplastic agents specific for metastasis
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P43/00—Drugs for specific purposes, not provided for in groups A61P1/00-A61P41/00
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
- C07K16/28—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants
- C07K16/2803—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants against the immunoglobulin superfamily
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
- C07K16/28—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants
- C07K16/2878—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants against the NGF-receptor/TNF-receptor superfamily, e.g. CD27, CD30, CD40, CD95
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/505—Medicinal preparations containing antigens or antibodies comprising antibodies
Definitions
- the invention relates to the treatment and prevention of cancer using immunostimulatory nucleic acids and antibodies.
- Cancer is a disease which involves the uncontrolled growth (i.e., division) of cells.
- Some of the known mechanisms which contribute to the uncontrolled proliferation of cancer cells include growth factor independence, failure to detect genomic mutation, and inappropriate cell signaling. The ability of cancer cells to ignore normal growth controls may result in an increased rate of proliferation.
- the causes of cancer have not been firmly established, there are some factors known to contribute, or at least predispose a subject, to cancer. Such factors include particular genetic mutations (e.g., BRCA gene mutation for breast cancer, APC for colon cancer), exposure to suspected cancer-causing agents, or carcinogens (e.g., asbestos, UN radiation) and familial disposition for particular cancers such as breast cancer.
- Cancer is currently treated using a variety of modalities including surgery, radiation therapy and chemotherapy.
- the choice of treatment modality will depend upon the type, location and dissemination of the cancer.
- surgery and radiation therapy may be more appropriate in the case of solid well-defined tumor masses and less practical in the case of non-solid tumor cancers such as leukemia and lymphoma.
- One of the advantages of surgery and radiation therapy is the ability to control to some extent the impact of the therapy, and thus to limit the toxicity to normal tissues in the body.
- surgery and radiation therapy are often followed by chemotherapy to guard against any remaining or radio-resistant cancer cells.
- Chemotherapy is also the most appropriate treatment for disseminated cancers such as leukemia and lymphoma as well as metastases.
- CpG DNA unmethylated CG-dinucleotides within certain sequence contexts
- CpG DNA activates a coordinated set of immune responses that include innate immunity (macrophages, dendritic cells, and natural killer cells), humoral immunity, and cellular immunity.
- innate immunity macrophages, dendritic cells, and natural killer cells
- humoral immunity and cellular immunity.
- Krieg AM et al. Pharmacol Ther 84:113- 20 (1999); Krieg AM et al., Curr Top Microbiol Immunol 247:1-21 (2000); Wagner H, Adv Immunol 73:329-68 (1999).
- CpG DNA is at least as effective as the gold standard complete Freund's adjuvant (CFA), but induces higher Thl activity and demonstrates less toxicity.
- CFA complete Freund's adjuvant
- the invention relates in some aspects to methods for treating and preventing cancer using immunostimulatory nucleic acids and antibodies.
- the invention is a method for treating or preventing cancer.
- the method involves administering to a subject having or at risk of developing cancer an effective amount to upregulate CD20 expression of a nucleic acid, and an anti-CD20 antibody.
- the cancer in some embodiments, is B-cell lymphoma associated with low levels of CD20 expression.
- the B-cell lymphoma in other embodiments is B-cell chronic lymphocytic leukemia (B-CLL) or a marginal zone lymphoma.
- the CD20 antibody is C2B8 or Rituximab.
- the invention in other aspects relates to a method for diagnosing lymphoma by isolating a B cell from a subject and identifying a change in cell surface markers when the B cell is contacted with an immunostimulatory nucleic acid, wherein the cell surface marker induced on the B cell is indicative of the type of lymphoma.
- the subject has a type of lymphoma.
- the subject is suspected of having a type of lymphoma.
- the method may optionally include a method for treating cancer by administering to the subject an immunostimulatory nucleic acid and an antibody specific for the cell surface antigens induced on the B cell in order to treat the cancer.
- the invention is a method for treating or preventing cancer by administering to a subject having or at risk of developing cancer an effective amount to induce expression of a surface antigen on a cancer cell surface, of a nucleic acid, and administering to the subject an antibody selected from the group consisting of an anti-CD22 antibody and an anti-CD 19 antibody.
- a method for treating lymphoma includes the steps of isolating a B cell from a subject having lymphoma, identifying a surface antigen which is not expressed or which is expressed on the surface of the B cell in an amount lower than that of a control B cell, administering to the subject an antibody specific for the identified surface antigen and an immunostimulatory nucleic acid in order to treat the lymphoma, wherein the nucleic acid is administered in an effective amount to upregulate expression of the surface antigen on the lymphoma cell surface.
- a method for treating a lymphoma resistant to antibody therapy includes administering to a subject having a lymphoma resistant to therapy with an antibody specific for a surface antigen, an antibody specific for the surface antigen to which the lymphoma is resistant and a nucleic acid in order to treat the lymphoma, wherein the nucleic acid is administered in an effective amount to upregulate expression of the surface antigen on the lymphoma cell surface.
- the surface antigen may be any type of surface antigen which is capable of being expressed on the surface of a cancer cell and which is induced by stimulation with immunostimulatory nucleic acids.
- the surface antigen is CD20, CD40, CD22, or CD19.
- the lymphoma is B-CLL or marginal zone lymphoma.
- the antibody is an anti-CD20 antibody, hi some embodiments the anti-CD20 antibody is C2B8. In another embodiment the anti-CD20 antibody is Rituximab. In some preferred embodiments the antibody is a human IgGl antibody. In some preferred embodiments the antibody is a murine IgG2a antibody. hi some embodiments the methods also include administering an anti-cancer therapy to the subject.
- the invention also includes a method for treating cancer in a human by administering to a human an immunostimulatory nucleic acid and an antibody of IgGl isotype (an IgGl isotype antibody as used herein refers to a human or humanized IgGl unless otherwise specified), which binds to a cell surface antigen of a cancer cell and wherein the nucleic acid and the antibody are administered in an effective amount for killing the cancer cell.
- the nucleic acid and the antibody are administered together.
- the nucleic acid and the antibody may be administered separately.
- the method includes the step of administering a cancer therapy.
- a cancer therapy is meant to embrace a single medicament, a plurality of medicaments of a particular class and a plurality of medicaments of different classes, and includes but is not limited to chemotherapeutic agents, cancer vaccines, biological response modifiers, and hormone therapies.
- a chemotherapeutic agent maybe selected from the group consisting of methotrexate, vincristine, adriamycin, cisplatin, non-sugar containing chloroethylnitrosoureas, 5- fluorouracil, mitomycin C, bleomycin, doxorubicin, dacarbazine, taxol, fragyline, Meglamine GLA, valrubicin, carmustaine and poliferposan, MMI270, BAY 12-9566, RAS famesyl transferase inhibitor, famesyl transferase inhibitor, MMP, MTA/LY231514, LY264618/Lometexol, Glamolec, CI-994, TNP-470, Hycamtin/Topotecan, PKC412, Valspodar/PSC833, Novantrone/Mitroxantrone, Metaret/Suramin, Batimastat, E7070, BCH- 4556, CS-682, 9
- Mitoguazone methyl-GAG; methyl glyoxal bis-guanylhydrazone; MGBG
- Pentostatin (2'deoxycoformycin
- Semustine methyl-CCNU
- Teniposide VM-26
- Vindesine sulfate Vindesine sulfate.
- the chemotherapeutic agent may be selected from the group consisting of methotrexate, vincristine, adriamycin, cisplatin, mitomycin C, bleomycin, doxorubicin, dacarbazine, taxol, valrubicin, Novantrone/Mitroxantrone, Evacet/liposomal doxorubicin, Yewtaxan Paclitaxel, Taxol/Paclitaxel, SPU-077/Cisplatin, HMR 1275/Flavopiridol, BMS-182751/oral platinum, Leustatin/Cladribine, Paxex/Paclitaxel, Doxil/liposomal doxorubicin, Caelyx/liposomal doxorubicin, Fludara/Fludarabine, Pharmarubicin/Epirubicin, DepoCyt, Caetyx/liposomal doxorubicin
- a cancer vaccine may be selected from the group consisting of EGF, Anti-idiotypic cancer vaccines, Gp75 antigen, GMK melanoma vaccine, MGV ganglioside conjugate vaccine, Her2/neu, Ovarex, M-Vax, O-Vax, L-Vax, STn-KHL theratope, BLP25 (MUC-1), liposomal idiotypic vaccine, Melacine, peptide antigen vaccines, toxin/antigen vaccines, MVA-based vaccine, PACIS, BCG vaccine, TA-HPV, TA-CLN, DISC-virus and hnmuCyst/TheraCys.
- Biological response modifiers include interferon, and lymphokines such as IL-2.
- Hormone replacement therapy includes tamoxifen alone or in combination with progesterone.
- the cancer therapy is interferon- ⁇ (e.g., INTRON® A, Schering).
- the cancer may be selected from the group consisting of basal cell carcinoma, bladder cancer, bone cancer, brain and central nervous system (CNS) cancer, breast cancer, cervical cancer, colon and rectum cancer, connective tissue cancer, esophageal cancer, eye cancer, kidney cancer, larynx cancer, leukemia, liver cancer, lung cancer, Hodgkin's lymphoma, non- Hodgkin's lymphoma, melanoma, myeloma, oral cavity cancer (e.g., lip, tongue, mouth, and pharynx), ovarian cancer, pancreatic cancer, prostate cancer, rhabdomyosarcoma, skin cancer, stomach cancer, testicular cancer, and uterine cancer.
- CNS central nervous system
- the cancer to be treated may be selected from the group consisting of bone cancer, brain and CNS cancer, connective tissue cancer, esophageal cancer, eye cancer, Hodgkin's lymphoma, larynx cancer, oral cavity cancer (e.g., lip, tongue, mouth, and pharynx), skin cancer, and testicular cancer.
- the invention encompasses a kit.
- the kit includes a package including at least two containers, the first container housing an immunostimulatory nucleic acid, the second container housing an antibody specific for a cell surface antigen, and instructions for screening a cell to determine whether the immunostimulatory nucleic acid upregulates expression of the cell surface antigen.
- the antibody is selected from the group consisting of an anti-CD20 antibody, an anti-CD 19 antibody, and an anti-CD22 antibody.
- the nucleic acids useful according to the invention are immunostimulatory nucleic acids and in some embodiments are immunostimulatory CpG nucleic acids having an unmethylated CpG motif, immunostimulatory T-rich nucleic acids, immunostimulatory poly-
- G nucleic acids, bacterial DNA, yeast DNA, or eukaryotic DNA.
- nucleic acid does not hybridize with genomic DNA or RNA under stringent conditions. In other embodiments the nucleic acid does hybridize with genomic DNA or RNA under stringent conditions.
- the nucleic acid may have natural linkages or may include at least one modified backbone internucleotide linkage.
- the modified backbone is a phosphate backbone modification.
- the modified backbone is a peptide modified oligonucleotide backbone.
- the nucleic acid may also include native bases or modified bases.
- the nucleotide backbone may be chimeric, or the nucleotide backbone is entirely modified.
- the immunostimulatory nucleic acid can have any length greater than 6 nucleotides, but in some embodiments is between 8 and 100 nucleotide residues in length. In other embodiments the nucleic acid comprises at least 20 nucleotides, at least 24 nucleotides, at least 27, nucleotides, or at least 30 nucleotides. The nucleic acid may be single-stranded or double-stranded. In some embodiments the nucleic acid is isolated and in other embodiments the nucleic acid may be a synthetic nucleic acid.
- the CpG nucleic acid in one embodiment contains at least one unmethylated CpG dinucleotide having a sequence including at least the following formula: 5' X ⁇ X CGX X 3' wherein C is unmethylated, wherein Xi, X 2 , X , and X 4 are nucleotides.
- the 5' X ⁇ X CGX 3 X 3' sequence of the CpG nucleic acid is a non-palindromic sequence, and in other embodiments it is a palindromic sequence.
- X 1 X2 are nucleotides selected from the group consisting of:
- X ⁇ X 2 are GpA or GpT and X 3 X 4 are
- Xi or X 2 or both are purines and X 3 or X or both are pyrimidines or X ⁇ X 2 are GpA and X 3 or X-j or both are pyrimidines.
- X 2 is a T and X 3 is a pyrimidine.
- the CpG nucleic acid has a sequence selected from the group consisting of SEQ ID NOs: 19, 35-37, 39-42, 91, 92, 101, 108, 111, 135, 141, 151, 274, 277,
- the T-rich immunostimulatory nucleic acid is a poly-T nucleic acid comprising 5' TTTT 3'.
- the poly-T nucleic acid comprises 5' X ⁇ X 2 TTTTX 3 X 3' wherein Xi, X 2 , X 3 , and X are nucleotides.
- X ⁇ X 2 is TT and/or X 3 X 4 is TT.
- X ⁇ X 2 is selected from the group consisting of TA, TG, TC, AT, AA, AG, AC, CT, CC, CA, CG, GT, GG, GA, and GC; and or X 3 X 4 is selected from the group consisting of TA, TG, TC, AT, AA, AG, AC, CT, CC, CA, CG, GT, GG, GA, and GC.
- the T-rich immunostimulatory nucleic acid may have only a single poly-T motif or it may have a plurality of poly-T nucleic acid motifs.
- the T-rich immunostimulatory nucleic acid comprises at least 2, at least 3, at least 4, at least 5, at least 6, at least 7, or at least 8 T motifs. In other embodiments it comprises at least 2, at least 3, at least 4, at least 5, at least 6, at least 7, or at least 8 CpG motifs. In some embodiments the plurality of CpG motifs and poly-T motifs are interspersed.
- At least one of the plurality of poly-T motifs comprises at least 3, at least 4, at least 5, at least 6, at least 7, at least 8, or at least 9 contiguous T nucleotide residues.
- the plurality of poly-T motifs is at least 3 motifs and wherein at least 3 motifs each comprises at least 3 contiguous T nucleotide residues or the plurality of poly-T motifs is at least 4 motifs and wherein the at least 4 motifs each comprises at least 3 contiguous T nucleotide residues.
- the T-rich immunostimulatory nucleic acid may include one or more CpG motifs, h other embodiments the T-rich immunostimulatory nucleic acid is free of one or more CpG dinucleotides. In other embodiments the T-rich immunostimulatory nucleic acid has poly A, poly-G, and/or poly C motifs. In other embodiments the T-rich immunostimulatory nucleic acid is free of two poly C sequences of at least 3 contiguous C nucleotide residues. Preferably the T- rich immunostimulatory nucleic acid is free of two poly A sequences of at least 3 contiguous A nucleotide residues.
- the T-rich immunostimulatory nucleic acid comprises a nucleotide composition of greater than 25% C or greater than 25% A. In yet other embodiments the T-rich immunostimulatory nucleic acid is free of poly-C sequences, poly-G sequences or poly-A sequences. In some cases the T-rich immunostimulatory nucleic acid may be free of poly-T motifs, but rather, comprises a nucleotide composition of greater than 25% T. In other embodiments the T-rich immunostimulatory nucleic acid may have poly-T motifs and also comprise a nucleotide composition of greater than 25% T.
- the T-rich immunostimulatory nucleic acid comprises a nucleotide composition of greater than 25 % T, greater than 30% T, greater than 40% T, greater than 50% T, greater than 60% T, greater than 80% T, or greater than 90% T nucleotide residues.
- the poly-G nucleic acid comprises: 5' X ⁇ X 2 GGGX 3 3' wherein Xj, X 2 , X 3 , and X are nucleotides. In embodiments at least one of X and are a G or both of X and are a G. In other embodiments the poly-G nucleic acid comprises the following formula: 5' GGGNGGG 3' wherein N represents between 0 and 20 nucleotides. In yet other embodiments the poly-G nucleic acid comprises the following formula: 5' GGGNGGGNGGG 3' wherein N represents between 0 and 20 nucleotides.
- the poly-G immunostimulatory nucleic acid may include one or more CpG motifs or T-rich motifs. In other embodiments the poly-G nucleic acid is free of one or more CpG dinucleotides or poly-T motifs.
- FIG. 1 depicts data from flow cytometry which demonstrates the induction of a morphologic change in marginal zone lymphoma cells upon CpG oligonucleotide stimulation.
- Malignant B cells from a patient with marginal zone lymphoma were stimulated with no oligonucleotide (A and D), control oligonucleotide (ODN 2017, SEQ ID NO: 168, B and E) or CpG oligonucleotide (ODN 2006, SEQ J_D NO: 729, C and F) and analyzed by flow cytometry.
- A, B, and C illustrate forward scatter (FSC; x-axis) vs. side scatter (SSC; y-axis).
- D, E and F illustrate CD 19 expression (x-axis) against FSC (y-axis).
- Figure 2 depicts data from flow cytometry which demonstrates the change in expression of surface antigens on marginal zone lymphoma cells upon CpG oligodoexynucleotide (ODN) treatment.
- ODN CpG oligodoexynucleotide
- Figure 3 is a set of bar graphs depicting changes in expression of surface antigens on primary cells representing different B-cell malignancies and cells of a benign follicular hyperplasia upon treatment with, from left to right in each panel: negative control, no oligonucleotide, control oligonucleotide (ODN 2017, SEQ JD NO: 168), or CpG oligonucleotide (ODN 2006, SEQ ID NO: 729). Each panel represents one experiment.
- Figure 4 is a set of graphs depicting the observation that the effect of CpG oligonucleotide on CD20 (top) and CD40 (bottom) is dependent on the baseline level of expression of CD20 and CD40.
- FIG. 5 depicts data from flow cytometry which demonstrates the effect of CpG oligonucleotide-induced proliferation of malignant and normal B cells.
- Peripheral blood mononuclear cells from patients with B-CLL (left) or marginal zone lymphoma with circulating malignant cells (right) were incubated with CpG oligonucleotide (bottom) or medium alone (top) and evaluated by two-color flow cytometry.
- CFSE fluorescence (x-axis) and expression of CD5 (B-CLL) or CD 19 (marginal zone lymphoma) (y-axis) were evaluated.
- Figure 6 is a graph depicting the survival of mice injected on Day 0 with tumor cells in response to CpG simulation in combmation with murine IgG2a and murine IgGl anti- tumor antibodies. Treatments are shown as filled squares, untreated controls; filled circles, murine IgGl ; filled triangles, murine IgGl plus CpG; filled diamonds, murine IgG2a; and open squares, murine IgG2a plus CpG.
- the invention provides methods and products for the more effective treatment of cancer using a combination of immunostimulatory nucleic acids, antibodies, and optionally cancer therapies.
- the invention is based, in part, on the surprising discovery that administration to a subject of immunostimulatory nucleic acids induces the expression of cell surface antigens including CD20, CD19, and CD22 on the surface of a cancer cell and that the induction of these antigens leads to enhanced antibody-dependent cellular cytotoxicity (ADCC). It was previously believed that CpG oligonucleotides enhanced ADCC by influencing the effector cell (e.g., by activating natural killer (NK) cells).
- NK natural killer
- the invention provides a method for treating or preventing cancer which involves the administration to a subject of a combination of an immunostimulatory nucleic acid and an antibody which specifically interacts with CD20, CD 19, and CD22 in an effective amount to prevent or treat the cancer.
- Immunostimulatory nucleic acids but not control nucleic acids, increased the expression of co-stimulatory molecules (e.g., CD40, CD80, CD86, CD54) on malignant B cells without altering the phenotype of B cells derived from reactive follicular hyperplasia.
- Immunostimulatory nucleic acids also enhanced expression of both class I and class II MHC in most samples.
- CD20 expression was increased in response to immunostimulatory nucleic acids, most notably in B-CLL and marginal zone lymphoma.
- the invention relates to methods for identifying an appropriate therapy for a lymphoma patient, and for treating the patient using that therapy.
- the method can be accomplished by isolating a B cell from a lymphoma patient and comparing the surface antigens expressed on the malignant B cell with those expressed on normal B cells.
- the antigens which are expressed in low levels or not at all on the malignant B cell can be identified.
- the subject can then be treated using a combination of an immunostimulating nucleic acid and an antibody which specifically recognizes the antigen(s) which are expressed in low levels or not at all on the malignant B cell.
- the invention is also useful for treating cancers which are resistant to monoclonal antibody therapy. It has been discovered according to the invention, that immunostimulatory nucleic acids can reverse the resistance of tumor cells and render tumor cells which were previously non-responsive or only weakly responsive, sensitive to therapy. In particular it has been discovered that immunostimulatory nucleic acids can cause a phenotypic change to a resistant tumor cell that renders it sensitive to monoclonal antibody therapy. For instance, the monoclonal anti-CD20 antibody Rituximab has been shown to be effective clinically in several trials and has recently been approved for the therapy of follicular B cell lymphoma.
- the immunostimulatory nucleic acids of the invention are useful for treating this set of resistant tumors. Additionally, Rituximab has not been useful for the treatment of all types of B cell malignancies. Expression of CD20 is relatively low on B-CLL cells, which provides an explanation for why Rituximab is less effective for CLL than for some other B-cell malignancies. Grinaldi L et a ⁇ ., JClin Pathol 51:364-9 (1998). The immunostimulatory nucleic acids of the invention are also useful for treating these tumors.
- the humanized monoclonal antibody 1D10 recognizes an HLA-DR variant antigen.
- This antibody is currently being tested in a phase I clinical trial in patients with lymphoma.
- the target antigen is only expressed by approximately 50% of B-cell lymphomas.
- its expression was upregulated by immunostimulatory nucleic acids in all lymphoma samples tested. It was discovered according to the invention that immunostimulatory nucleic acids may enhance the efficacy of therapy with these and other antibodies by increasing expression of target antigen.
- the invention includes methods for treating lymphoma by administering to a subject an immunostimulatory nucleic acid and antibodies specific for HLA-DR.
- One useful antibody is the humanized monoclonal antibody ID 10. It is particularly useful for treating resistant tumors.
- the invention also relates to the discovery of a specific subclass, or isotype, of antibody which when combined with immunostimulatory nucleic acids produces a synergistic immune response. Another subclass, or isotype, does not even provide an additive response when combined with immunostimulatory nucleic acids. It was discovered according to the invention that the combination of immunostimulatory nucleic acids and human antibodies of the IgGl isotype results in an increased (synergistic) survival rate.
- immunostimulatory nucleic acids When immunostimulatory nucleic acids are combined with human antibodies of the IgG2 isotype, no increase in survival rate is observed over the use of the IgG2 antibody alone.
- the IgG2 isotype (which correlates with the murine IgGl isotype) is believed to be recognized by the Fc receptor designated CD 16 that is expressed largely by NK cells.
- Immunostimulatory nucleic acids are known to activate NK cells, and thus, it is su ⁇ rising that immunostimulatory nucleic acids do not enhance the therapeutic effect of human IgG2 or murine IgGl antibodies.
- NK cells are believed to be involved in ADCC and are activated by immunostimulatory nucleic acids, it was surprising that antibodies of the human IgG2 (or murine IgGl) isotype do not produce a synergistic or even additive response when administered with immunostimulatory nucleic acids.
- a cancer cell is a cell that divides and reproduces abnormally due to a loss of normal growth control. Cancer cells almost always arise from at least one genetic mutation. In some instances, it is possible to distinguish cancer cells from their normal counte ⁇ arts based on profiles of expressed genes and proteins, as well as to the level of their expression. Genes commonly affected in cancer cells include oncogenes, such as ras, neu/HER2/erbB, myb, myc and abl, as well as tumor suppressor genes such as p53, Rb, DCC, RET and WT. Cancer-related mutations in some of these genes leads to a decrease in their expression or a complete deletion. In others, mutations cause an increase in expression or the expression of an activated variant of the normal counterpart.
- neoplasm is usually equated with neoplasm, which literally means “new growth” and is used interchangeably with “cancer.”
- a "neoplastic disorder” is any disorder associated with cell proliferation, specifically with a neoplasm.
- a “neoplasm” is an abnormal mass of tissue that persists and proliferates after withdrawal of the carcinogenic factor that initiated its appearance.
- the method of the invention can be used to treat neoplastic disorders in humans, including but not limited to: sarcoma, carcinoma, fibroma, glioma, leukemia, lymphoma, melanoma, myeloma, neuroblastoma, retinoblastoma, and rhabdomyosarcoma, as well as each of the other tumors described herein.
- sarcoma as used herein refers to an uncontrolled growth of cells which interferes with the normal functioning of the bodily organs and systems. Cancers which migrate from their original location and seed vital organs can eventually lead to the death of the subject through the functional deterioration of the affected organs.
- Hemopoietic cancers such as leukemia, are able to out-compete the normal hemopoietic compartments in a subject, thereby leading to hemopoietic failure (in the form of anemia, thrombocytopenia and neutropenia), ultimately causing death.
- a metastasis is a region of cancer cells, distinct from the primary tumor location, resulting from the dissemination of cancer cells from the primary tumor to other parts of the body.
- the subject may be monitored for the presence of metastases. Metastases are most often detected through the sole or combined use of magnetic resonance imaging (MRI) scans, computed tomography (CT) scans, blood and platelet counts, liver function studies, chest X-rays and bone scans in addition to the monitoring of specific symptoms.
- MRI magnetic resonance imaging
- CT computed tomography
- Cancers include, but are not limited to, basal cell carcinoma, biliary tract cancer; bladder cancer; bone cancer; brain and CNS cancer; breast cancer; cervical cancer; choriocarcinoma; colon and rectum cancer; connective tissue cancer; cancer of the digestive system; endometrial cancer; esophageal cancer; eye cancer; cancer of the head and neck; gastric cancer; infra-epithelial neoplasm; kidney cancer; larynx cancer; leukemia; liver cancer; lung cancer (e.g., small cell and non-small cell); lymphoma including Hodgkin's and non-Hodgkin's lymphoma; melanoma; myeloma; neuroblastoma; oral cavity cancer (e.g., lip, tongue, mouth, and pharynx); ovarian cancer; pancreatic cancer; prostate cancer; retinoblastoma; rhabdomyosarcoma; rectal cancer; renal cancer; cancer of the respiratory system;
- the immunostimulatory nucleic acids and antibodies are useful for treating or preventing cancer in a subject.
- a "subject” unless otherwise specified shall mean a human or vertebrate mammal including but not limited to a dog, cat, horse, cow, pig, sheep, goat, or primate, e.g., monkey.
- the invention can be used to treat cancer and tumors in human and non human subjects.
- Cancer is one of the leading causes of death in companion animals (i.e., cats and dogs). Cancer usually strikes older animals which, in the case of house pets, have become integrated into the family. Forty-five percent of dogs older than 10 years of age are likely to succumb to the disease. The most common treatment options include surgery, chemotherapy and radiation therapy.
- treatment modalities which have been used with some success are laser therapy, cryotherapy, hyperthermia and immunotherapy.
- the choice of treatment depends on the type of cancer and degree of dissemination. Unless the malignant growth is confined to a discrete area in the body, it is difficult to remove only malignant tissue without also affecting normal cells.
- Malignant disorders commonly diagnosed in dogs and cats include but are not limited to lymphosarcoma, osteosarcoma, mammary tumors, mastocytoma, brain tumor, melanoma, adenosquamous carcinoma, carcinoid lung tumor, bronchial gland tumor, bronchiolar adenocarcinoma, fibroma, myxochondroma, pulmonary sarcoma, neurosarcoma, osteoma, papilloma, retinoblastoma, Ewing's sarcoma, Wilnis' tumor, Burkitt's lymphoma, microglioma, neuroblastoma, osteoclastoma, oral neoplasia, fibrosarcoma, osteosarcoma and rhabdomyosarcoma.
- neoplasias in dogs include genital squamous cell carcinoma, transmissable venereal tumor, testicular tumor, seminoma, Sertoli cell tumor, hemangiopericytoma, histiocytoma, chloroma (granulocytic sarcoma), corneal papilloma, corneal squamous cell carcinoma, hemangiosarcoma, pleural mesothelioma, basal cell tumor, thymoma, stomach tumor, adrenal gland carcinoma, oral papillomatosis, hemangioendothelioma and cystadenoma.
- Additional malignancies diagnosed in cats include follicular lymphoma, intestinal lymphosarcoma, fibrosarcoma and pulmonary squamous cell carcinoma.
- the ferret an ever-more popular house pet, is known to develop insulinoma, lymphoma, sarcoma, neuroma, pancreatic islet cell tumor, gastric MALT lymphoma and gastric adenocarcinoma.
- Neoplasias affecting agricultural livestock include leukemia, hemangiopericytoma and bovine ocular neoplasia (in cattle); preputial fibrosarcoma, ulcerative squamous cell carcinoma, preputial carcinoma, connective tissue neoplasia and mastocytoma (in horses); hepatocellular carcinoma (in swine); lymphoma and pulmonary adenomatosis (in sheep); pulmonary sarcoma, lymphoma, Rous sarcoma, reticuloendotheliosis, fibrosarcoma, nephroblastoma, B-cell lymphoma and lymphoid leukosis (in avian species); retinoblastoma, hepatic neoplasia, lymphosarcoma (lymphoblastic lymphoma), plasmacytoid leukemia and swimbladder sarcoma (in fish), caseous lymphadenitis (C
- a method for treating cancer involves administering the compositions of the invention to a subject having cancer.
- a "subject having cancer” is a subject that has been diagnosed with a cancer.
- the subject has a cancer type characterized by a solid mass tumor.
- the solid tumor mass if present, may be a primary tumor mass.
- a primary tumor mass refers to a growth of cancer cells in a tissue resulting from the transformation of a normal cell of that tissue. In most cases, the primary tumor mass is identified by the presence of a cyst, which can be found through visual inspection or palpation methods, or by irregularity in shape, texture or weight of the tissue.
- the invention is aimed at administering the compositions of the invention to a subject at risk of developing cancer.
- a subject at risk of developing a cancer is one who has a high probability of developing cancer. These subjects include, for instance, subjects having a genetic abnormality, the presence of which has been demonstrated to have a correlative relation to a higher likelihood of developing a cancer.
- Subjects exposed to cancer-causing agents such as tobacco, asbestos, or other chemical toxins are also subjects at risk of developing cancers used herein.
- an immunostimulatory nucleic acid, an antibody and optionally a cancer therapy on a regular basis, such as monthly, the cancer growth will be prevented from initiating.
- This aspect of the invention is particularly advantageous when the subjects employed in certain trades which are exposed to cancer- causing agents on an ongoing basis. For example, many airborne, or inhaled, carcinogens such as tobacco smoke and asbestos have been associated with lung cancer.
- a carcinogen is an agent capable of initiating development of malignant cancers. Exposure to carcinogens generally increases the risk of neoplasms in subjects, usually by affecting DNA directly. Carcinogens may take one of several forms such as chemical, electromagnetic radiation, or may be an inert solid body. Substances for which there is sufficient evidence to establish a causal relationship in cancer in humans are referred to as confirmed human carcinogens.
- Aflatoxins include Alcoholic beverages, Aluminium production, 4- aminobiphenyl, Arsenic and arsenic compounds, Asbestos, Manufacture of auramine, Azathioprine, Benzene, Benzidine, Beryllium and beryllium compounds, Betel quid with tobacco, Bis(chloromethyl)ether and chloromethyl methyl ether (technical grade), Boot and shoe manufacture and repair (occupational exposure), 1,4 Butanediol dimethanesulphonate (Myleran), Cadmium and cadmium compounds, Chlorambucil, Chlornaphazine, l-(2- Chloroethyl)-3-(4-methylcyclohexyl)-l nitrosourea, Chloromethyl methyl ether (technical), Chromium compounds (hexavalent), Coal gasification, Coal tar pitches, Coal tars, Coke production, Cyclophosphamide,
- Substances for which there is a lesser degree of evidence in humans but sufficient evidence in animal studies, or degrees of evidence considered unequivocal of mutagenicity in mammalian cells, are referred to as probable human carcinogens.
- This category of substances includes: Acrylamide, Acrylonitrile, Adriamycin, Anabolic steroids, Azacitidine, Benzanthracene, Benzidine-based dyes (technical grade), Direct Black 38, Direct Blue 6, Direct Brown 95, Benzopyrenel,3-Butadiene, Captafol, Bischloroethyl nitrosourea (BCNU), 1 -(2-Chloroethyl)-3-cyclohexyl-l -nitrosourea (CCNU), Chloramphenicolpara-Chloro-ortho- toluidine and its strong acid salts, Chlorozotocin, Cisplatin, Creosotes, Dibenzanthracene, Diesel engine exhaust, Diethy
- Substances for which there is sufficient evidence in animal tests are referred to as possible human carcinogens.
- This category of substances includes: A-C(2-Amino-9H- pyrido[2,3-b]indole), Acetaldehyde, Acetamide, AF-2[2-(2-Furyl)-3-(5-nitro-2- furyl)acrylamide, para-Aminoazobenzene, ortho-Aminoazobenzene, 2-Amino-5-(5-nitro-2- furyl)-l,3,4-thiadiazole, Amitrole, ortho-Anisidine, Antimony trioxide, Aramite, Atrazine, Attapulgite, Azaserine, Benzo[b]fluoranthene, Benzo[j]fluoranthene, Benzo[k]fluoranthene, Benzyl violet, Bitumens (extracts of steam-refined and air-refined bitumens), Bleomycins, Bra
- Diaminodiphenyl ether 2,4-Diaminotoluene, Dibenz[a,h]acridine, Dibenz[a,j]acridine, 7H- Dibenzo[c,g]carbazole, Dibenzo[a,e]pyrene, Dibenzo[a,h]pyrene, Dibenzo[a,i]pyrene, Dibenzo[a,l]pyrene, l,2-Dibromo-3-chloropropane, para-Dichlorobenzene, 3,3'- Dichlorobenzene, 3,3'-Dichloro-4,4'-diaminodiphenyl ether, 1,2-Dichloroethane, Dichloromethane, 1,3-Dichloropropene (technical grade), Dichlorvos, Diepoxybutane, Diesel fuel (marine), Di(2-ethylhexyl)phthalate, 1,2-Diethylhydrazine, Diglycidyl
- Phenoxybenzamine hydrochloride Phenyl glycidyl ether, PhenytoinPhJJP (2 -Amino- 1- methyl-6-phenylimidazo[4,5-b]pyridine, Pickled vegetables, traditional Asian, Polybrominated biphenyls, Ponceau MXPonceau 3R, Potassium bromate, 1,3 -Propane sultone, Propylene oxide, Progestins, Medroxyprogesterone acetate, a-Propiolactone, Propylthiouracil, Rockwool, Saccharin, Safrole, Slagwool, Sodium ortho-phenylphenate,
- Subjects at risk of developing cancer also include those who have a genetic predisposition to cancer.
- genetic predisposition to cancer can be identified by studying the occurrence of cancer in family members.
- Examples of genetic predisposition to common forms of cancer include, but are not limited to, mutation of BRCA1 and BRCA2 in familial breast cancer, mutation of APC in familial colony cancer (familial polyposis coli), mutation of MSH2 and MLH1 in hereditary nonpolyposis colon cancer (HNPCC), mutation of p53 in Li-Fraumeni syndrome, mutation of Rbl in retinoblastoma, mutation of RET in multiple endocrine neoplasia type 2 (MEN2), mutation of VHL in renal cancer and mutation of WT1 in Wilms' tumor.
- Other cancers for which a familial predisposition has been identified include ovarian, prostate, melanoma and lung cancer.
- cancer medicaments It has been estimated that almost half of all currently diagnosed cancers will be treated with some form of cancer medicament.
- many forms of cancer including melanoma, colorectal, prostate, endometrial, cervical and bladder cancer, do not respond well to treatment with cancer medicaments.
- cancer medicaments only about 5-10 percent of cancers can be cured using cancer medicaments alone. These include some forms of leukemias and lymphomas, testicular cancer, choriocarcinoma, Wilms' tumor, Ewing's sarcoma, neuroblastoma, small-cell lung cancer and ovarian cancer.
- Treatment of still other cancers, including breast cancer requires a combination therapy of surgery or radiotherapy in conjunction with a cancer medicament.
- the immunostimulatory nucleic acids are administered in combination with antibodies which specifically bind to cancer cell surface antigens.
- antibodies include but are not limited to anti-CD20 antibodies, anti-CD40 antibodies, anti-CD 19 antibodies, anti-CD22 antibodies, anti-HLA-DR antibodies, anti-CD80 antibodies, anti-CD86 antibodies, anti-CD54 antibodies, and anti-CD69 antibodies. These antibodies are available from commercial sources or may be synthesized de novo.
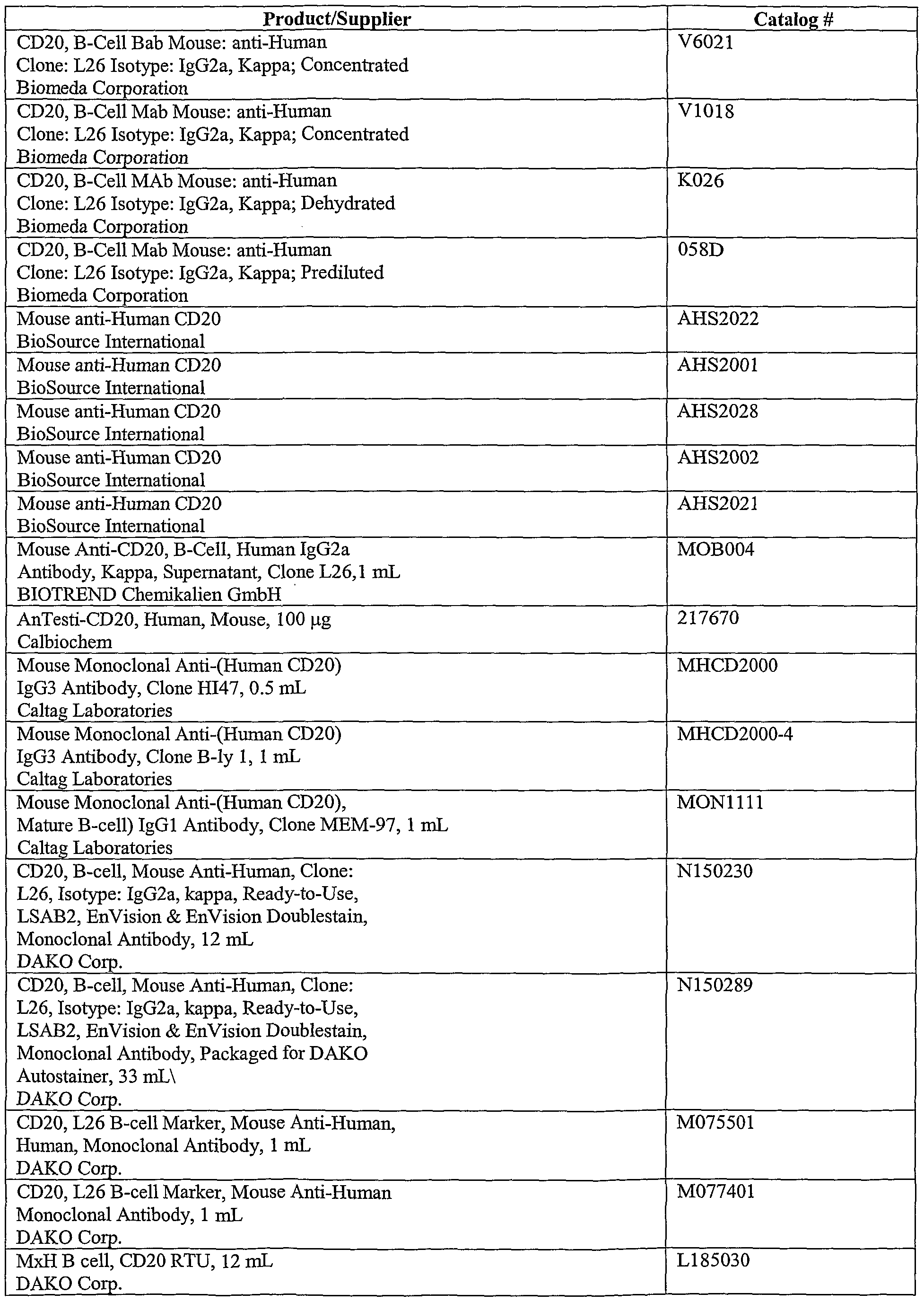
- anti-CD20 antibodies include but are not limited to those presented in Table 1 below.
- Antibodies are well known to those of ordinary skill in the science of immunology.
- the term “antibody” means not only intact antibody molecules but also fragments of antibody molecules retaining specific binding ability. Such fragments are also well known in the art and are regularly employed both in vitro and in vivo.
- the term “antibody” means not only intact immunoglobulin molecules but also the well-known active fragments F(ab') , and Fab. F(ab') 2 , and Fab fragments which lack the Fc fragment of intact antibody, clear more rapidly from the circulation, and may have less non-specific tissue binding of an intact antibody. Wahl RL et al., JNucl Med 24:316-25 (1983).
- Antibody fragments which are particularly useful according to the methods of the invention are those which are bispecific and constructed to enhance FcR binding, e.g., include an Fc portion. These include, but are not limited to Medarex antibodies (MDX-210, 220, 22, 447, and 260). Other non-Fc containing fragments which interact with the antigens induced on the cell surface are also useful. These are particularly useful in combination with immunotoxins and/or radioactivity. The fragments can be delivered separately from the immunotoxins or radioactivity or conjugated thereto (e.g., radiolabled antibodies or antibody fragments).
- CDRs complementarity-determining regions
- FRs framework regions
- CDR1 through CDR3 complementarity-determining regions
- a "humanized monoclonal antibody” as used herein is a human monoclonal antibody or functionally active fragment thereof having human constant regions and a binding CDR3 region from a mammal of a species other than a human.
- Humanized monoclonal antibodies may be made by any method known in the art. Humanized monoclonal antibodies, for example, may be constructed by replacing the non-CDR regions of a non-human mammalian antibody with similar regions of human antibodies while retaining the epitopic specificity of the original antibody. For example, non-human CDRs and optionally some of the framework regions may be covalently joined to human FR and/or Fc/pFc' regions to produce a functional antibody.
- European Patent Application 0239400 provides an exemplary teaching of the production and use of humanized monoclonal antibodies in which at least the CDR portion of a murine (or other non-human mammal) antibody is included in the humanized antibody. Briefly, the following methods are useful for constructing a humanized CDR monoclonal antibody including at least a portion of a mouse CDR.
- a first replicable expression vector including a suitable promoter operably linked to a DNA sequence encoding at least a variable domain of an Ig heavy or light chain and the variable domain comprising framework regions from a human antibody and a CDR region of a murine antibody is prepared.
- a second replicable expression vector which includes a suitable promoter operably linked to a DNA sequence encoding at least the variable domain of a complementary human Ig light or heavy chain respectively.
- a cell line is then transformed with the vectors.
- the cell line is an immortalized mammalian cell line of lymphoid origin, such as a myeloma, hybridoma, trioma, or quadroma cell line, or is a normal lymphoid cell which has been immortalized by transformation with a virus.
- the transformed cell line is then cultured under conditions known to those of skill in the art to produce the humanized antibody.
- several techniques are well known in the art for creating the particular antibody domains to be inserted into the replicable vector.
- the DNA sequence encoding the domain may be prepared by oligonucleotide synthesis.
- Another method involves the preparation of the DNA sequence encoding the variable CDR containing domain by oligonucleotide site- directed mutagenesis. Each of these methods is well known in the art. Therefore, those skilled in the art may construct humanized antibodies containing a murine CDR region without destroying the specificity of the antibody for its epitope.
- Human monoclonal antibodies may be made by any of the methods known in the art, such as those disclosed in U.S. Patent No. 5,567,610, issued to Borrebaeck et al., U.S. Patent No. 5,565,354, issued to Ostberg, U.S. Patent No. 5,571,893, issued to Baker et al, Kozbor D et al., J Immunol 133:3001-5 (1984), Brodeur et al., Monoclonal Antibody Production
- Such antibodies may also be prepared by immunizing transgenic animals that are capable of producing human antibodies (e.g., Jakobovits A et al., Proc Natl Acad Sci USA 90:2551-5 (1993); Jakobovits A et al., N ⁇ twre 362:255-8 (1993); Bruggermann et al., Year in Immunology 7:33 (1993); and U.S. Patent No. 5,569,825 issued to Lonberg).
- Jakobovits A et al. Proc Natl Acad Sci USA 90:2551-5 (1993); Jakobovits A et al., N ⁇ twre 362:255-8 (1993); Bruggermann et al., Year in Immunology 7:33 (1993); and U.S. Patent No. 5,569,825 issued to Lonberg).
- an antibody from which the pFc' region has been enzymatically cleaved, or which has been produced without the pFc' region designated an F(ab') 2 fragment
- an antibody from which the Fc region has been enzymatically cleaved, or which has been produced without the Fc region designated an Fab fragment
- Fab fragments consist of a covalently bound antibody light chain and a portion of the antibody heavy chain denoted Fd.
- the Fd fragments are the major determinant of antibody specificity (a single Fd fragment may be associated with up to ten different light chains without altering antibody specificity) and Fd fragments retain epitope-binding ability in isolation.
- antibodies useful according to the invention are antibodies of the IgGl isotype.
- anti-IgGl isotype antibody as used herein refers to a human or humanized anti-IgGl unless otherwise specified.
- IgGl isotype antibodies are well known in the art and include at least the antibodies listed in Table 2 below.
- the nucleic acid and antibody are administered in combination with a cancer therapy.
- a cancer therapy refers to an agent which prevents growth of a cancer cell by decreasing or slowing the rate of growth, by inhibiting growth altogether, or by killing or inducing apoptosis of the cancer cell.
- treating cancer includes preventing the development of a cancer, reducing the symptoms of cancer, and/or inhibiting the growth of an established cancer.
- the cancer therapy is administered to a subject at risk of developing a cancer for the pu ⁇ ose of reducing the risk of developing the cancer.
- chemotherapeutic agents are classified as chemotherapeutic agents, cancer vaccines, hormone therapy, biological response modifiers, surgical procedures, and radiotherapy aimed at treating cancer.
- the methods of the invention are intended to embrace the use of more than one cancer therapy along with the immunostimulatory nucleic acids and antibody.
- the immunostimulatory nucleic acids may be administered with a both a chemotherapeutic agent and a radiotherapy.
- Cancer therapies function in a variety of ways. Some cancer therapies work by targeting physiological mechanisms that are specific to tumor cells. Examples include the targeting of specific genes and their gene products (i.e., proteins primarily) which are mutated in cancers. Such genes include but are not limited to oncogenes (e.g., Ras, Her2, bcl-2), tumor suppressor genes (e.g., EGF, p53, Rb), and cell cycle targets (e.g., CDK4, p21, telomerase). Cancer therapies can alternately target signal transduction pathways and molecular mechanisms which are altered in cancer cells.
- oncogenes e.g., Ras, Her2, bcl-2
- tumor suppressor genes e.g., EGF, p53, Rb
- cell cycle targets e.g., CDK4, p21, telomerase.
- cancer therapies target cells other than cancer cells.
- some medicaments prime the immune system to attack tumor cells (i.e., cancer vaccines).
- Still other medicaments called angiogenesis inhibitors, function by attacking the blood supply of solid tumors. Since the most malignant cancers are able to metastasize (i.e., exit the primary tumor site and seed a distal tissue, thereby forming a secondary tumor), medicaments that impede this metastasis are also useful in the treatment of cancer.
- Angiogenic mediators include basic FGF, VEGF, angiopoietins, angiostatin, endostatin, TNF- ⁇ , TNP-470, thrombospondin-1, platelet factor 4, CAI, and certain members of the integrin family of proteins.
- a metalloproteinase inhibitor which inhibits the enzymes used by the cancer cells to exit the primary tumor site and extravasate into another tissue.
- chemotherapeutic agents encompass both chemical and biological agents. These agents function to inhibit a cellular activity which the cancer cell is dependent upon for continued survival. Categories of chemotherapeutic agents include alkylating/alkaloid agents, antimetabolites, hormones or hormone analogs, and miscellaneous antineoplastic drugs. Most ifnot all of these agents are directly toxic to cancer cells and do not require immune stimulation. Chemotherapeutic agents which are currently in development or in use in a clinical setting are shown in Table 3 below.
- Interferon- ⁇ e.g., INTRON® A, Schering.
- nucleic acids may be double-stranded or single-stranded. Generally, double-stranded molecules may be more stable in vivo, while single-stranded molecules may have increased activity.
- nucleic acid and oligonucleotide refer to multiple nucleotides (i.e., molecules comprising a sugar (e.g., ribose or deoxyribose) linked to a phosphate group and to an exchangeable organic base, which is either a substituted pyrimidine (e.g., cytosine (C), thymine (T) or uracil (U)) or a substituted purine (e.g., adenine (A) or guanine (G)) or a modified base.
- a substituted pyrimidine e.g., cytosine (C), thymine (T) or uracil (U)
- purine e.g., adenine (A) or guanine (
- nucleic acid and oligonucleotide also encompass nucleic acids or oligonucleotides with a covalently modified base and/or sugar. For example, they include nucleic acids having backbone sugars which are covalently attached to low molecular weight organic groups other than a hydroxyl group at the 3' position and other than a phosphate group at the 5' position.
- modified nucleic acids may include a 2'-O-alkylated ribose group.
- modified nucleic acids may include sugars such as arabinose instead of ribose.
- the nucleic acids may be heterogeneous in backbone composition thereby containing any possible combination of polymer units linked together such as peptide-nucleic acids (which have amino acid backbone with nucleic acid bases).
- the nucleic acids are homogeneous in backbone composition.
- Nucleic acids also can include base analogs such as C-5 propyne modified bases.
- Purines and pyrimidines include but are not limited to adenine, cytosine, guanine, thymine, 5-methylcytosine, 2-aminopurine, 2-amino-6-chloropurine, 2,6-diaminopurine, hypoxanthine, and other naturally and non-naturally occurring nucleobases, substituted and unsubstituted aromatic moieties.
- the nucleic acid is a linked polymer of bases or nucleotides. As used herein with respect to linked units of a nucleic acid, "linked" or “linkage” means two entities are bound to one another by any physicochemical means.
- linkages Any linkage known to those of ordinary skill in the art, covalent or non-covalent, is embraced. Such linkages are well known to those of ordinary skill in the art. Natural linkages, which are those ordinarily found in nature connecting the individual units of a nucleic acid , are most common. The individual units of a nucleic acid may be linked, however, by synthetic or modified linkages.
- nucleic acid is represented by a sequence of letters it will be understood that the nucleotides are in 5' ⁇ 3' order from left to right and that "A” denotes adenosine, “C” denotes cytosine, “G” denotes guanosine, “T” denotes thymidine, and “U” denotes uracil unless otherwise noted.
- Nucleic acid molecules useful according to the invention can be obtained from natural nucleic acid sources (e.g., genomic nuclear or mitochondrial DNA or cDNA), or are synthetic (e.g., produced by oligonucleotide synthesis). Nucleic acids isolated from existing nucleic acid sources are referred to herein as native, natural, or isolated nucleic acids.
- the nucleic acids useful according to the invention may be isolated from any source, including eukaryotic sources, prokaryotic sources, nuclear DNA, mitochondrial DNA, etc. Thus, the term nucleic acid encompasses both synthetic and isolated nucleic acids.
- isolated refers to a nucleic acid which is substantially free of other nucleic acids, proteins, lipids, carbohydrates or other materials with which it is naturally associated.
- the nucleic acids can be produced on a large scale in plasmids, (see Sambrook T et al., "Molecular Cloning: A Laboratory Manual", Cold Spring Harbor Laboratory Press, New York, 1989) and separated into smaller pieces or administered whole. After being administered to a subject the plasmid can be degraded into oligonucleotides.
- One skilled in the art can purify viral, bacterial, eukaryotic, etc., nucleic acids using standard techniques, such as those employing restriction enzymes, exonucleases or endonucleases.
- the nucleic acids can be synthesized de novo using any of a number of procedures well known in the art.
- the b-cyanoethyl phosphoramidite method (Beaucage SL et al., Tetrahedron Lett 22:1859, 1981); nucleoside H-phosphonate method (Garegg et al., Tetrahedron Lett 27:4051-4, 1986; Froehler et al., Nucl Acid Res 14:5399-407, 1986; Garegg et al., Tetrahedron Lett 27:4055-8, 1986; Gaffhey et al., Tetrahedron Lett 29:2619-22, 1988).
- These chemistries can be performed by a variety of automated oligonucleotide synthesizers available in the market.
- the nucleic acids useful according to the invention are immunostimulatory nucleic acids.
- An immunostimulatory nucleic acid is any nucleic acid, as described above, which is capable of modulating an immune response.
- a nucleic acid which modulates an immune response is one which produces any form of immune stimulation, including, but not limited to, induction of cytokines, B-cell activation, T-cell activation, monocyte activation.
- Immunostimulatory nucleic acids include, but are not limited to, CpG nucleic acids, methylated CpG nucleic acids, T-rich nucleic acids, poly-G nucleic acids, and nucleic acids having phosphate modified backbones, such as phosphorothioate backbones.
- CpG nucleic acid or a “CpG immunostimulatory nucleic acid” as used herein is a nucleic acid containing at least one unmethylated CpG dinucleotide (cytosine-guanine dinucleotide sequence, i.e., "CpG DNA” or DNA containing a 5' cytosine followed by 3' guanosine and linked by a phosphate bond) and activates a component of the immune system.
- the entire CpG nucleic acid can be unmethylated or portions may be unmethylated but at least the C of the 5' CG 3' must be unmethylated.
- the invention provides a CpG nucleic acid represented by at least the formula:
- Xi and X 2 are nucleotides and N is any nucleotide and Ni and N 2 are nucleic acid sequences composed of from about 0-25 N's each.
- Xi is adenine, guanine, or thymine and X 2 is cytosine, adenine, or thymine.
- Xi is cytosine and/or X 2 is guanine.
- the CpG nucleic acid is represented by at least the formula: 5' N ⁇ X ⁇ X 2 CGX 3 X 4 N 2 3' wherein Xi, X 2 , X 3 , and X 4 are nucleotides.
- X ⁇ X 2 are nucleotides selected from the group consisting of: GpT, GpG, GpA, ApA, ApT, ApG, CpT, CpA, CpG, TpA, TpT, and TpG; and X - are nucleotides selected from the group consisting of: TpT, CpT, ApT, TpG, ApG, CpG, TpC, ApC, CpC, TpA, ApA, and CpA; N is any nucleotide and Ni and N 2 are nucleic acid sequences composed of from about 0-25 N's each.
- X ⁇ X 2 are GpA or GpT and X 3 X 4 are TpT.
- Xi or X 2 or both are purines and X or X-j or both are pyrimidines or X ⁇ X are GpA and X 3 or X or both are pyrimidines.
- Ni and N 2 of the nucleic acid do not contain a CCGG or CGCG quadmer or more than one CCG or CGG trimer. The effect of a CCGG or CGCG quadmer or more than one CCG or CGG trimer depends in part on the status of the nucleic acid backbone.
- the nucleic acid has a phosphodiester backbone or a chimeric backbone the inclusion of these sequences in the nucleic acid will only have minimal if any affect on the biological activity of the nucleic acid. If the backbone is completely phosphorothioate or significantly phosphorothioate then the inclusion of these sequences may have more influence on the biological activity or the kinetics of the biological activity, but compounds containing these sequences are still useful.
- the CpG nucleic acid has the sequence 5' TCN ⁇ TX ⁇ X 2 CGX X 4 3'.
- T-rich nucleic acid or “T-rich immunostimulatory nucleic acid” is a nucleic acid which includes at least one poly-T sequence and/or which has a nucleotide composition of greater than 25% T nucleotide residues and which activates a component of the immune system.
- a nucleic acid having a poly-T sequence includes at least four Ts in a row, such as 5' TTTT 3'.
- the T-rich nucleic acid includes more than one poly-T sequence, hi preferred embodiments the T-rich nucleic acid may have 2, 3, 4, etc., poly-T sequences, such as oligonucleotide #2006 (5' TCGTCGTTTTGTCGTTTTGTCGTT 3', SEQ ID NO: 729).
- oligonucleotide #2006 5' TCGTCGTTTTGTCGTTTTGTCGTT 3', SEQ ID NO: 729.
- One of the most highly immunostimulatory T-rich oligonucleotides discovered according to the invention is a nucleic acid composed entirely of T nucleotide residues, e.g., oligonucleotide #2183 (5* ⁇ 3 ⁇ SE Q j ) N0: 841).
- T-rich nucleic acids have a nucleotide composition of greater than 25% T nucleotide residues, but do not necessarily include a poly-T sequence.
- the T nucleotide resides may be separated from one another by other types of nucleotide residues, i.e., G, C, and A.
- the T-rich nucleic acids have a nucleotide composition of greater than 30%, 40%, 50%, 60%, 70%, 80%, 90%, and 99%, T nucleotide residues and every integer % in between.
- the T-rich nucleic acids have at least one poly-T sequence and a nucleotide composition of greater than 25% T nucleotide residues.
- the T-rich nucleic acid is represented by at least the formula:
- X ⁇ X is TT and or X 3 X 4 is TT.
- X ⁇ X 2 are any one of the following nucleotides TA, TG, TC, AT, AA, AG, AC, CT, CC, CA, CG, GT, GG, GA, and GC; and X 3 X 4 are any one of the following nucleotides TA, TG, TC, AT, AA, AG, AC, CT, CC, CA, CG, GT, GG, GA, and GC.
- the T-rich nucleic acid does not contain poly-C (CCCC), poly-A (AAAA), poly-G (GGGG), CpG motifs, or multiple GGs. In other embodiments the T-rich nucleic acid includes these motifs.
- the T-rich nucleic acids include CpG dmucleotides and in other embodiments the T-rich nucleic acids are free of CpG dmucleotides. The CpG dmucleotides maybe methylated or unmethylated.
- Poly-G containing nucleic acids are also immunostimulatory.
- references including Pisetsky DS et al., Mol Biol Rep 18:217-21 (1993); Krieger M et al., Annu Rev Biochem 63:601-37 (1994); Macaya RF et al., Proc Natl Acad Sci USA 90:3745-9 (1993); Wyatt JR et al., Proc Natl Acad Sci USA 91:1356-60 (1994); Rando and Hogan, 1998, In: Applied Antisense Oligonucleotide Technology, eds. Krieg AM and Stein C, pp.
- Poly G nucleic acids preferably are nucleic acids having the following formulas:
- the poly-G nucleic acid is free of unmethylated CG dmucleotides, such as, for example, the nucleic acids listed in Table 4 below as SEQ ID NOs: 12-14, 23, 56, 100, 155, 163, 182, 227, 237, 246, 400, 407, 429, 430, 432, 435, 438, 439, 446, 450, 451, 480, 487, 493, 522, 661, 662, 671-673, 807, 808, 821, 823, and 834.
- the poly-G nucleic acid includes at least one unmethylated CG dinucleotide, such as, for example, the nucleic acids listed in Table 4 below as SEQ ID NOs: 6, 7, 22, 26, 28-30, 87, 115, 141, 177, 191, 209, 254, 258, 267, 303, 317, 329, 335, 344, 345, 395, 414, 417, 418, 423-426, 428, 431, 433, 434, 436, 437, 440, 442-445, 447-449, 458, 460, 463, 467-469, 474, 515, 516, 594, 638-640, 663, 664, 727, 752, 776, 795, 799, 817, 818, 831, and 832.
- SEQ ID NOs: 6, 7, 22, 26, 28-30 87, 115, 141, 177, 191, 209, 254, 258, 267, 303, 317, 329, 335,
- Nucleic acids having modified backbones such as phosphorothioate backbones, also fall within the class of immunostimulatory nucleic acids.
- U.S. Patents Nos. 5,723,335 and 5,663,153 issued to Hutcherson, et al. and related PCT publication WO95/26204 describe immune stimulation using phosphorothioate oligonucleotide analogues. These patents describe the ability of the phosphorothioate backbone to stimulate an immune response in a non-sequence specific manner.
- the immunostimulatory nucleic acids may be any size but in some embodiments are in the range of between 6 and 100 or in some embodiments between 8 and 35 nucleotides in size, hnmunostimulatory nucleic acids can be produced on a large scale in plasmids. These may be administered in plasmid form or alternatively they can be degraded into oligonucleotides.
- “Palindromic sequence” shall mean an inverted repeat (i.e., a sequence such as ABCDEE'D'C'B'A' in which A and A' are bases capable of forming the usual Watson-Crick base pairs and which includes at least 6 nucleotides in the palindrome. In vivo, such sequences may form double-stranded structures.
- the nucleic acid contains a palindromic sequence.
- a palindromic sequence used in this context refers to a palindrome in which the CpG is part of the palindrome, and optionally is the center of the palindrome. In another embodiment the nucleic acid is free of a palindrome.
- a nucleic acid that is free of a palindrome does not have any regions of 6 nucleotides or greater in length which are palindromic.
- a nucleic acid that is free of a palindrome can include a region of less than 6 nucleotides which are palindromic.
- a "stabilized nucleic acid molecule” shall mean a nucleic acid molecule that is relatively resistant to in vivo degradation (e.g., via an exonuclease or endonuclease). Stabilization can be a function of length or secondary structure. Nucleic acids that are tens to hundreds of kbs long are relatively resistant to in vivo degradation. For shorter nucleic acids, secondary structure can stabilize and increase their effect.
- an oligonucleotide For example, if the 3' end of an oligonucleotide has self-complementarity to an upstream region, so that it can fold back and form a sort of stem loop structure, then the oligonucleotide becomes stabilized and therefore exhibits more activity.
- Some stabilized oligonucleotides of the instant invention have a modified backbone. It has been demonstrated that modification of the oligonucleotide backbone provides enhanced activity of the nucleic acids when administered in vivo. Nucleic acids, including at least two phosphorothioate linkages at the 5' end of the oligonucleotide and multiple phosphorothioate linkages at the 3' end, preferably 5, may provide maximal activity and protect the oligonucleotide from degradation by intracellular exo- and endo-nucleases.
- modified oligonucleotides include phosphodiester modified oligonucleotide, combinations of phosphodiester and phosphorothioate oligonucleotide, methylphosphonate, methylphosphorothioate, phosphorodithioate, and combinations thereof.
- phosphodiester modified oligonucleotide combinations of phosphodiester and phosphorothioate oligonucleotide, methylphosphonate, methylphosphorothioate, phosphorodithioate, and combinations thereof.
- modified oligonucleotides may show more stimulatory activity due to enhanced nuclease resistance, increased cellular uptake, increased protein binding, and/or altered intracellular localization. Both phosphorothioate and phosphodiester nucleic acids are active in immune cells.
- oligonucleotides include: nonionic DNA analogs, such as alkyl- and aryl-phosphates (in which the charged phosphonate oxygen is replaced by an alkyl or aryl group), phosphodiester and alkylphosphotriesters, in which the charged oxygen moiety is alkylated. Oligonucleotides which contain diol, such as tetraethyleneglycol or hexaethyleneglycol, at either or both termini have also been shown to be substantially resistant to nuclease degradation.
- nucleic acids are preferably relatively resistant to degradation (e.g., via endonucleases and exonucleases). Secondary structures, such as stem loops, can stabilize nucleic acids against degradation. Alternatively, nucleic acid stabilization can be accomplished via phosphate backbone modifications. One type of stabilized nucleic acid has at least a partial phosphorothioate modified backbone. Phosphorothioates may be synthesized using automated techniques employing either phosphoramidate or H-phosphonate chemistries. Aryl- and alkyl-phosphonates can be made, e.g., as described in U.S. Patent No.
- 4,469,863; and alkylphosphotriesters in which the charged oxygen moiety is alkylated as described in U.S. Patent No. 5,023,243 and European Patent No. 092,574 can be prepared by automated solid phase synthesis using commercially available reagents. Methods for making other DNA backbone modifications and substitutions have been described. Uhlmann E et al., Chem Rev 90:544-84 (1990); Goodchild J, Bioconjugate Chem 1:165-87 (1990).
- the immunostimulatory nucleic acids having backbone modifications useful according to the invention in some embodiments are S- or R-chiral immunostimulatory nucleic acids.
- S chiral immunostimulatory nucleic acid as used herein is an immunostimulatory nucleic acid wherein at least two nucleotides have a backbone modification forming a chiral center and wherein a plurality of the chiral centers have S chirality.
- R chiral immunostimulatory nucleic acid as used herein is an immunostimulatory nucleic acid wherein at least two nucleotides have a backbone modification forming a chiral center and wherein a plurality of the chiral centers have R chirality.
- the backbone modification may be any type of modification that forms a chiral center.
- the modifications include but are not limited to phosphorothioate, methylphosphonate, methylphosphorothioate, phosphorodithioate, 2'-OMe and combinations thereof. In other embodiments they are non-chiral.
- a non-chiral nucleic acid is any nucleic acid which does not have at least two chiral centers.
- the chiral immunostimulatory nucleic acids must have at least two nucleotides within the nucleic acid that have a backbone modification. All or less than all of the nucleotides in the nucleic acid, however, may have a modified backbone. Of the nucleotides having a modified backbone (referred to as chiral centers), a plurality have a single chirality, S or R. A "plurality" as used herein refers to an amount greater than or equal to 75%. Thus, less than all of the chiral centers may have S or R chirality as long as a plurality of the chiral centers have S or R chirality.
- At least 75%, 80%, 85%, 90%, 95%, or 100% of the chiral centers have S or R chirality.
- at least 75%, 80%, 85%, 90%, 95%, or 100% of the nucleotides have backbone modifications.
- the S- and R- chiral immunostimulatory nucleic acids may be prepared by any method known in the art for producing chirally pure oligonucleotides.
- Stec et al. teach methods for producing stereopure phosphorothioate oligodeoxynucleotides using an oxathiaphospholane.
- the vector as used herein may be an empty vector or a vector carrying a gene which can be expressed.
- the vector In the case when the vector is carrying a gene the vector generally transports the gene to the target cells with reduced degradation relative to the extent of degradation that would result in the absence of the vector.
- the vector optionally includes gene expression sequences to enhance expression of the gene in target cells such as immune cells, but it is not required that the gene be expressed in the cell.
- vectors include, but are not limited to, plasmids, phagemids, viruses, other vehicles derived from viral or bacterial sources.
- Viral vectors are one type of vector and include, but are not limited to, nucleic acid sequences from the following viruses: retrovirus, such as Moloney murine leukemia virus, Harvey murine sarcoma virus, murine mammary tumor virus, and Rous sarcoma virus; adenovirus, adeno-associated virus; SN40-type viruses; polyoma viruses; Epstein-Barr viruses; papiUoma viruses; herpes virus; vaccinia virus; polio virus; and R ⁇ A virus such as a retrovirus.
- retrovirus such as Moloney murine leukemia virus, Harvey murine sarcoma virus, murine mammary tumor virus, and Rous sarcoma virus
- adenovirus adeno-associated virus
- SN40-type viruses polyoma viruses
- Epstein-Barr viruses papiUoma viruses
- herpes virus vaccinia virus
- polio virus polio virus
- Some viral vectors are based on non-cytopathic eukaryotic viruses in which non-essential genes have been replaced with a nucleic acid to be delivered.
- ⁇ on-cytopathic viruses include retroviruses, the life cycle of which involves reverse transcription of genomic viral R ⁇ A into D ⁇ A.
- Plasmid vectors have been extensively described in the art and are well-known to those of skill in the art. See e.g., Sambrook et al., "Molecular Cloning: A Laboratory Manual," Second Edition, Cold Spring Harbor Laboratory Press, 1989. h the last few years, plasmid vectors have been found to be particularly advantageous for delivering genes to cells in vivo because of their inability to replicate within and integrate into a host genome. Some plasmids, however, having a promoter compatible with the host cell, can express a peptide from a gene operatively encoded within the plasmid.
- Plasmids include pBR322, pUC18, pUC19, pcDNA3.1, pSV40, and pBlueScript. Other plasmids are well-known to those of ordinary skill in the art. Additionally, plasmids may be custom designed using restriction enzymes and ligation reactions to remove and add specific fragments of DNA.
- plasmids empty or gene-carrying
- Modified forms of bacteria such as Salmonella can be transfected with the plasmid and used as delivery vehicles.
- the bacterial delivery vehicles can be administered to a host subject orally or by other administration means.
- the bacteria deliver the plasmid to immune cells, e.g., dendritic cells, probably by passing through the gut barrier. High levels of immune protection have been established using this methodology.
- Such methods of delivery are useful for the aspects of the invention utilizing systemic delivery of nucleic acid.
- an immunostimulatory nucleic acid is intended to embrace the administration of one or more immunostimulatory nucleic acids which may or may not differ in terms of their profile, sequence, backbone modifications and biological effect.
- CpG nucleic acids and T-rich nucleic acids may be administered to a single subject along with an antibody and optionally a cancer therapy.
- a plurality of CpG nucleic acids which differ in nucleotide sequence may also be administered to a subject.
- the nucleic acids are delivered in effective amounts.
- the term "effective amount" of a immunostimulatory nucleic acid refers to the amount necessary or sufficient to realize a desired biologic effect.
- an effective amount of an immunostimulatory nucleic acid could be that amount necessary to cause activation of the immune system.
- an effective amount is that amount of an immunostimulatory nucleic acid and that amount of an antibody, which when combined or co-administered, results in the prevention or the treatment of the cancer.
- a synergistic effect is observed.
- a synergistic amount is that amount which produces an anti-cancer response that is greater than the sum of the individual effects of either the immunostimulatory nucleic acid and the antibody alone.
- a synergistic combination of an immunostimulatory nucleic acid and an antibody provides a biological effect which is greater than the combined biological effect which could have been achieved using each of the components (i.e., the nucleic acid and the antibody) separately.
- the biological effect may be the amelioration and or absolute elimination of symptoms resulting from the cancer.
- the biological effect is the complete abrogation of the cancer, as evidenced for example, by the absence of a tumor or a biopsy or blood smear which is free of cancer cells.
- the effective amount of immunostimulatory nucleic acid necessary to treat a cancer or in the reduction of the risk of developing a cancer may vary depending upon the sequence of the immunostimulatory nucleic acid, the backbone constituents of the nucleic acid, and the mode of delivery of the nucleic acid.
- the effective amount for any particular application can also vary depending on such factors as the cancer being treated, the particular immunostimulatory nucleic acid being administered (e.g., the nature, number or location of immunostimulatory motifs in the nucleic acid), the size of the subject, or the severity of the disease or condition.
- One of ordinary skill in the art can empirically determine the effective amount of a particular immunostimulatory nucleic acid and antibody combination without necessitating undue experimentation.
- an effective prophylactic or therapeutic treatment regimen can be planned which does not cause substantial toxicity and yet is entirely effective to treat the particular subject.
- Therapeutic doses of cancer therapies are well known in the field of medicine for the treatment of cancer. These dosages have been extensively described in references such as Remington's Pharmaceutical Sciences, 18th ed., 1990; as well as many other medical references relied upon by the medical profession as guidance for the treatment of cancer. Therapeutic dosages of immunostimulatory nucleic acids have also been described in the art and methods for identifying therapeutic dosages in subjects are described in more detail herein. Subject doses of the compounds described herein typically range from about 0.1 ⁇ g to
- mucosal or local doses range from about 10 ⁇ g to 5 mg per administration, and most typically from about 100 ⁇ g to 1 mg, with 2 - 4 administrations being spaced hours, days or weeks apart.
- immune stimulant doses range from 1 ⁇ g to 10 mg per administration, and most typically 10 ⁇ g to 1 mg, with daily or weekly administrations.
- Subject doses of the compounds described herein for parenteral delivery, wherein the compounds are delivered without another therapeutic agent are typically 5 to 10,000 times higher than the effective mucosal dose or for immune stimulant applications, and more typically 10 to 1,000 times higher, and most typically 20 to 100 times higher.
- parenteral doses for these purposes range from about 10 ⁇ g to 5 mg per administration, and most typically from about 100 ⁇ g to 1 mg, with 2 - 4 administrations being spaced hours, days or weeks apart. In some embodiments, however, parenteral doses for these purposes may be used in a range of 5 to 10,000 times higher than the typical doses described above.
- the therapeutically effective amount can be initially determined from animal models, e.g., the animal models described herein.
- a therapeutically effective dose can also be determined from human data for CpG nucleic acids which have been tested in humans (human clinical trials have been initiated and the results publicly disseminated) and for compounds which are known to exhibit similar pharmacological activities.
- Higher doses may be required for parenteral administration, as described above.
- the applied dose can be adjusted based on the relative bioavailability and potency of the administered compound. Adjusting the dose to achieve maximal efficacy based on the methods described above and other methods as are well-known in the art is well within the capabilities of the ordinarily skilled artisan.
- compositions of the invention are administered in pharmaceutically acceptable solutions, which may routinely contain pharmaceutically acceptable concentrations of salt, buffering agents, preservatives, compatible carriers, adjuvants, and optionally other therapeutic ingredients.
- an effective amount of the nucleic acid can be administered to a subject by any mode that delivers the nucleic acid to a subject.
- administering the pharmaceutical composition of the present invention may be accomplished by any means known to the skilled artisan. Some routes of administration include but are not limited to oral, intranasal, intratracheal, inhalation, ocular, vaginal, rectal, parenteral (e.g., intramuscular, intradermal, intravenous or subcutaneous injection) and direct injection.
- the compounds i.e., nucleic acids and antibodies
- pharmaceutically acceptable carriers well known in the art.
- pharmaceutically-acceptable carrier means one or more compatible solid or liquid filler, dilutants or encapsulating substances which are suitable for administration to a human or other vertebrate animal.
- carrier denotes an organic or inorganic ingredient, natural or synthetic, with which the active ingredient is combined to facilitate the application.
- the components of the pharmaceutical compositions also are capable of being commingled with the compounds of the present invention, and with each other, in a manner such that there is no interaction which would substantially impair the desired pharmaceutical efficiency.
- Such carriers enable the compounds of the invention to be formulated as tablets, pills, dragees, capsules, liquids, gels, syrups, slurries, suspensions and the like, for oral ingestion by a subject to be treated.
- Pharmaceutical preparations for oral use can be obtained as solid excipient, optionally grinding a resulting mixture, and processing the mixture of granules, after adding suitable auxiliaries, if desired, to obtain tablets or dragee cores.
- Suitable excipients are, in particular, fillers such as sugars, including lactose, sucrose, mannitol, or sorbitol; cellulose preparations such as, for example, maize starch, wheat starch, rice starch, potato starch, gelatin, gum tragacanth, methyl cellulose, hydroxypropylmethyl-cellulose, sodium carboxymethylcellulose, and/or polyvinylpyrrolidone (PNP).
- disintegrating agents may be added, such as the cross-linked polyvinyl pyrrolidone, agar, or alginic acid or a salt thereof such as sodium alginate.
- the oral formulations may also be fo ⁇ nulated in saline or buffers for neutralizing internal acid conditions.
- Dragee cores may be provided with suitable coatings.
- suitable coatings For this purpose, concentrated sugar solutions may be used, which may optionally contain gum arabic, talc, polyvinyl pyrrohdone, carbopol gel, polyethylene glycol, and/or titanium dioxide, lacquer solutions, and suitable organic solvents or solvent mixtures.
- Dyestuffs or pigments may be added to the tablets or dragee coatings for identification or to characterize different combinations of active compound doses.
- compositions which can be used orally include push-fit capsules made of gelatin, as well as soft, sealed capsules made of gelatin and a plasticizer, such as glycerol or sorbitol.
- the push-fit capsules can contain the active ingredients in admixture with filler such as lactose, binders such as starches, and/or lubricants such as talc or magnesium stearate and, optionally, stabilizers, h soft capsules, the active compounds may be dissolved or suspended in suitable liquids, such as fatty oils, liquid paraffin, or liquid polyethylene glycols. In addition, stabilizers may be added.
- suitable liquids such as fatty oils, liquid paraffin, or liquid polyethylene glycols.
- stabilizers may be added.
- Microspheres formulated for oral administration may also be used. Such microspheres have been well defined in the art. All formulations for oral administration should be in dosages suitable for such administration.
- the compositions may take the form of tablets or lozenges formulated in conventional manner.
- the compounds for use according to the present invention may be conveniently delivered in the form of an aerosol spray, from pressurized packs or a nebulizer, with the use of a suitable propellant, e.g., dichlorodifluoromethane, trichlorofluoromethane, dichlorotetrafluoroethane, carbon dioxide or other suitable gas.
- a suitable propellant e.g., dichlorodifluoromethane, trichlorofluoromethane, dichlorotetrafluoroethane, carbon dioxide or other suitable gas.
- a pressurized aerosol the dosage unit may be determined by providing a valve to deliver a metered amount.
- Capsules and cartridges of e.g., gelatin for use in an inhaler or insufflator may be formulated containing a powder mix of the compound and a suitable powder base such as lactos
- the compounds when it is desirable to deliver them systemically, may be formulated for parenteral administration by injection, e.g., by bolus injection or continuous infusion.
- Formulations for injection may be presented in unit dosage form, e.g., in ampoules or in multi-dose containers, with an added preservative.
- the compositions may take such forms as suspensions, solutions or emulsions in oily or aqueous vehicles, and may contain formulatory agents such as suspending, stabilizing and/or dispersing agents.
- compositions for parenteral administration include aqueous solutions of the active compounds in water-soluble form. Additionally, suspensions of the active compounds may be prepared as appropriate oily injection suspensions. Suitable lipophilic solvents or vehicles include fatty oils such as sesame oil, or synthetic fatty acid esters, such as ethyl oleate or triglycerides, or liposomes. Aqueous injection suspensions may contain substances which increase the viscosity of the suspension, such as sodium carboxymethyl cellulose, sorbitol, or dextran. Optionally, the suspension may also contain suitable stabilizers or agents which increase the solubility of the compounds to allow for the preparation of highly concentrated solutions.
- the active compounds may be in powder form for constitution with a suitable vehicle, e.g., sterile pyrogen-free water, before use.
- a suitable vehicle e.g., sterile pyrogen-free water
- the compounds may also be formulated in rectal or vaginal compositions such as suppositories or retention enemas, e.g., containing conventional suppository bases such as cocoa butter or other glycerides.
- the compounds may also be formulated as a depot preparation.
- Such long acting formulations may be formulated with suitable polymeric or hydrophobic materials (for example as an emulsion in an acceptable oil) or ion exchange resins, or as sparingly soluble derivatives, for example, as a sparingly soluble salt.
- compositions also may comprise suitable solid or gel phase carriers or excipients.
- suitable solid or gel phase carriers or excipients include but are not limited to calcium carbonate, calcium phosphate, various sugars, starches, cellulose derivatives, gelatin, and polymers such as polyethylene glycols.
- Suitable liquid or solid pharmaceutical preparation forms are, for example, aqueous or saline solutions for inhalation, microencapsulated, encochleated, coated onto microscopic gold particles, contained in liposomes, nebulized, aerosols, pellets for implantation into the skin, or dried onto a sharp object to be scratched into the skin.
- the pharmaceutical compositions may also include granules, powders, tablets, coated tablets, (micro)capsules, suppositories, syrups, emulsions, suspensions, creams, drops or preparations with protracted release of active compounds, in whose preparation excipients and additives and/or auxiliaries such as disintegrants, binders, coating agents, swelling agents, lubricants, flavorings, sweeteners or solubilizers are customarily used as described above.
- the pharmaceutical compositions are suitable for use in a variety of drug delivery systems. For a brief review of present methods for drug delivery, see Langer R, Science 249:1527-33 (1990), which is incorporated herein by reference.
- the nucleic acids and/or antibodies may be administered per se (neat) or in the form of a pharmaceutically acceptable salt.
- the salts should be pharmaceutically acceptable, but non-pharmaceutically acceptable salts may conveniently be used to prepare pharmaceutically acceptable salts thereof.
- Such salts include, but are not limited to, those prepared from the following acids: hydrochloric, hydrobromic, sulphuric, nitric, phosphoric, maleic, acetic, salicylic, p-toluene sulphonic, tartaric, citric, methane sulphonic, formic, malonic, succinic, naphthalene-2-sulphonic, and benzene sulphonic.
- salts can be prepared as alkaline metal or alkaline earth salts, such as sodium, potassium or calcium salts of the carboxylic acid group.
- Suitable buffering agents include: acetic acid and a salt (1-2% w/v); citric acid and a salt (1-3% w/v); boric acid and a salt (0.5-2.5% w/v); and phosphoric acid and a salt (0.8-2% w/v).
- Suitable preservatives include benzalkonium chloride (0.003-0.03% w/v); chlorobutanol (0.3-0.9% w/v); parabens (0.01-0.25% w/v) and thimerosal (0.004-0.02% w/v).
- the nucleic acids or other therapeutics useful in the invention may be delivered in mixtures with additional antibodies. A mixture may consist of several antibodies in addition to the nucleic acid.
- a variety of administration routes are available. The particular mode selected will depend, of course, upon the particular nucleic acids or antibodies selected, the particular condition being treated and the dosage required for therapeutic efficacy.
- the methods of this invention may be practiced using any mode of administration that is medically acceptable, meaning any mode that produces effective levels of an immune response without causing clinically unacceptable adverse effects. Preferred modes of administration are discussed above.
- compositions may conveniently be presented in unit dosage form and may be prepared by any of the methods well known in the art of pharmacy. All methods include the step of bringing the compounds into association with a carrier which constitutes one or more accessory ingredients. In general, the compositions are prepared by uniformly and intimately bringing the compounds into association with a liquid carrier, a finely divided solid carrier, or both, and then, if necessary, shaping the product.
- Liquid dose units are vials or ampoules. Solid dose units are tablets, capsules and suppositories.
- Other delivery systems can include time-release, delayed release or sustained release delivery systems. Such systems can avoid repeated administrations of the compounds, increasing convenience to the subject and the physician.
- Many types of release delivery systems are available and known to those of ordinary skill in the art. They include polymer base systems such as poly(lactide-glycolide), copolyoxalates, polycaprolactones, polyesteramides, polyorthoesters, polyhydroxybutyric acid, and polyanhydrides. Microcapsules of the foregoing polymers containing drugs are described in, for example, U.S. Patent No. 5,075,109.
- Delivery systems also include non-polymer systems that are: lipids including sterols such as cholesterol, cholesterol esters and fatty acids or neutral fats such as mono-, di-, and tri-glycerides; hydrogel release systems; sylastic systems; peptide based systems; wax coatings; compressed tablets using conventional binders and excipients; partially fused implants; and the like.
- lipids including sterols such as cholesterol, cholesterol esters and fatty acids or neutral fats such as mono-, di-, and tri-glycerides
- hydrogel release systems such as lipids including sterols such as cholesterol, cholesterol esters and fatty acids or neutral fats such as mono-, di-, and tri-glycerides
- sylastic systems such as cholesterol, cholesterol esters and fatty acids or neutral fats such as mono-, di-, and tri-glycerides
- peptide based systems such as fatty acids
- wax coatings such as those described in U.S. Patent Nos.
- the nucleic acid may be directly administered to the subject or may be administered in conjunction with a pharmaceutically acceptable carrier or a delivery vehicle.
- the nucleic acid and optionally other therapeutic agents may be administered alone (e.g., in saline or buffer) or using any delivery vehicles known in the art.
- One type of delivery vehicle is referred to herein as a nucleic acid delivery complex.
- a "nucleic acid delivery complex” shall mean a nucleic acid molecule associated with (e.g., ionically or covalently bound to; or encapsulated within) a targeting means (e.g., a molecule that results in higher affinity binding to target cell (e.g., dendritic cell surfaces and/or increased cellular uptake by target cells).
- nucleic acid delivery complexes include nucleic acids associated with: a sterol (e.g., cholesterol), a lipid (e.g., a cationic lipid, virosome or liposome), or a target cell specific binding agent (e.g., a ligand recognized by target cell specific receptor).
- a sterol e.g., cholesterol
- a lipid e.g., a cationic lipid, virosome or liposome
- a target cell specific binding agent e.g., a ligand recognized by target cell specific receptor
- Preferred complexes may be sufficiently stable in vivo to reduce significant uncoupling prior to internalization by the target cell. However, the complex may be cleavable under appropriate conditions within the cell so that the nucleic acid may be released in a functional form.
- the nucleic acids may be delivered by non-invasive methods as described above.
- Non-invasive delivery of compounds is desirable for treatment of children, elderly, animals, and even adults and also to avoid the risk of needle-stick injury.
- Delivery vehicles for delivering compounds to mucosal surfaces have been described and include but are not limited to: Cochleates (Gould-Fogerite et al., 1994, 1996); Emulsomes (Vancott et al., 1998, Lowell et al., 1997); ISCOMs (Mowat et al., 1993, Carlsson et al., 1991, Hu et al., 1998, Morein et al., 1999); Liposomes (Childers et al., 1999, Michalek et al., 1989, 1992, de Haan 1995a, 1995b); Live bacterial vectors (e.g., Salmonella, Escherichia coli, Bacillus Calmette- Guerin, Shigella, Lactobacillus) (Hone et al., 1996, Pouwels et al., 1998
- kits generally include a package with a plurality of containers housing active agents and instructions for carrying out the methods of the invention.
- the active agents include but are not limited to immunostimulatory nucleic acids, antibodies such as antibodies specific for a cell surface antigen, and anti-cancer therapies.
- a variety of cellular receptors and antigens are involved in growth, differentiation and apoptosis of B-cell malignancies.
- Antibodies or ligands against a variety of antigens can cause growth inhibition or even apoptosis including CD20, surface immunoglobulins, MHC II, CD80, CD86 and CD40.
- mononuclear cells were obtained from peripheral blood or pleural fluid as described. Hartmann G et al., J Pharmacol Exp Ther 285:920-8 (1998). Red blood cells were removed by resuspending the cells in 5 ml ACK lysis buffer according to standard procedures. Cells were frozen slowly and stored in liquid nitrogen.
- Oligonucleotides Nuclease-resistant phosphorothioate-modified oligodeoxynucleotide (ODN) were purchased from Operon Technologies (Alameda, CA) and Hybridon Specialty Products (Milford, MA). Sequences were as follows: CpG ODN 2006: 5'-TCGTCGTTTTGTCGTTTTGTCGTT-3' (SEQ ID NO: 729), and control ODN 2017: 5'-CCCCCCCCCCCCCCCCCC-3' (SEQ J-D NO: 168). ODN was diluted in TE (10 mM Tris-HCl, 1 mM EDTA, pH 8) using pyrogen-free reagents. ODN was added at a final concentration of 5 ⁇ g/ml.
- Monoclonal antibodies to CD40 (5C3), CD69 (FN50), CD80 (L307.4), CD86 (IT2.2), CD54 (HA58), MHC I (G46-2.6) and MHC II (TU39) as well as isotype controls (IgGl, MOPC-21 and IgG2a, G155-178) were purchased from PharMingen, San Diego, CA.
- FITC-labeled polyclonal anti-human Ig was purchased from Southern Biotech, Birmingham, AL. 1D10, a monoclonal humanized antibody directed against a variant of HLA-DR was produced in our laboratory as described earlier. Link BK et al., Blood 81 :3343-9 (1993).
- C2B8 a monoclonal humanized anti-CD20 antibody, was purchased from J-DEC Pharmaceuticals, San Diego, CA. 1D10 and C2B8 were labeled with FITC according to standard protocols. The analysis gate was set on viable cells identified according to FSC/SSC characteristics and Annexin V staining (> 97 % viable cells within analysis gate). Spectral overlap was corrected by appropriate compensation. Flow cytometric data from 1 x 10 4 cells per sample were acquired on a FACScan (Beckton Dickinson hnmunocytometry Systems, San Jose, CA). Data were analyzed using the computer program FlowJo (version 2.5.1, Tree Star, Inc., Stanford, CA).
- CFSE staining CFSE 5- (and 6-) carboxyfluorescein diacetate succinimidyl ester, Molecular Probes, USA, is a fluorescein-derived intracellular fluorescent label which is divided equally between daughter cells upon cell division. Staining of cells with CFSE allows both quantification and immunophenotyping of proliferating cells in a mixed cell suspension. Interference between oligonucleotide degradation products and thymidine uptake (standard proliferation assay) is avoided by using this method. The technique has described in detail previously. Lyons AB et al., J Immunol Methods 171:131-7 (1994).
- TUNEL assay A two-color DNA strand break labeling assay, based on a modification of the assay described by Li et al. (Li X et al., ExpCell Res 222:28-37 (1996)) was used to assess B-cell proliferation in response to CpG ODN. This assay involved terminal transferase-mediated dUTP nick end labeling (TUNEL) before and after induction of DNA strand breaks in BrdU-labeled cells. Briefly, cells were cultured for 3 days with and without ODN. They were then incubated for 16 hours in lO ⁇ M BrdU and placed onto slides by cytospin.
- TUNEL terminal transferase-mediated dUTP nick end labeling
- TUNEL staining steps included incubating slides in 50 ⁇ l of TdT mix (34 ⁇ l distilled water, lO ⁇ l of 5X TdT buffer, 5 ⁇ l of 25mM cobalt chloride, 12.5 units terminal transferase and 0.5nmol fluorochrome-conjugated-dUTP) (Boeliringer-Marrnheim) under a coverslip for one hour at 37°C in a humidified chamber.
- the slides were then washed in 5 quick changes of distilled water followed by 3 changes of 2XSSC containing 30% formamide for 5 minutes each at room temperature.
- TUNEL labeling step cells were counterstained for CD 19, and also stained with Wright solution for blood cell differentiation and mounted in Vectashield media containing DAPI counterstain (Vector Laboratories, Burlingame, CA). The morphology and staining of cells were assessed using both visible light and fluorescence microscopy. Apoptotic cells were identified by green fluorescence (FITC label), and proliferating cells by red fluorescence (TMR label). The percentage of apoptotic and proliferating cells was determined by counting at least 200 cells per sample by three observers blinded to whether cells were treated with ODN. Mean and standard error were determined for each sample based on these three readings.
- Example 1 Immunostimulatory nucleic acids induce morphological and phenotypic changes in malignant B cells.
- FIG. 1 depicts the morphologic changes of marginal zone lymphoma cells upon
- CpG ODN stimulation Malignant B cells from a patient with marginal zone lymphoma were stimulated with 5 ⁇ g/ml of no ODN (A and D), control ODN (B and E) or CpG ODN (C and F) for 72 hours and analyzed by flow cytometry.
- A, B, and C illustrate FSC (x-axis) vs. SSC (y-axis).
- D, E and F illustrate CD 19 expression (x-axis) against FSC (y-axis), allowing for separation of B cells from other leukocyte subpopulations.
- CpG ODN B cells shifted up and to the right, indicating an increase in granularity and size.
- Figure 2 depicts the expression of surface antigens on marginal zone lymphoma cells upon CpG ODN treatment.
- Flow cytometric analysis of surface antigen expression on malignant B cells from a patient with marginal zone lymphoma was performed 72 hours after stimulation with 5 ⁇ g/ml of either CpG ODN or non-CpG ODN.
- CpG ODN median fluorescence intensity for all markers tested shifted to the right, indicating an increase in surface expression.
- Thin curves indicate incubation with medium alone, dotted curves incubation with control ODN, and bold curves incubation with CpG ODN.
- Figure 3 depicts the expression of surface antigens on primary cells representing different B-cell malignancies and cells of a benign follicular hyperplasia upon CpG ODN treatment.
- Cells from lymph node biopsies, peripheral blood or pleural fluid from patients with different B-cell malignancies were incubated for 72 hours with either media alone, control ODN or CpG ODN. Each panel represents one experiment.
- CD20 was expressed to varying degrees in all samples tested. As is well known, baseline CD20 expression was lower in the B-CLL samples when compared to the B-cell malignancies of other histologies. CpG-ODN 2006 but not the control ODN 2017 increased CD20 expression in both B-CLLs and both marginal zone lymphomas. No or only little upregulation was seen in the other lymphoma samples. Non-malignant CD19+ cells derived from the reactive follicular hyperplasia decreased CD20 expression in response to CpG (Fig. 3).
- Table 5 Percentage Of CD 19+ Cells In Samples Tested.
- Example 2 Immunostimulatory nucleic acids induce proliferation and apoptosis of malignant B cells.
- CpG induces a strong proliferative response of primary human B cells. Hartmann G et al., J Immunol 164:944-53 (2000). Two techniques were used to assess whether CpG ODN is capable of inducing proliferation of B-CLL cells. For select samples, cells were stained with CFSE and incubated for four days. Proliferation of cells is indicated by a loss of CFSE stain with every cell division.
- CD5 can be used to identify malignant B cells among CD19+ cells.
- Figure 5 shows a comparison of CpG ODN induced proliferation of malignant and normal B cells.
- Peripheral blood mononuclear cells from two patients, one with B-CLL and one with marginal zone lymphoma with circulating malignant cells were incubated for 72 hours with CpG ODN or medium alone and evaluated by two-color flow cytometry.
- CFSE fluorescence (x-axis) and expression of CD5 (CLL) or CD 19 (marginal zone lymphoma) (y- axis) were evaluated.
- CLL CpG ODN enhanced proliferation of both CD5+ and the CD5- cells.
- the relative number of proliferating cells and the number of divisions is lower in the CD5- subset than in the CD5+ subset.
- marginal zone lymphoma CpG ODN enhanced proliferation in the CD 19+ cell subset.
- Table 7 Apoptosis And Proliferation As Determined By TUNEL.
- Example 3 CpG ODN enhance the therapeutic effect of murine IgG2a (which relates to human IgGl) but not murine IgGl (which relates to human IgG2) anti-tumor antibody.
- CpG ODN when combined with antibody of murine subtype IgG2a dramatically promotes survival in mice having tumors. Mice were injected i.p. with 5000 T3C cells on day 0. They were then given 100 ⁇ g anti-idiotype monoclonal antibody as either IgGl (MS5A10) or IgG2a (MSI 1G6) on days 5, 7, and 10. In this model, the target antigen is the idiotype expressed by the lymphoma cells.
- the anti-tumor antibodies are also "anti-idiotype.” These antibodies (MS5A10 and MSI 1G6) are simultaneously both anti- tumor antibodies and anti-idiotype antibodies. Twenty micrograms of CpG ODN 1826 (5' TCCATGACGTTCCTGACGTT 3'; SEQ ID NO: 560) was given at the same time. Results are shown in Figure 6. Untreated controls had a median survival time (MST) of 17 days after inoculation with tumor. Mice treated with murine IgGl antibody plus CpG ODN had survival that was similar to those treated with murine IgGl antibody alone (MST 28 days and 27 days, respectively). In contrast, mice treated with murine IgG2a plus CpG ODN had survival that was significantly improved when compared to mice treated with murine IgG2a alone (MST 45 days and 37 days, respectively).
- MST median survival time
Abstract
Description
Claims
Priority Applications (9)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| DK01948684T DK1296714T3 (en) | 2000-06-22 | 2001-06-22 | Combination of CpG and antibodies directed against CD19, CD20, CD22 or CD40 for the treatment or prevention of cancer |
| DE60139689T DE60139689D1 (en) | 2000-06-22 | 2001-06-22 | Combination of CpG and antibodies against CD19, CD20, CD22 or CD40 for the prevention or treatment of cancer. |
| CA2410371A CA2410371C (en) | 2000-06-22 | 2001-06-22 | Methods for enhancing antibody-induced cell lysis and treating cancer |
| SI200130937T SI1296714T1 (en) | 2000-06-22 | 2001-06-22 | Combination of CpG and antibodies directed against CD19,CD20, CD22 or CD40 for the treatment or prevention of cancer. |
| EP01948684A EP1296714B1 (en) | 2000-06-22 | 2001-06-22 | Combination of CpG and antibodies directed against CD19,CD20, CD22 or CD40 for the treatment or prevention of cancer. |
| AT01948684T ATE440618T1 (en) | 2000-06-22 | 2001-06-22 | COMBINATION OF CPG AND ANTIBODIES AGAINST CD19, CD20,CD22 OR CD40 FOR THE PREVENTION OR TREATMENT OF CANCER. |
| JP2002503327A JP2003535907A (en) | 2000-06-22 | 2001-06-22 | Method for promoting antibody-induced cell lysis and treating cancer |
| AU2001270134A AU2001270134B2 (en) | 2000-06-22 | 2001-06-22 | Methods for enhancing antibody-induced cell lysis and treating cancer |
| AU7013401A AU7013401A (en) | 2000-06-22 | 2001-06-22 | Methods for enhancing antibody-induced cell lysis and treating cancer |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US21334600P | 2000-06-22 | 2000-06-22 | |
| US60/213,346 | 2000-06-22 |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| WO2001097843A2 true WO2001097843A2 (en) | 2001-12-27 |
| WO2001097843A3 WO2001097843A3 (en) | 2003-01-23 |
Family
ID=22794755
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| PCT/US2001/020154 WO2001097843A2 (en) | 2000-06-22 | 2001-06-22 | Methods for enhancing antibody-induced cell lysis and treating cancer |
Country Status (12)
| Country | Link |
|---|---|
| US (1) | US7534772B2 (en) |
| EP (1) | EP1296714B1 (en) |
| JP (1) | JP2003535907A (en) |
| AT (1) | ATE440618T1 (en) |
| AU (5) | AU7013401A (en) |
| CA (1) | CA2410371C (en) |
| DE (1) | DE60139689D1 (en) |
| DK (1) | DK1296714T3 (en) |
| ES (1) | ES2332444T3 (en) |
| PT (1) | PT1296714E (en) |
| SI (1) | SI1296714T1 (en) |
| WO (1) | WO2001097843A2 (en) |
Cited By (45)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| EP1435987A1 (en) * | 2001-09-07 | 2004-07-14 | The Trustees of Boston University | Method and composition for treating immune complex associated disorders |
| EP1501359A2 (en) * | 2001-08-03 | 2005-02-02 | Celldex Therapeutics, Inc. | Compositions comprising immunostimulatory oligonucleotides and uses thereof to enhance fc receptor-mediated immunotherapies |
| WO2005111057A2 (en) * | 2004-04-02 | 2005-11-24 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for inducing il-10 responses |
| JP2006514689A (en) * | 2002-11-06 | 2006-05-11 | セルジーン・コーポレーション | Methods and compositions using immunomodulatory compounds for the treatment and management of cancer and other diseases |
| JPWO2004078764A1 (en) * | 2003-03-04 | 2006-06-08 | 株式会社そーせい | Antitumor effect potentiator comprising GM-95 substance, antitumor combination preparation and antitumor agent |
| JP2006528697A (en) * | 2003-05-16 | 2006-12-21 | イデラ ファーマシューティカルズ インコーポレイテッド | Synergistic treatment of cancer using immunomers in combination with chemotherapeutic agents |
| JP2007509040A (en) * | 2003-10-11 | 2007-04-12 | イネックス ファーマシューティカルズ コーポレイション | Methods and compositions for enhancing innate immunity and antibody-dependent cytotoxicity |
| EP1809671A2 (en) * | 2004-11-09 | 2007-07-25 | University Of Southern California | Targeted innate immunity |
| EP1859793A1 (en) * | 2005-02-28 | 2007-11-28 | Eisai R&D Management Co., Ltd. | Novel combinational use of sulfonamide compound |
| EP1883411A1 (en) * | 2005-05-17 | 2008-02-06 | Changchun Huapu Biotechnology Co., Ltd. | An oligonucleotide or its functional homologue, a composition comprising the same and a method for treating b cell neoplasm |
| WO2008014979A2 (en) * | 2006-07-31 | 2008-02-07 | Curevac Gmbh | NUCLEIC ACID OF FORMULA (I): GIXmGn, OR (II): CIXmCn, IN PARTICULAR AS AN IMMUNE-STIMULATING AGENT/ADJUVANT |
| WO2008132500A2 (en) * | 2007-04-27 | 2008-11-06 | Astrazeneca Ab | Chkl inhibitors with b cell depleting antibodies for the treatment of hematologic malignancies |
| WO2009154565A1 (en) * | 2008-06-18 | 2009-12-23 | Index Pharmaceuticals Ab | Combination therapies against cancer |
| WO2010053433A1 (en) * | 2008-11-04 | 2010-05-14 | Index Pharmaceuticals Ab | Increased expression of specific antigens |
| US7741297B2 (en) | 2002-02-04 | 2010-06-22 | Oncothyreon Inc. | Immunostimulatory, covalently lipidated oligonucleotides |
| US7850962B2 (en) | 2004-04-20 | 2010-12-14 | Genmab A/S | Human monoclonal antibodies against CD20 |
| SG166673A1 (en) * | 2002-08-19 | 2010-12-29 | Coley Pharm Group Inc | Immunostimulatory nucleic acids |
| US8084015B2 (en) * | 2002-02-14 | 2011-12-27 | United Biomedical, Inc. | Stabilized synthetic immunogen delivery system |
| US8148341B2 (en) | 2005-07-01 | 2012-04-03 | Index Pharmaceuticals Ab | Method for modulating responsiveness to steroids |
| US8258106B2 (en) * | 1994-07-15 | 2012-09-04 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| US8258107B2 (en) | 2005-07-01 | 2012-09-04 | Index Pharmaceuticals Ab | Immunostimulatory method |
| US8304396B2 (en) | 2002-08-19 | 2012-11-06 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids |
| US8349792B2 (en) | 2006-12-19 | 2013-01-08 | Cyclacel Limited | Combination comprising CNDAC (2′-cyano-2′-deoxy-N4-palmitoyl-1-beta-D-arabinofuranosyl-cytosine) and a cytotoxic agent |
| US8444973B2 (en) | 2005-02-15 | 2013-05-21 | Duke University | Anti-CD19 antibodies and uses in B cell disorders |
| US8524867B2 (en) | 2006-08-14 | 2013-09-03 | Xencor, Inc. | Optimized antibodies that target CD19 |
| US8530445B2 (en) | 2008-06-09 | 2013-09-10 | Cyclacel Limited | Combinations of sapacitabine or CNDAC with DNA methyltransferase inhibitors such as decitabine and procaine |
| US8529902B2 (en) | 2002-10-17 | 2013-09-10 | Genmab A/S | Human monoclonal antibodies against CD20 |
| EP2650368A1 (en) * | 2006-07-31 | 2013-10-16 | CureVac GmbH | Nucleic acid of formula (I): GlXmGn, or (II): ClXmCn, in particular as an immune-stimulating agent/adjuvant |
| JP2014065735A (en) * | 2002-09-13 | 2014-04-17 | Lab Francais Du Fractionnement Et Des Biotechnologies | Treatment of pathologies which escape the immune response, using optimised antibodies |
| US8834900B2 (en) | 2001-08-17 | 2014-09-16 | University Of Iowa Research Foundation | Combination motif immune stimulatory oligonucleotides with improved activity |
| US8895522B2 (en) | 2005-10-28 | 2014-11-25 | Index Pharmaceuticals Ab | Composition and method for the prevention, treatment and/or alleviation of an inflammatory disease |
| US8968746B2 (en) | 2010-07-30 | 2015-03-03 | Curevac Gmbh | Complexation of nucleic acids with disulfide-crosslinked cationic components for transfection and immunostimulation |
| US9050378B2 (en) | 2003-12-10 | 2015-06-09 | Board Of Regents, The University Of Texas System | N2S2 chelate-targeting ligand conjugates |
| US9226959B2 (en) | 2008-01-31 | 2016-01-05 | Curevac Ag | Nucleic acids comprising formula (NuGlXmGnNv)a and derivatives thereof as immunostimulating agent/adjuvant |
| US9314535B2 (en) | 2009-09-03 | 2016-04-19 | Curevac Ag | Disulfide-linked polyethyleneglycol/peptide conjugates for the transfection of nucleic acids |
| US9572874B2 (en) | 2008-09-30 | 2017-02-21 | Curevac Ag | Composition comprising a complexed (M)RNA and a naked mRNA for providing or enhancing an immunostimulatory response in a mammal and uses thereof |
| EP3096787A4 (en) * | 2014-01-22 | 2018-02-07 | The Board of Trustees of the Leland Stanford Junior University | Methods and compositions for antibody and antibody-loaded dendritic cell mediated therapy |
| US10111967B2 (en) | 2007-09-04 | 2018-10-30 | Curevac Ag | Complexes of RNA and cationic peptides for transfection and for immunostimulation |
| US10226478B2 (en) | 2011-04-14 | 2019-03-12 | Cyclacel Limited | Dosage regimen for sapacitabine and decitabine in combination for treating acute myeloid leukemia |
| US10369216B2 (en) | 2014-04-01 | 2019-08-06 | Curevac Ag | Polymeric carrier cargo complex for use as an immunostimulating agent or as an adjuvant |
| US10675358B2 (en) | 2016-07-07 | 2020-06-09 | The Board Of Trustees Of The Leland Stanford Junior University | Antibody adjuvant conjugates |
| US10814013B2 (en) | 2006-10-05 | 2020-10-27 | The Board Of Regents Of The University Of Texas System | Efficient synthesis of chelators for nuclear imaging and radiotherapy: compositions and applications |
| US11400164B2 (en) | 2019-03-15 | 2022-08-02 | Bolt Biotherapeutics, Inc. | Immunoconjugates targeting HER2 |
| US11690910B2 (en) | 2012-01-31 | 2023-07-04 | CureVac SE | Pharmaceutical composition comprising a polymeric carrier cargo complex and at least one protein or peptide antigen |
| US11739125B2 (en) | 2013-08-21 | 2023-08-29 | Cure Vac SE | Respiratory syncytial virus (RSV) vaccine |
Families Citing this family (158)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US6727230B1 (en) * | 1994-03-25 | 2004-04-27 | Coley Pharmaceutical Group, Inc. | Immune stimulation by phosphorothioate oligonucleotide analogs |
| US6239116B1 (en) * | 1994-07-15 | 2001-05-29 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| US6429199B1 (en) * | 1994-07-15 | 2002-08-06 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules for activating dendritic cells |
| US7935675B1 (en) * | 1994-07-15 | 2011-05-03 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| US20030026782A1 (en) * | 1995-02-07 | 2003-02-06 | Arthur M. Krieg | Immunomodulatory oligonucleotides |
| JP4359654B2 (en) * | 1996-01-30 | 2009-11-04 | ザ リージェンツ オブ ザ ユニバーシティー オブ カリフォルニア | Gene expression vector for generating antigen-specific immune response and method of use thereof |
| EP0855184A1 (en) * | 1997-01-23 | 1998-07-29 | Grayson B. Dr. Lipford | Pharmaceutical composition comprising a polynucleotide and an antigen especially for vaccination |
| US6406705B1 (en) * | 1997-03-10 | 2002-06-18 | University Of Iowa Research Foundation | Use of nucleic acids containing unmethylated CpG dinucleotide as an adjuvant |
| US20030158220A1 (en) * | 1997-11-03 | 2003-08-21 | Foss Joseph F. | Use of methylnaltrexone and related compounds to treat chronic opioid use side effects |
| US6274591B1 (en) * | 1997-11-03 | 2001-08-14 | Joseph F. Foss | Use of methylnaltrexone and related compounds |
| WO1999051259A2 (en) * | 1998-04-03 | 1999-10-14 | University Of Iowa Research Foundation | Methods and products for stimulating the immune system using immunotherapeutic oligonucleotides and cytokines |
| NZ508650A (en) * | 1998-05-14 | 2003-05-30 | Coley Pharm Gmbh | Regulating hematopoiesis using unmethylated C and G CpG-oligonucleotides with a phosphorothioate modification |
| DE69932717T2 (en) | 1998-05-22 | 2007-08-09 | Ottawa Health Research Institute, Ottawa | METHODS AND PRODUCTS FOR INDUCING MUCOSAL IMMUNITY |
| US20030022854A1 (en) | 1998-06-25 | 2003-01-30 | Dow Steven W. | Vaccines using nucleic acid-lipid complexes |
| US6693086B1 (en) * | 1998-06-25 | 2004-02-17 | National Jewish Medical And Research Center | Systemic immune activation method using nucleic acid-lipid complexes |
| ATE464907T1 (en) * | 1999-02-17 | 2010-05-15 | Csl Ltd | IMMUNOGENIC COMPLEXES AND METHODS RELATING THEM |
| EP1176966B1 (en) | 1999-04-12 | 2013-04-03 | THE GOVERNMENT OF THE UNITED STATES OF AMERICA, as represented by THE SECRETARY, DEPARTMENT OF HEALTH AND HUMAN SERVICES | Oligodeoxynucleotide and its use to induce an immune response |
| US6977245B2 (en) | 1999-04-12 | 2005-12-20 | The United States Of America As Represented By The Department Of Health And Human Services | Oligodeoxynucleotide and its use to induce an immune response |
| EP1642596A3 (en) * | 1999-05-07 | 2006-04-12 | Genentech, Inc. | Treatment of autoimmune diseases with antagonists which bind to B cell surface markers |
| BR0013201A (en) * | 1999-07-12 | 2002-04-30 | Genentech Inc | Method of blocking an immune response to an external antigen in mammals through the use of an antagonist that binds to cd20, method of treating mammals, method of treating a disease of graft versus host or host versus graft in mammals, method of numbness of mammals awaiting transplantation and industrialized article |
| AP2006003503A0 (en) * | 1999-09-25 | 2006-02-28 | Univ Iowa Res Found | Immunostimulatory nucleic acids. |
| US6949520B1 (en) * | 1999-09-27 | 2005-09-27 | Coley Pharmaceutical Group, Inc. | Methods related to immunostimulatory nucleic acid-induced interferon |
| AU3108001A (en) * | 2000-01-20 | 2001-12-24 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for inducing a th2 immune response |
| US7585847B2 (en) * | 2000-02-03 | 2009-09-08 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for the treatment of asthma and allergy |
| DK1255558T3 (en) * | 2000-02-16 | 2006-10-23 | Genentech Inc | Anti-April antibodies and hybridoma cells |
| US20040131628A1 (en) * | 2000-03-08 | 2004-07-08 | Bratzler Robert L. | Nucleic acids for the treatment of disorders associated with microorganisms |
| US7030219B2 (en) | 2000-04-28 | 2006-04-18 | Johns Hopkins University | B7-DC, Dendritic cell co-stimulatory molecules |
| AU2001275294A1 (en) * | 2000-06-07 | 2001-12-17 | Biosynexus Incorporated. | Immunostimulatory RNA/DNA hybrid molecules |
| KR100917101B1 (en) * | 2000-08-04 | 2009-09-15 | 도요 보세키 가부시키가이샤 | Flexible metal laminate and production method thereof |
| WO2002022809A2 (en) * | 2000-09-15 | 2002-03-21 | Coley Pharmaceutical Gmbh | PROCESS FOR HIGH THROUGHPUT SCREENING OF CpG-BASED IMMUNO-AGONIST/ANTAGONIST |
| MXPA03002262A (en) * | 2000-09-18 | 2003-10-15 | Idec Pharma Corp | Combination therapy for treatment of autoimmune diseases using b cell depleting/immunoregulatory antibody combination. |
| TWI283575B (en) * | 2000-10-31 | 2007-07-11 | Eisai Co Ltd | Medicinal compositions for concomitant use as anticancer agent |
| ES2307568T3 (en) * | 2000-12-08 | 2008-12-01 | Coley Pharmaceutical Gmbh | CPG TYPE NUCLEIC ACIDS AND SAME USE METHODS. |
| US20030133939A1 (en) | 2001-01-17 | 2003-07-17 | Genecraft, Inc. | Binding domain-immunoglobulin fusion proteins |
| US7754208B2 (en) | 2001-01-17 | 2010-07-13 | Trubion Pharmaceuticals, Inc. | Binding domain-immunoglobulin fusion proteins |
| US7829084B2 (en) * | 2001-01-17 | 2010-11-09 | Trubion Pharmaceuticals, Inc. | Binding constructs and methods for use thereof |
| US7666674B2 (en) | 2001-07-27 | 2010-02-23 | The United States Of America As Represented By The Secretary Of The Department Of Health And Human Services | Use of sterically stabilized cationic liposomes to efficiently deliver CPG oligonucleotides in vivo |
| KR20040019105A (en) * | 2001-08-03 | 2004-03-04 | 제넨테크, 인크. | TACIs and BR3 Polypeptides and Uses Thereof |
| US7354909B2 (en) * | 2001-08-14 | 2008-04-08 | The United States Of America As Represented By Secretary Of The Department Of Health And Human Services | Method for rapid generation of mature dendritic cells |
| CA2461315A1 (en) * | 2001-10-05 | 2003-04-17 | Coley Pharmaceutical Gmbh | Toll-like receptor 3 signaling agonists and antagonists |
| AU2002360278A1 (en) * | 2001-10-12 | 2003-11-11 | Coley Pharmaceutical Gmbh | Methods and products for enhancing immune responses using imidazoquinoline compounds |
| US8466116B2 (en) | 2001-12-20 | 2013-06-18 | The Unites States Of America As Represented By The Secretary Of The Department Of Health And Human Services | Use of CpG oligodeoxynucleotides to induce epithelial cell growth |
| AU2002366710A1 (en) * | 2001-12-20 | 2003-07-09 | The Government Of The United States Of America As Represented By The Secretary Of The Department Of | USE OF CpG OLIGODEOXYNUCLEOTIDES TO INDUCE ANGIOGENESIS |
| US8153141B2 (en) * | 2002-04-04 | 2012-04-10 | Coley Pharmaceutical Gmbh | Immunostimulatory G, U-containing oligoribonucleotides |
| US20040009949A1 (en) * | 2002-06-05 | 2004-01-15 | Coley Pharmaceutical Group, Inc. | Method for treating autoimmune or inflammatory diseases with combinations of inhibitory oligonucleotides and small molecule antagonists of immunostimulatory CpG nucleic acids |
| CA2513143A1 (en) * | 2002-07-01 | 2004-01-08 | Tufts University | Methods and compositions for inhibition of multi-drug resistance by hyaluronan oligomers |
| US7576066B2 (en) | 2002-07-03 | 2009-08-18 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US20040053880A1 (en) * | 2002-07-03 | 2004-03-18 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US7605138B2 (en) * | 2002-07-03 | 2009-10-20 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US7569553B2 (en) * | 2002-07-03 | 2009-08-04 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US7807803B2 (en) | 2002-07-03 | 2010-10-05 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| MXPA05000940A (en) * | 2002-07-25 | 2005-05-16 | Genentech Inc | Taci antibodies and uses thereof. |
| US8263091B2 (en) * | 2002-09-18 | 2012-09-11 | The United States Of America As Represented By The Secretary Of The Department Of Health And Human Services | Method of treating and preventing infections in immunocompromised subjects with immunostimulatory CpG oligonucleotides |
| MXPA05004588A (en) * | 2002-10-29 | 2005-12-14 | Coley Pharmaceutical Group Ltd | Use of cpg oligonucleotides in the treatment of hepatitis c virus infection. |
| AU2003300919A1 (en) | 2002-12-11 | 2004-06-30 | Coley Pharmaceutical Gmbh | 5' cpg nucleic acids and methods of use |
| BRPI0316779B8 (en) * | 2002-12-16 | 2023-02-28 | Genentech Inc | HUMAN ANTI-CD20 ANTIBODY OR ANTIGEN-BINDING FRAGMENT THEREOF, ITS USES, COMPOSITION, MANUFACTURED ARTICLE AND LIQUID FORMULATION |
| US20040235770A1 (en) * | 2003-04-02 | 2004-11-25 | Coley Pharmaceutical Group, Ltd. | Immunostimulatory nucleic acid oil-in-water formulations and related methods of use |
| CN1767855A (en) * | 2003-04-08 | 2006-05-03 | 普罗热尼奇制药公司 | Combination therapy for constipation comprising a laxative and a peripheral opioid antagonist |
| US20050004155A1 (en) * | 2003-04-08 | 2005-01-06 | Boyd Thomas A. | Use of methylnaltrexone to treat irritable bowel syndrome |
| DK2368553T3 (en) * | 2003-04-08 | 2015-02-09 | Progenics Pharm Inc | Pharmaceutical preparation comprising methylnaltrexone |
| ZA200507805B (en) | 2003-04-09 | 2006-12-27 | Genentech Inc | Therapy of autoimmune disease in a patient with an inadequate response to a TNF-alpha inhibitor |
| US20050163775A1 (en) * | 2003-06-05 | 2005-07-28 | Genentech, Inc. | Combination therapy for B cell disorders |
| WO2005005462A2 (en) * | 2003-06-05 | 2005-01-20 | Genentech, Inc. | Blys antagonists and uses thereof |
| JP2007524615A (en) * | 2003-06-20 | 2007-08-30 | コーリー ファーマシューティカル ゲーエムベーハー | Low molecular weight Toll-like receptor (TLR) antagonist |
| US20050013812A1 (en) * | 2003-07-14 | 2005-01-20 | Dow Steven W. | Vaccines using pattern recognition receptor-ligand:lipid complexes |
| AU2004264601A1 (en) * | 2003-07-29 | 2005-02-24 | Genentech, Inc. | Assay for human anti CD20 antibodies and uses therefor |
| CN1845755A (en) * | 2003-08-29 | 2006-10-11 | 健泰科生物技术公司 | Anti-CD20 therapy of ocular disorders |
| CA2536139A1 (en) * | 2003-09-25 | 2005-04-07 | Coley Pharmaceutical Group, Inc. | Nucleic acid-lipophilic conjugates |
| CA2540949A1 (en) * | 2003-10-30 | 2005-05-12 | Coley Pharmaceutical Gmbh | C-class oligonucleotide analogs with enhanced immunostimulatory potency |
| US20050239733A1 (en) * | 2003-10-31 | 2005-10-27 | Coley Pharmaceutical Gmbh | Sequence requirements for inhibitory oligonucleotides |
| US20050100983A1 (en) * | 2003-11-06 | 2005-05-12 | Coley Pharmaceutical Gmbh | Cell-free methods for identifying compounds that affect toll-like receptor 9 (TLR9) signaling |
| CN1917901A (en) * | 2003-12-19 | 2007-02-21 | 健泰科生物技术公司 | Detection of cd20 in therapy of autoimmune diseases |
| MXPA06006865A (en) * | 2003-12-19 | 2006-08-23 | Genentech Inc | Detection of cd20 in transplant rejection. |
| CA2550058C (en) * | 2003-12-19 | 2016-07-12 | Antisense Pharma Gmbh | Pharmaceutical composition comprising a tgf-beta2 antisense oligonucleotide and a chemotherapeutic |
| EP1720568A2 (en) * | 2004-02-19 | 2006-11-15 | Coley Pharmaceutical Group, Inc. | Immunostimulatory viral rna oligonucleotides |
| TWI235440B (en) * | 2004-03-31 | 2005-07-01 | Advanced Semiconductor Eng | Method for making leadless semiconductor package |
| EP1735000A2 (en) * | 2004-04-16 | 2006-12-27 | Genentech, Inc. | Method for augmenting b cell depletion |
| BRPI0510224A (en) * | 2004-05-05 | 2007-10-23 | Genentech Inc | autoimmune disease prevention methods and industrialized article |
| US7531628B2 (en) * | 2004-05-28 | 2009-05-12 | Idexx Laboratories, Inc. | Canine CD20 compositions |
| DOP2005000108A (en) * | 2004-06-04 | 2007-06-15 | Genentech Inc | METHOD FOR TREATING LUPUS |
| RU2384345C2 (en) | 2004-06-04 | 2010-03-20 | Дженентек, Инк. | Method of treating multiple sclerosis |
| EP1781325A2 (en) * | 2004-07-18 | 2007-05-09 | CSL Limited | Immuno stimulating complex and oligonucleotide formulations for inducing enhanced interferon-gamma responses |
| RU2007106722A (en) * | 2004-07-22 | 2008-08-27 | Дженентек, Инк. (Us) | METHOD FOR TREATING SHEHREN'S SYNDROME |
| CN101087807A (en) * | 2004-10-05 | 2007-12-12 | 健泰科生物技术公司 | Method for treating vasculitis |
| MY159370A (en) * | 2004-10-20 | 2016-12-30 | Coley Pharm Group Inc | Semi-soft-class immunostimulatory oligonucleotides |
| ZA200705459B (en) * | 2005-01-13 | 2008-09-25 | Genentech Inc | Treatment method |
| US20060205753A1 (en) * | 2005-01-20 | 2006-09-14 | Israel Robert J | Use of methylnaltrexone and related compounds to treat post-operative gastrointestinal dysfunction |
| DOP2006000029A (en) * | 2005-02-07 | 2006-08-15 | Genentech Inc | ANTIBODY VARIANTS AND USES THEREOF. (VARIATIONS OF AN ANTIBODY AND USES OF THE SAME) |
| WO2006089133A2 (en) * | 2005-02-15 | 2006-08-24 | Duke University | Anti-cd19 antibodies and uses in oncology |
| CN101160401A (en) * | 2005-02-24 | 2008-04-09 | 科勒制药集团公司 | Immunostimulatory oligonucleotides |
| TW200714289A (en) * | 2005-02-28 | 2007-04-16 | Genentech Inc | Treatment of bone disorders |
| US9662325B2 (en) | 2005-03-07 | 2017-05-30 | The University Of Chicago | Use of opioid antagonists to attenuate endothelial cell proliferation and migration |
| US8518962B2 (en) | 2005-03-07 | 2013-08-27 | The University Of Chicago | Use of opioid antagonists |
| MX2007010833A (en) * | 2005-03-07 | 2009-02-17 | Univ Chicago | Use of opioid antagonists to attenuate endothelial cell proliferation and migration. |
| US8524731B2 (en) * | 2005-03-07 | 2013-09-03 | The University Of Chicago | Use of opioid antagonists to attenuate endothelial cell proliferation and migration |
| EP1874325A2 (en) * | 2005-04-08 | 2008-01-09 | Coley Pharmaceutical Group, Inc. | Methods for treating infectious disease exacerbated asthma |
| AR053579A1 (en) * | 2005-04-15 | 2007-05-09 | Genentech Inc | TREATMENT OF INTESTINAL INFLAMMATORY DISEASE (IBD) |
| US20060241076A1 (en) * | 2005-04-26 | 2006-10-26 | Coley Pharmaceutical Gmbh | Modified oligoribonucleotide analogs with enhanced immunostimulatory activity |
| EP2221316A1 (en) * | 2005-05-05 | 2010-08-25 | Duke University | Anti-CD19 antibody therapy for autoimmune disease |
| EP1902320B1 (en) * | 2005-05-20 | 2010-03-10 | Genentech, Inc. | Pretreatment of a biological sample from an autoimmune disease subject |
| AR057325A1 (en) * | 2005-05-25 | 2007-11-28 | Progenics Pharm Inc | SYNTHESIS OF (S) -N-METHYLNTREXONE, PHARMACEUTICAL COMPOSITIONS AND USES |
| AR057035A1 (en) * | 2005-05-25 | 2007-11-14 | Progenics Pharm Inc | SYNTHESIS OF (R) -N-METHYLNTREXONE, PHARMACEUTICAL COMPOSITIONS AND USES |
| US20080194611A1 (en) * | 2005-06-03 | 2008-08-14 | Alverdy John C | Modulation of Cell Barrier Dysfunction |
| NZ565311A (en) * | 2005-07-07 | 2009-10-30 | Pfizer | Anti-ctla-4 antibody and cpg-motif-containing synthetic oligodeoxynucleotide combination therapy for cancer treatment |
| NZ565173A (en) | 2005-07-25 | 2012-01-12 | Emergent Product Dev Seattle | Single dose use of CD20 scFv for rheumatoid arthritis |
| US20080279850A1 (en) * | 2005-07-25 | 2008-11-13 | Trubion Pharmaceuticals, Inc. | B-Cell Reduction Using CD37-Specific and CD20-Specific Binding Molecules |
| SI2298815T1 (en) | 2005-07-25 | 2015-08-31 | Emergent Product Development Seattle, Llc | B-cell reduction using CD37-specific and CD20-specific binding molecules |
| WO2007088423A2 (en) * | 2005-09-16 | 2007-08-09 | Coley Pharmaceutical Gmbh | Immunostimulatory single-stranded ribonucleic acid with phosphodiester backbone |
| EA013375B1 (en) * | 2005-09-16 | 2010-04-30 | Коли Фармасьютикал Гмбх | MODULATION OF IMMUNOSTIMULATORY PROPERTIES OF SHORT INTERFERING RIBONUCLEIC ACID (siRNA) BY NUCLEOTIDE MODIFICATION |
| GB0523041D0 (en) * | 2005-11-11 | 2005-12-21 | Cyclacel Ltd | Combination |
| MY149159A (en) | 2005-11-15 | 2013-07-31 | Hoffmann La Roche | Method for treating joint damage |
| ES2618543T3 (en) * | 2005-11-23 | 2017-06-21 | Genentech, Inc. | Methods and compositions related to B lymphocyte assays |
| DK1957647T3 (en) | 2005-11-25 | 2015-04-07 | Zoetis Belgium S A | Immunostimulatory oligoribonucleotides |
| EP2405002B1 (en) * | 2006-02-15 | 2014-09-24 | AdiuTide Pharmaceuticals GmbH | Compositions and methods for oligonucleotide formulations |
| CA3149553C (en) * | 2006-06-12 | 2023-11-21 | Aptevo Research And Development Llc | Single-chain multivalent binding proteins with effector function |
| US20080031887A1 (en) * | 2006-06-30 | 2008-02-07 | Joseph Lustgarten | Conjugates for inducing targeted immune responses and methods of making and using same |
| TW200817048A (en) * | 2006-09-08 | 2008-04-16 | Wyeth Corp | Dry powder compound formulations and uses thereof |
| MX2009003398A (en) | 2006-09-27 | 2009-08-12 | Coley Pharm Gmbh | Cpg oligonucleotide analogs containing hydrophobic t analogs with enhanced immunostimulatory activity. |
| US20090142362A1 (en) * | 2006-11-06 | 2009-06-04 | Avant Immunotherapeutics, Inc. | Peptide-based vaccine compositions to endogenous cholesteryl ester transfer protein (CETP) |
| DK2139890T3 (en) * | 2007-03-29 | 2014-08-25 | Wyeth Llc | PERIPHERAL OPIOID RECEPTOR ANTAGONISTS AND APPLICATIONS THEREOF |
| MX351611B (en) | 2007-03-29 | 2017-10-20 | Wyeth Llc | Crystal forms of (r) -n-methylnaltrexone bromide and uses thereof. |
| CA2682125C (en) * | 2007-03-29 | 2015-06-16 | Progenics Pharmaceuticals, Inc. | Peripheral opioid receptor antagonists and uses thereof |
| DK2573176T3 (en) * | 2007-05-04 | 2016-08-01 | Index Pharmaceuticals Ab | Tumor growth retardant compounds and methods of use thereof |
| EP2188302B1 (en) | 2007-07-09 | 2017-11-01 | Genentech, Inc. | Prevention of disulfide bond reduction during recombinant production of polypeptides |
| CA2699265A1 (en) * | 2007-09-13 | 2009-03-19 | Molecular Insight Pharmaceuticals, Inc. | Infusion and transfer system for use with radioactive agents |
| HUE030134T2 (en) | 2007-10-16 | 2017-04-28 | Zymogenetics Inc | Combination of transmembrane activator and calcium modulator and cyclophilin ligand interactor (TACI) and anti-CD20 agents for treatment of autoimmune disease |
| EP2077281A1 (en) | 2008-01-02 | 2009-07-08 | Bergen Teknologioverforing AS | Anti-CD20 antibodies or fragments thereof for the treatment of chronic fatigue syndrome |
| CN101959892B (en) | 2008-02-06 | 2014-01-08 | 普罗热尼奇制药公司 | Preparation and use of (R),(R)-2,2'-bis-methylnaltrexone |
| US8685995B2 (en) * | 2008-03-21 | 2014-04-01 | The University Of Chicago | Treatment with opioid antagonists and mTOR inhibitors |
| MX340204B (en) * | 2008-04-11 | 2016-06-30 | Emergent Product Dev Seattle | Cd37 immunotherapeutic and combination with bifunctional chemotherapeutic thereof. |
| WO2009131712A2 (en) | 2008-04-25 | 2009-10-29 | Duke University Medical Center | Regulatory b cells and their uses |
| TWI351288B (en) * | 2008-07-04 | 2011-11-01 | Univ Nat Pingtung Sci & Tech | Cpg dna adjuvant in avian vaccines |
| AU2009288730B2 (en) * | 2008-08-25 | 2013-06-20 | Amplimmune, Inc. | Compositions of PD-1 antagonists and methods of use |
| TW201014605A (en) | 2008-09-16 | 2010-04-16 | Genentech Inc | Methods for treating progressive multiple sclerosis |
| CA2676881C (en) | 2008-09-30 | 2017-04-25 | Wyeth | Peripheral opioid receptor antagonists and uses thereof |
| WO2010075249A2 (en) | 2008-12-22 | 2010-07-01 | Genentech, Inc. | A method for treating rheumatoid arthritis with b-cell antagonists |
| AU2010229835B2 (en) | 2009-03-25 | 2015-01-15 | The Board Of Regents Of The University Of Texas System | Compositions for stimulation of mammalian innate immune resistance to pathogens |
| WO2010132622A2 (en) * | 2009-05-14 | 2010-11-18 | The Regents Of The University Of California | Anticd20-cpg conjugates and methods of treating b cell malignancies |
| CN104059955A (en) | 2009-08-11 | 2014-09-24 | 弗·哈夫曼-拉罗切有限公司 | Production Of Proteins In Glutamine-free Cell Culture Media |
| CA2789629A1 (en) | 2010-02-10 | 2011-08-18 | Immunogen, Inc. | Cd20 antibodies and uses thereof |
| US20130224237A1 (en) * | 2010-07-20 | 2013-08-29 | University Of Miami | Inhibition of nonsense mediated decay pathways |
| US10131875B2 (en) | 2010-08-04 | 2018-11-20 | Duke University | Regulatory B cells and their uses |
| WO2012064671A1 (en) * | 2010-11-08 | 2012-05-18 | The Ohio State University Research Foundation | Compositions and methods for increasing drug efficacy in cancer |
| WO2012088272A1 (en) * | 2010-12-21 | 2012-06-28 | Duke University | Methods and compositions combining immunotherapy with monocyte activation |
| JP5930146B2 (en) * | 2011-03-28 | 2016-06-08 | 国立研究開発法人物質・材料研究機構 | Immunostimulatory oligonucleotide and therapeutic agent comprising said immunostimulatory oligonucleotide |
| US20130157261A1 (en) * | 2011-06-01 | 2013-06-20 | The Methodist Hospital Research Institute | Compositions and Methods for Quantitative Histology, Calibration of Images in Fluorescence Microscopy, and ddTUNEL Analyses |
| US10017739B2 (en) | 2012-09-06 | 2018-07-10 | Duke University | Methods of expanding and assessing B cells and using expanded B cells to treat disease |
| US10436680B2 (en) | 2013-10-15 | 2019-10-08 | Kianoosh Peyvan | Capture, disruption, and extraction apparatus and method |
| US10286065B2 (en) | 2014-09-19 | 2019-05-14 | Board Of Regents, The University Of Texas System | Compositions and methods for treating viral infections through stimulated innate immunity in combination with antiviral compounds |
| WO2017053469A2 (en) | 2015-09-21 | 2017-03-30 | Aptevo Research And Development Llc | Cd3 binding polypeptides |
| EP3356406A1 (en) | 2015-10-02 | 2018-08-08 | H. Hoffnabb-La Roche Ag | Bispecific anti-human cd20/human transferrin receptor antibodies and methods of use |
| AR106189A1 (en) | 2015-10-02 | 2017-12-20 | Hoffmann La Roche | BIESPECTIFIC ANTIBODIES AGAINST HUMAN A-b AND THE HUMAN TRANSFERRINE RECEIVER AND METHODS OF USE |
| CA3002073A1 (en) * | 2015-10-20 | 2017-04-27 | Sorrento Therapeutics, Inc. | Intracellular delivery compounds |
| US20190185852A1 (en) * | 2016-05-05 | 2019-06-20 | M. Mahmood Hussain | Therapeutically modulating apob and apoai |
| WO2018112407A1 (en) | 2016-12-15 | 2018-06-21 | Duke University | Antibodies and methods for depleting regulatory b10 cells and use in combination with immune checkpoint inhibitors |
| MX2019012295A (en) | 2017-04-14 | 2020-02-07 | Tollnine Inc | Immunomodulating polynucleotides, antibody conjugates thereof, and methods of their use. |
| CN111826764B (en) * | 2020-07-28 | 2021-10-15 | 吴忠德悦纺织科技有限公司 | Preparation method of modified multi-component composite yarn |
| CN114216985A (en) * | 2021-12-22 | 2022-03-22 | 珠海润都制药股份有限公司 | Method for testing diisopropyl sulfate in isosorbide |
Family Cites Families (90)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3854480A (en) | 1969-04-01 | 1974-12-17 | Alza Corp | Drug-delivery system |
| US3906092A (en) | 1971-11-26 | 1975-09-16 | Merck & Co Inc | Stimulation of antibody response |
| US4469863A (en) | 1980-11-12 | 1984-09-04 | Ts O Paul O P | Nonionic nucleic acid alkyl and aryl phosphonates and processes for manufacture and use thereof |
| US4675189A (en) | 1980-11-18 | 1987-06-23 | Syntex (U.S.A.) Inc. | Microencapsulation of water soluble active polypeptides |
| US5023243A (en) | 1981-10-23 | 1991-06-11 | Molecular Biosystems, Inc. | Oligonucleotide therapeutic agent and method of making same |
| US4452775A (en) | 1982-12-03 | 1984-06-05 | Syntex (U.S.A.) Inc. | Cholesterol matrix delivery system for sustained release of macromolecules |
| US5567610A (en) | 1986-09-04 | 1996-10-22 | Bioinvent International Ab | Method of producing human monoclonal antibodies and kit therefor |
| US5565354A (en) | 1986-09-05 | 1996-10-15 | Sandoz Ltd. | Production of human monoclonal antibodies specific for hepatitis B surface antigen |
| US5075109A (en) | 1986-10-24 | 1991-12-24 | Southern Research Institute | Method of potentiating an immune response |
| US6214804B1 (en) | 1989-03-21 | 2001-04-10 | Vical Incorporated | Induction of a protective immune response in a mammal by injecting a DNA sequence |
| US5133974A (en) | 1989-05-05 | 1992-07-28 | Kv Pharmaceutical Company | Extended release pharmaceutical formulations |
| US5786189A (en) | 1989-11-29 | 1998-07-28 | Smithkline Beecham Biologicals (S.A.) | Vaccine |
| US5506212A (en) | 1990-01-11 | 1996-04-09 | Isis Pharmaceuticals, Inc. | Oligonucleotides with substantially chirally pure phosphorothioate linkages |
| US5212295A (en) | 1990-01-11 | 1993-05-18 | Isis Pharmaceuticals | Monomers for preparation of oligonucleotides having chiral phosphorus linkages |
| US5248670A (en) | 1990-02-26 | 1993-09-28 | Isis Pharmaceuticals, Inc. | Antisense oligonucleotides for inhibiting herpesviruses |
| KR100272077B1 (en) | 1990-08-29 | 2000-11-15 | 젠팜인터내셔날,인코포레이티드 | Transgenic non-human animals capable of producing heterologous antibodies |
| US5208146A (en) * | 1990-11-05 | 1993-05-04 | The Regents Of The University Of California | Murine monoclonal anti-idiotype antibodies |
| US5512668A (en) | 1991-03-06 | 1996-04-30 | Polish Academy Of Sciences | Solid phase oligonucleotide synthesis using phospholane intermediates |
| US5359052A (en) | 1991-08-05 | 1994-10-25 | Polish Academy Of Sciences | Chalcophospholanes useful in the synthesis of oligonucleoside phosphorothioates, phosphorodithioates and related selenates |
| US5599797A (en) | 1991-10-15 | 1997-02-04 | Isis Pharmaceuticals, Inc. | Oligonucleotides having phosphorothioate linkages of high chiral purity |
| US5407686A (en) | 1991-11-27 | 1995-04-18 | Sidmak Laboratories, Inc. | Sustained release composition for oral administration of active ingredient |
| US5585479A (en) | 1992-07-24 | 1996-12-17 | The United States Of America As Represented By The Secretary Of The Navy | Antisense oligonucleotides directed against human ELAM-I RNA |
| US6015886A (en) | 1993-05-24 | 2000-01-18 | Chemgenes Corporation | Oligonucleotide phosphate esters |
| US5849719A (en) | 1993-08-26 | 1998-12-15 | The Regents Of The University Of California | Method for treating allergic lung disease |
| US5679647A (en) | 1993-08-26 | 1997-10-21 | The Regents Of The University Of California | Methods and devices for immunizing a host against tumor-associated antigens through administration of naked polynucleotides which encode tumor-associated antigenic peptides |
| IL111658A0 (en) | 1993-11-16 | 1995-01-24 | Genta Inc | Chirally enriched synthetic phosphonate oligomers |
| US6727230B1 (en) * | 1994-03-25 | 2004-04-27 | Coley Pharmaceutical Group, Inc. | Immune stimulation by phosphorothioate oligonucleotide analogs |
| WO1995026204A1 (en) | 1994-03-25 | 1995-10-05 | Isis Pharmaceuticals, Inc. | Immune stimulation by phosphorothioate oligonucleotide analogs |
| US5534615A (en) | 1994-04-25 | 1996-07-09 | Genentech, Inc. | Cardiac hypertrophy factor and uses therefor |
| US6239116B1 (en) * | 1994-07-15 | 2001-05-29 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| US6429199B1 (en) * | 1994-07-15 | 2002-08-06 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules for activating dendritic cells |
| ES2267100T5 (en) | 1994-07-15 | 2011-04-08 | The University Of Iowa Research Foundation | IMMUNOMODULATING OLIGONUCLEOTIDES. |
| US20030050263A1 (en) * | 1994-07-15 | 2003-03-13 | The University Of Iowa Research Foundation | Methods and products for treating HIV infection |
| US20030026782A1 (en) * | 1995-02-07 | 2003-02-06 | Arthur M. Krieg | Immunomodulatory oligonucleotides |
| US7935675B1 (en) * | 1994-07-15 | 2011-05-03 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| US6207646B1 (en) * | 1994-07-15 | 2001-03-27 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| US5736152A (en) | 1995-10-27 | 1998-04-07 | Atrix Laboratories, Inc. | Non-polymeric sustained release delivery system |
| US5969135A (en) * | 1995-11-02 | 1999-10-19 | Icn Pharmaceuticals, Inc. | Oligonucleotide analogs with an amino acid or a modified amino alcohol residue |
| US5780448A (en) | 1995-11-07 | 1998-07-14 | Ottawa Civic Hospital Loeb Research | DNA-based vaccination of fish |
| US5856465A (en) | 1996-05-24 | 1999-01-05 | Polska Akademia Nauk Centrum Badan Molekularnych I Makromolekularnych | Compositions and methods for the synthesis of chirally pure organophosphorus nucleoside derivatives |
| EP0855184A1 (en) * | 1997-01-23 | 1998-07-29 | Grayson B. Dr. Lipford | Pharmaceutical composition comprising a polynucleotide and an antigen especially for vaccination |
| AU738513B2 (en) | 1997-02-28 | 2001-09-20 | University Of Iowa Research Foundation, The | Use of nucleic acids containing unmethylated CpG dinucleotide in the treatment of LPS-associated disorders |
| EP1005368B1 (en) * | 1997-03-10 | 2009-09-02 | Ottawa Hospital Research Institute | Use of nucleic acids containing unmethylated CpG dinucleotide in combination with alum as adjuvants |
| US6406705B1 (en) * | 1997-03-10 | 2002-06-18 | University Of Iowa Research Foundation | Use of nucleic acids containing unmethylated CpG dinucleotide as an adjuvant |
| US6306393B1 (en) * | 1997-03-24 | 2001-10-23 | Immunomedics, Inc. | Immunotherapy of B-cell malignancies using anti-CD22 antibodies |
| US6183744B1 (en) * | 1997-03-24 | 2001-02-06 | Immunomedics, Inc. | Immunotherapy of B-cell malignancies using anti-CD22 antibodies |
| EP1003531B1 (en) * | 1997-05-20 | 2007-08-22 | Ottawa Health Research Institute | Processes for preparing nucleic acid constructs |
| US6221882B1 (en) | 1997-07-03 | 2001-04-24 | University Of Iowa Research Foundation | Methods for inhibiting immunostimulatory DNA associated responses |
| WO1999051259A2 (en) | 1998-04-03 | 1999-10-14 | University Of Iowa Research Foundation | Methods and products for stimulating the immune system using immunotherapeutic oligonucleotides and cytokines |
| NZ508650A (en) * | 1998-05-14 | 2003-05-30 | Coley Pharm Gmbh | Regulating hematopoiesis using unmethylated C and G CpG-oligonucleotides with a phosphorothioate modification |
| DE69932717T2 (en) | 1998-05-22 | 2007-08-09 | Ottawa Health Research Institute, Ottawa | METHODS AND PRODUCTS FOR INDUCING MUCOSAL IMMUNITY |
| NZ528199A (en) * | 1998-08-11 | 2005-06-24 | Idec Pharma Corp | Combination therapies for B-cell lyphomas comprising administration of anti-CD20 antibody |
| AU761844C (en) * | 1998-11-09 | 2004-09-23 | F. Hoffmann-La Roche Ag | Treatment of hematologic malignancies associated with circulating tumor cells using chimeric anti-CD20 antibody |
| JP2003519417A (en) * | 1999-06-23 | 2003-06-17 | データム・インコーポレイテツド | System and method for providing a trusted third party clock and a trusted local clock |
| AP2006003503A0 (en) * | 1999-09-25 | 2006-02-28 | Univ Iowa Res Found | Immunostimulatory nucleic acids. |
| US6949520B1 (en) * | 1999-09-27 | 2005-09-27 | Coley Pharmaceutical Group, Inc. | Methods related to immunostimulatory nucleic acid-induced interferon |
| AU3108001A (en) * | 2000-01-20 | 2001-12-24 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for inducing a th2 immune response |
| US7585847B2 (en) * | 2000-02-03 | 2009-09-08 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for the treatment of asthma and allergy |
| US20020156033A1 (en) * | 2000-03-03 | 2002-10-24 | Bratzler Robert L. | Immunostimulatory nucleic acids and cancer medicament combination therapy for the treatment of cancer |
| US20040131628A1 (en) * | 2000-03-08 | 2004-07-08 | Bratzler Robert L. | Nucleic acids for the treatment of disorders associated with microorganisms |
| US20020091097A1 (en) * | 2000-09-07 | 2002-07-11 | Bratzler Robert L. | Nucleic acids for the prevention and treatment of sexually transmitted diseases |
| WO2002022809A2 (en) * | 2000-09-15 | 2002-03-21 | Coley Pharmaceutical Gmbh | PROCESS FOR HIGH THROUGHPUT SCREENING OF CpG-BASED IMMUNO-AGONIST/ANTAGONIST |
| ES2307568T3 (en) * | 2000-12-08 | 2008-12-01 | Coley Pharmaceutical Gmbh | CPG TYPE NUCLEIC ACIDS AND SAME USE METHODS. |
| US20030055014A1 (en) * | 2000-12-14 | 2003-03-20 | Bratzler Robert L. | Inhibition of angiogenesis by nucleic acids |
| US20030050268A1 (en) * | 2001-03-29 | 2003-03-13 | Krieg Arthur M. | Immunostimulatory nucleic acid for treatment of non-allergic inflammatory diseases |
| WO2003012061A2 (en) * | 2001-08-01 | 2003-02-13 | Coley Pharmaceutical Gmbh | Methods and compositions relating to plasmacytoid dendritic cells |
| SI1446162T1 (en) * | 2001-08-17 | 2009-04-30 | Coley Pharm Gmbh | Combination motif immune stimulatory oligonucleotides with improved activity |
| CA2461315A1 (en) * | 2001-10-05 | 2003-04-17 | Coley Pharmaceutical Gmbh | Toll-like receptor 3 signaling agonists and antagonists |
| AU2002360278A1 (en) * | 2001-10-12 | 2003-11-11 | Coley Pharmaceutical Gmbh | Methods and products for enhancing immune responses using imidazoquinoline compounds |
| US8153141B2 (en) * | 2002-04-04 | 2012-04-10 | Coley Pharmaceutical Gmbh | Immunostimulatory G, U-containing oligoribonucleotides |
| US20040009949A1 (en) * | 2002-06-05 | 2004-01-15 | Coley Pharmaceutical Group, Inc. | Method for treating autoimmune or inflammatory diseases with combinations of inhibitory oligonucleotides and small molecule antagonists of immunostimulatory CpG nucleic acids |
| US7569553B2 (en) * | 2002-07-03 | 2009-08-04 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US7576066B2 (en) * | 2002-07-03 | 2009-08-18 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US7605138B2 (en) * | 2002-07-03 | 2009-10-20 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US7807803B2 (en) * | 2002-07-03 | 2010-10-05 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| US20040053880A1 (en) * | 2002-07-03 | 2004-03-18 | Coley Pharmaceutical Group, Inc. | Nucleic acid compositions for stimulating immune responses |
| AR040996A1 (en) * | 2002-08-19 | 2005-04-27 | Coley Pharm Group Inc | IMMUNE STIMULATING NUCLEIC ACIDS |
| MXPA05004588A (en) * | 2002-10-29 | 2005-12-14 | Coley Pharmaceutical Group Ltd | Use of cpg oligonucleotides in the treatment of hepatitis c virus infection. |
| AU2003300919A1 (en) * | 2002-12-11 | 2004-06-30 | Coley Pharmaceutical Gmbh | 5' cpg nucleic acids and methods of use |
| US20040235770A1 (en) | 2003-04-02 | 2004-11-25 | Coley Pharmaceutical Group, Ltd. | Immunostimulatory nucleic acid oil-in-water formulations and related methods of use |
| JP2007524615A (en) * | 2003-06-20 | 2007-08-30 | コーリー ファーマシューティカル ゲーエムベーハー | Low molecular weight Toll-like receptor (TLR) antagonist |
| CA2536139A1 (en) * | 2003-09-25 | 2005-04-07 | Coley Pharmaceutical Group, Inc. | Nucleic acid-lipophilic conjugates |
| US20050215501A1 (en) * | 2003-10-24 | 2005-09-29 | Coley Pharmaceutical Group, Inc. | Methods and products for enhancing epitope spreading |
| US20050239733A1 (en) * | 2003-10-31 | 2005-10-27 | Coley Pharmaceutical Gmbh | Sequence requirements for inhibitory oligonucleotides |
| US20050100983A1 (en) * | 2003-11-06 | 2005-05-12 | Coley Pharmaceutical Gmbh | Cell-free methods for identifying compounds that affect toll-like receptor 9 (TLR9) signaling |
| EP1730281A2 (en) * | 2004-04-02 | 2006-12-13 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for inducing il-10 responses |
| CA2574090A1 (en) * | 2004-07-18 | 2006-12-21 | Coley Pharmaceutical Group, Ltd. | Methods and compositions for inducing innate immune responses |
| MY159370A (en) * | 2004-10-20 | 2016-12-30 | Coley Pharm Group Inc | Semi-soft-class immunostimulatory oligonucleotides |
| CN101160401A (en) * | 2005-02-24 | 2008-04-09 | 科勒制药集团公司 | Immunostimulatory oligonucleotides |
| DK1957647T3 (en) * | 2005-11-25 | 2015-04-07 | Zoetis Belgium S A | Immunostimulatory oligoribonucleotides |
-
2001
- 2001-06-22 AU AU7013401A patent/AU7013401A/en active Pending
- 2001-06-22 AT AT01948684T patent/ATE440618T1/en active
- 2001-06-22 PT PT01948684T patent/PT1296714E/en unknown
- 2001-06-22 EP EP01948684A patent/EP1296714B1/en not_active Expired - Lifetime
- 2001-06-22 ES ES01948684T patent/ES2332444T3/en not_active Expired - Lifetime
- 2001-06-22 JP JP2002503327A patent/JP2003535907A/en active Pending
- 2001-06-22 US US09/888,326 patent/US7534772B2/en not_active Expired - Fee Related
- 2001-06-22 SI SI200130937T patent/SI1296714T1/en unknown
- 2001-06-22 WO PCT/US2001/020154 patent/WO2001097843A2/en active Application Filing
- 2001-06-22 AU AU2001270134A patent/AU2001270134B2/en not_active Revoked
- 2001-06-22 DK DK01948684T patent/DK1296714T3/en active
- 2001-06-22 DE DE60139689T patent/DE60139689D1/en not_active Expired - Lifetime
- 2001-06-22 CA CA2410371A patent/CA2410371C/en not_active Expired - Lifetime
-
2006
- 2006-09-15 AU AU2006216542A patent/AU2006216542B2/en not_active Expired
-
2009
- 2009-07-28 AU AU2009203061A patent/AU2009203061C1/en not_active Expired
- 2009-09-01 AU AU2009212978A patent/AU2009212978A1/en active Pending
Non-Patent Citations (9)
| Title |
|---|
| CHU RS ET AL., JEXP MED, vol. 186, 1997, pages 1623 - 31 |
| DAVIS HL ET AL., J IMMUNOL, vol. 160, 1998, pages 870 - 6 |
| HARTMANN G ET AL., J IMMUNOL, vol. 164, 2000, pages 944 - 53 |
| KRIEG AM ET AL., CURR TOP MICROBIOL IMMUNOL, vol. 247, 2000, pages 1 - 21 |
| KRIEG AM ET AL., PHARMACAL THER, vol. 84, 1999, pages 113 - 20 |
| LIPFORD GB ET AL., EUR J IMMUNOL, vol. 27, 1997, pages 2340 - 4 |
| ROMAN M ET AL., NAT MED, vol. 3, 1997, pages 849 - 54 |
| WAGNER H, ADV INZMUNOL, vol. 73, 1999, pages 329 - 68 |
| WEINER GJ ET AL., PROC NATL ACAD SCI USA, vol. 94, 1997, pages 10833 - 7 |
Cited By (82)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US8258106B2 (en) * | 1994-07-15 | 2012-09-04 | University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| EP1501359A2 (en) * | 2001-08-03 | 2005-02-02 | Celldex Therapeutics, Inc. | Compositions comprising immunostimulatory oligonucleotides and uses thereof to enhance fc receptor-mediated immunotherapies |
| EP1501359A4 (en) * | 2001-08-03 | 2007-04-18 | Celldex Therapeutics Inc | Compositions comprising immunostimulatory oligonucleotides and uses thereof to enhance fc receptor-mediated immunotherapies |
| US8834900B2 (en) | 2001-08-17 | 2014-09-16 | University Of Iowa Research Foundation | Combination motif immune stimulatory oligonucleotides with improved activity |
| EP1435987A4 (en) * | 2001-09-07 | 2005-11-23 | Univ Boston | Method and composition for treating immune complex associated disorders |
| EP1435987A1 (en) * | 2001-09-07 | 2004-07-14 | The Trustees of Boston University | Method and composition for treating immune complex associated disorders |
| US7709451B2 (en) | 2001-09-07 | 2010-05-04 | Trustees Of Boston University | Method and composition for treating immune complex associated disorders |
| US7741297B2 (en) | 2002-02-04 | 2010-06-22 | Oncothyreon Inc. | Immunostimulatory, covalently lipidated oligonucleotides |
| US8088388B2 (en) | 2002-02-14 | 2012-01-03 | United Biomedical, Inc. | Stabilized synthetic immunogen delivery system |
| US8084015B2 (en) * | 2002-02-14 | 2011-12-27 | United Biomedical, Inc. | Stabilized synthetic immunogen delivery system |
| SG166673A1 (en) * | 2002-08-19 | 2010-12-29 | Coley Pharm Group Inc | Immunostimulatory nucleic acids |
| US8304396B2 (en) | 2002-08-19 | 2012-11-06 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids |
| JP2014065735A (en) * | 2002-09-13 | 2014-04-17 | Lab Francais Du Fractionnement Et Des Biotechnologies | Treatment of pathologies which escape the immune response, using optimised antibodies |
| US8529902B2 (en) | 2002-10-17 | 2013-09-10 | Genmab A/S | Human monoclonal antibodies against CD20 |
| JP4754967B2 (en) * | 2002-11-06 | 2011-08-24 | セルジーン コーポレイション | Pharmaceutical composition for the treatment and management of brain tumors comprising 1-oxo-2- (2,6-dioxopiperidin-3-yl) -4-methylisoindoline |
| JP2006514689A (en) * | 2002-11-06 | 2006-05-11 | セルジーン・コーポレーション | Methods and compositions using immunomodulatory compounds for the treatment and management of cancer and other diseases |
| JPWO2004078764A1 (en) * | 2003-03-04 | 2006-06-08 | 株式会社そーせい | Antitumor effect potentiator comprising GM-95 substance, antitumor combination preparation and antitumor agent |
| US7875594B2 (en) * | 2003-05-16 | 2011-01-25 | Idera Pharmaceuticals, Inc. | Synergistic treatment of cancer using immunomers in conjunction with chemotherapeutic agents |
| JP2006528697A (en) * | 2003-05-16 | 2006-12-21 | イデラ ファーマシューティカルズ インコーポレイテッド | Synergistic treatment of cancer using immunomers in combination with chemotherapeutic agents |
| US7569554B2 (en) * | 2003-05-16 | 2009-08-04 | Idera Pharmaceuticals, Inc. | Synergistic treatment of cancer using immunomers in conjunction with therapeutic agents |
| JP2007509040A (en) * | 2003-10-11 | 2007-04-12 | イネックス ファーマシューティカルズ コーポレイション | Methods and compositions for enhancing innate immunity and antibody-dependent cytotoxicity |
| US9050378B2 (en) | 2003-12-10 | 2015-06-09 | Board Of Regents, The University Of Texas System | N2S2 chelate-targeting ligand conjugates |
| WO2005111057A3 (en) * | 2004-04-02 | 2006-07-27 | Coley Pharm Group Inc | Immunostimulatory nucleic acids for inducing il-10 responses |
| WO2005111057A2 (en) * | 2004-04-02 | 2005-11-24 | Coley Pharmaceutical Group, Inc. | Immunostimulatory nucleic acids for inducing il-10 responses |
| US7850962B2 (en) | 2004-04-20 | 2010-12-14 | Genmab A/S | Human monoclonal antibodies against CD20 |
| EP1809671A4 (en) * | 2004-11-09 | 2009-02-25 | Univ Southern California | Targeted innate immunity |
| US9522958B2 (en) | 2004-11-09 | 2016-12-20 | University Of Southern California | Cancer targeted innate immunity |
| EP1809671A2 (en) * | 2004-11-09 | 2007-07-25 | University Of Southern California | Targeted innate immunity |
| US9260530B2 (en) | 2005-02-15 | 2016-02-16 | Duke University | Anti-CD19 antibodies and uses in B cell disorders |
| US8444973B2 (en) | 2005-02-15 | 2013-05-21 | Duke University | Anti-CD19 antibodies and uses in B cell disorders |
| EP1859793A4 (en) * | 2005-02-28 | 2008-07-23 | Eisai R&D Man Co Ltd | Novel combinational use of sulfonamide compound |
| EP1859793A1 (en) * | 2005-02-28 | 2007-11-28 | Eisai R&D Management Co., Ltd. | Novel combinational use of sulfonamide compound |
| US8450292B2 (en) | 2005-05-17 | 2013-05-28 | Changchun Huapu Biotechnology Co., Ltd. | Oligonucleotides or their functional homologues, a composition comprising the same and a method of treating B cell neoplasm |
| EP1883411A1 (en) * | 2005-05-17 | 2008-02-06 | Changchun Huapu Biotechnology Co., Ltd. | An oligonucleotide or its functional homologue, a composition comprising the same and a method for treating b cell neoplasm |
| AU2006246897B2 (en) * | 2005-05-17 | 2012-04-12 | Changchun Huapu Biotechnology Co., Ltd. | Oligonucleotides or their functional homologues, a composition comprising the same and a method of treating B cell neoplasm |
| EP1883647A1 (en) * | 2005-05-17 | 2008-02-06 | Changchun Huapu Biotechnology Co., Ltd. | Oligonucleotides or their functional homologues, a composition comprising the same and a method of treating b cell neoplasm |
| EP1883647A4 (en) * | 2005-05-17 | 2010-10-06 | Changchun Huapu Biotechnology | Oligonucleotides or their functional homologues, a composition comprising the same and a method of treating b cell neoplasm |
| EP1883411A4 (en) * | 2005-05-17 | 2010-10-06 | Changchun Huapu Biotechnology | An oligonucleotide or its functional homologue, a composition comprising the same and a method for treating b cell neoplasm |
| US8133874B2 (en) | 2005-05-17 | 2012-03-13 | Changchun Huapu Biotechnology Co., Ltd. | Oligonucleotide or its functional homologue, a composition comprising the same and a method of treating B cell neoplasm |
| KR101294131B1 (en) | 2005-05-17 | 2013-08-07 | 창춘 후아푸 바이오테크놀로지 씨오., 엘티디. | An oligonucleotide or its functional homologue, a composition comprising the same and a method for treating b cell neoplasm |
| US8569257B2 (en) | 2005-07-01 | 2013-10-29 | Index Pharmaceuticals Ab | Method for modulating responsiveness to steroids |
| US8148341B2 (en) | 2005-07-01 | 2012-04-03 | Index Pharmaceuticals Ab | Method for modulating responsiveness to steroids |
| US8258107B2 (en) | 2005-07-01 | 2012-09-04 | Index Pharmaceuticals Ab | Immunostimulatory method |
| US8592390B2 (en) | 2005-07-01 | 2013-11-26 | Index Pharmaceuticals Ab | Immunostimulatory method |
| US8895522B2 (en) | 2005-10-28 | 2014-11-25 | Index Pharmaceuticals Ab | Composition and method for the prevention, treatment and/or alleviation of an inflammatory disease |
| WO2008014979A3 (en) * | 2006-07-31 | 2008-05-02 | Curevac Gmbh | NUCLEIC ACID OF FORMULA (I): GIXmGn, OR (II): CIXmCn, IN PARTICULAR AS AN IMMUNE-STIMULATING AGENT/ADJUVANT |
| EP2650368A1 (en) * | 2006-07-31 | 2013-10-16 | CureVac GmbH | Nucleic acid of formula (I): GlXmGn, or (II): ClXmCn, in particular as an immune-stimulating agent/adjuvant |
| WO2008014979A2 (en) * | 2006-07-31 | 2008-02-07 | Curevac Gmbh | NUCLEIC ACID OF FORMULA (I): GIXmGn, OR (II): CIXmCn, IN PARTICULAR AS AN IMMUNE-STIMULATING AGENT/ADJUVANT |
| US10441653B2 (en) | 2006-07-31 | 2019-10-15 | Curevac Ag | Nucleic acid comprising GlXmGn as an immune-stimulating agent/adjuvant |
| AU2007280690C1 (en) * | 2006-07-31 | 2012-08-23 | Curevac Gmbh | Nucleic acid of formula (I): GIXmGn, or (II): CIXmCn, in particular as an immune-stimulating agent/adjuvant |
| AU2007280690B2 (en) * | 2006-07-31 | 2012-04-05 | Curevac Gmbh | Nucleic acid of formula (I): GIXmGn, or (II): CIXmCn, in particular as an immune-stimulating agent/adjuvant |
| US10626182B2 (en) | 2006-08-14 | 2020-04-21 | Xencor, Inc. | Optimized antibodies that target CD19 |
| US11618788B2 (en) | 2006-08-14 | 2023-04-04 | Xencor, Inc. | Optimized antibodies that target CD19 |
| US8524867B2 (en) | 2006-08-14 | 2013-09-03 | Xencor, Inc. | Optimized antibodies that target CD19 |
| US9803020B2 (en) | 2006-08-14 | 2017-10-31 | Xencor, Inc. | Optimized antibodies that target CD19 |
| US10925977B2 (en) | 2006-10-05 | 2021-02-23 | Ceil>Point, LLC | Efficient synthesis of chelators for nuclear imaging and radiotherapy: compositions and applications |
| US10814013B2 (en) | 2006-10-05 | 2020-10-27 | The Board Of Regents Of The University Of Texas System | Efficient synthesis of chelators for nuclear imaging and radiotherapy: compositions and applications |
| US8349792B2 (en) | 2006-12-19 | 2013-01-08 | Cyclacel Limited | Combination comprising CNDAC (2′-cyano-2′-deoxy-N4-palmitoyl-1-beta-D-arabinofuranosyl-cytosine) and a cytotoxic agent |
| WO2008132500A3 (en) * | 2007-04-27 | 2009-08-06 | Astrazeneca Ab | Chkl inhibitors with b cell depleting antibodies for the treatment of hematologic malignancies |
| WO2008132500A2 (en) * | 2007-04-27 | 2008-11-06 | Astrazeneca Ab | Chkl inhibitors with b cell depleting antibodies for the treatment of hematologic malignancies |
| US10111967B2 (en) | 2007-09-04 | 2018-10-30 | Curevac Ag | Complexes of RNA and cationic peptides for transfection and for immunostimulation |
| US9226959B2 (en) | 2008-01-31 | 2016-01-05 | Curevac Ag | Nucleic acids comprising formula (NuGlXmGnNv)a and derivatives thereof as immunostimulating agent/adjuvant |
| US8975239B2 (en) | 2008-06-09 | 2015-03-10 | Cyclacel Limited | Combinations of sapacitabine or CNDAC with DNA methyltransferase inhibitors such as decitabine and procaine |
| US8530445B2 (en) | 2008-06-09 | 2013-09-10 | Cyclacel Limited | Combinations of sapacitabine or CNDAC with DNA methyltransferase inhibitors such as decitabine and procaine |
| WO2009154565A1 (en) * | 2008-06-18 | 2009-12-23 | Index Pharmaceuticals Ab | Combination therapies against cancer |
| US9572874B2 (en) | 2008-09-30 | 2017-02-21 | Curevac Ag | Composition comprising a complexed (M)RNA and a naked mRNA for providing or enhancing an immunostimulatory response in a mammal and uses thereof |
| WO2010053433A1 (en) * | 2008-11-04 | 2010-05-14 | Index Pharmaceuticals Ab | Increased expression of specific antigens |
| US9314535B2 (en) | 2009-09-03 | 2016-04-19 | Curevac Ag | Disulfide-linked polyethyleneglycol/peptide conjugates for the transfection of nucleic acids |
| US9907862B2 (en) | 2009-09-03 | 2018-03-06 | Curevac Ag | Disulfide-linked polyethyleneglycol/peptide conjugates for the transfection of nucleic acids |
| US10751424B2 (en) | 2009-09-03 | 2020-08-25 | Curevac Ag | Disulfide-linked polyethyleneglycol/peptide conjugates for the transfection of nucleic acids |
| US8968746B2 (en) | 2010-07-30 | 2015-03-03 | Curevac Gmbh | Complexation of nucleic acids with disulfide-crosslinked cationic components for transfection and immunostimulation |
| US10226478B2 (en) | 2011-04-14 | 2019-03-12 | Cyclacel Limited | Dosage regimen for sapacitabine and decitabine in combination for treating acute myeloid leukemia |
| US11690910B2 (en) | 2012-01-31 | 2023-07-04 | CureVac SE | Pharmaceutical composition comprising a polymeric carrier cargo complex and at least one protein or peptide antigen |
| US11739125B2 (en) | 2013-08-21 | 2023-08-29 | Cure Vac SE | Respiratory syncytial virus (RSV) vaccine |
| EP3096787A4 (en) * | 2014-01-22 | 2018-02-07 | The Board of Trustees of the Leland Stanford Junior University | Methods and compositions for antibody and antibody-loaded dendritic cell mediated therapy |
| AU2015209277B2 (en) * | 2014-01-22 | 2020-09-03 | The Board Of Trustees Of The Leland Stanford Junior University | Methods and compositions for antibody and antibody-loaded dendritic cell mediated therapy |
| US11110166B2 (en) | 2014-04-01 | 2021-09-07 | Curevac Ag | Polymeric carrier cargo complex for use as an immunostimulating agent or as an adjuvant |
| US10369216B2 (en) | 2014-04-01 | 2019-08-06 | Curevac Ag | Polymeric carrier cargo complex for use as an immunostimulating agent or as an adjuvant |
| US11110178B2 (en) | 2016-07-07 | 2021-09-07 | The Board Of Trustees Of The Leland Standford Junior University | Antibody adjuvant conjugates |
| US11547761B1 (en) | 2016-07-07 | 2023-01-10 | The Board Of Trustees Of The Leland Stanford Junior University | Antibody adjuvant conjugates |
| US10675358B2 (en) | 2016-07-07 | 2020-06-09 | The Board Of Trustees Of The Leland Stanford Junior University | Antibody adjuvant conjugates |
| US11400164B2 (en) | 2019-03-15 | 2022-08-02 | Bolt Biotherapeutics, Inc. | Immunoconjugates targeting HER2 |
Also Published As
| Publication number | Publication date |
|---|---|
| AU2009212978A1 (en) | 2009-10-01 |
| AU2001270134B2 (en) | 2006-06-15 |
| CA2410371C (en) | 2015-11-17 |
| AU2009203061A1 (en) | 2009-08-20 |
| AU2009203061B2 (en) | 2012-02-23 |
| US7534772B2 (en) | 2009-05-19 |
| AU2006216542A1 (en) | 2006-10-12 |
| AU7013401A (en) | 2002-01-02 |
| DE60139689D1 (en) | 2009-10-08 |
| ATE440618T1 (en) | 2009-09-15 |
| US20030026801A1 (en) | 2003-02-06 |
| SI1296714T1 (en) | 2010-01-29 |
| DK1296714T3 (en) | 2009-12-07 |
| WO2001097843A3 (en) | 2003-01-23 |
| EP1296714A2 (en) | 2003-04-02 |
| AU2006216542B2 (en) | 2009-04-30 |
| ES2332444T3 (en) | 2010-02-05 |
| AU2009203061C1 (en) | 2012-06-28 |
| EP1296714B1 (en) | 2009-08-26 |
| CA2410371A1 (en) | 2001-12-27 |
| PT1296714E (en) | 2009-10-15 |
| JP2003535907A (en) | 2003-12-02 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| AU2009203061C1 (en) | Methods for enhancing antibody-induced cell lysis and treating cancer | |
| AU2001270134A1 (en) | Methods for enhancing antibody-induced cell lysis and treating cancer | |
| US20200101102A1 (en) | Treatment of cancer using tlr9 agonist with checkpoint inhibitors | |
| JP7236483B2 (en) | Combination of PD-1 antagonists and CpG-C type oligonucleotides for the treatment of cancer | |
| US20060211639A1 (en) | Immunostimulatory nucleic acids and cancer medicament combination therapy for the treatment of cancer | |
| JP2009500412A (en) | Combination therapy of anti-CTLA-4 antibody and CPG motif-containing synthetic oligodeoxynucleotide for the treatment of cancer | |
| US20110293565A1 (en) | Novel synthetic agonists of tlr9 | |
| WO2018192505A1 (en) | Immunomodulatory polynucleotides and uses thereof | |
| JP2022515188A (en) | Compositions and Methods for Cancer Treatment | |
| US20220175763A1 (en) | Compositions and methods for enhancing cancer immune checkpoint therapy | |
| US20230203504A1 (en) | Immunomodulatory polynucleotides and uses thereof |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| AK | Designated states |
Kind code of ref document: A2 Designated state(s): AE AG AL AM AT AU AZ BA BB BG BR BY BZ CA CH CN CO CR CU CZ DE DK DM DZ EC EE ES FI GB GD GE GH GM HR HU ID IL IN IS JP KE KG KP KR KZ LC LK LR LS LT LU LV MA MD MG MK MN MW MX MZ NO NZ PL PT RO RU SD SE SG SI SK SL TJ TM TR TT TZ UA UG UZ VN YU ZA ZW |
|
| AL | Designated countries for regional patents |
Kind code of ref document: A2 Designated state(s): GH GM KE LS MW MZ SD SL SZ TZ UG ZW AM AZ BY KG KZ MD RU TJ TM AT BE CH CY DE DK ES FI FR GB GR IE IT LU MC NL PT SE TR BF BJ CF CG CI CM GA GN GW ML MR NE SN TD TG |
|
| DFPE | Request for preliminary examination filed prior to expiration of 19th month from priority date (pct application filed before 20040101) | ||
| 121 | Ep: the epo has been informed by wipo that ep was designated in this application | ||
| WWE | Wipo information: entry into national phase |
Ref document number: 2410371 Country of ref document: CA |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2001270134 Country of ref document: AU |
|
| ENP | Entry into the national phase |
Ref country code: JP Ref document number: 2002 503327 Kind code of ref document: A Format of ref document f/p: F |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2001948684 Country of ref document: EP |
|
| WWP | Wipo information: published in national office |
Ref document number: 2001948684 Country of ref document: EP |
|
| REG | Reference to national code |
Ref country code: DE Ref legal event code: 8642 |