US8637640B2 - Blood coagulation protein conjugates - Google Patents
Blood coagulation protein conjugates Download PDFInfo
- Publication number
- US8637640B2 US8637640B2 US12/843,542 US84354210A US8637640B2 US 8637640 B2 US8637640 B2 US 8637640B2 US 84354210 A US84354210 A US 84354210A US 8637640 B2 US8637640 B2 US 8637640B2
- Authority
- US
- United States
- Prior art keywords
- blood coagulation
- coagulation protein
- psa
- protein
- aminooxy
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Active, expires
Links
- DZEJMPNILLCRBD-UHFFFAOYSA-N NOCCOCCOCCOCCON Chemical compound NOCCOCCOCCOCCON DZEJMPNILLCRBD-UHFFFAOYSA-N 0.000 description 4
- ZESQVNWRUDEXNZ-UHFFFAOYSA-N NOCCOCCON Chemical compound NOCCOCCON ZESQVNWRUDEXNZ-UHFFFAOYSA-N 0.000 description 4
- IXDINHMYXQVMAD-UHFFFAOYSA-N C=CC.C=CC(C)(=O)(OC(C)=O)ON1C(=O)CCC1=O.CC(C)C(=O)ON1C(=O)CCC1=O.CCC(=O)ON1C(=O)CCC1=O Chemical compound C=CC.C=CC(C)(=O)(OC(C)=O)ON1C(=O)CCC1=O.CC(C)C(=O)ON1C(=O)CCC1=O.CCC(=O)ON1C(=O)CCC1=O IXDINHMYXQVMAD-UHFFFAOYSA-N 0.000 description 1
- XMFKFYVREMCLFK-UHFFFAOYSA-N CC(=O)CCC(=O)ON1C(=O)CCC1=O.CC(=O)CCCC(=O)ON1C(=O)CCC1=O.CCC(=O)ON1C(=O)CCC1=O.CCCCCCC(=O)ON1C(=O)CCC1=O.CCN1C(=O)CCC1=O Chemical compound CC(=O)CCC(=O)ON1C(=O)CCC1=O.CC(=O)CCCC(=O)ON1C(=O)CCC1=O.CCC(=O)ON1C(=O)CCC1=O.CCCCCCC(=O)ON1C(=O)CCC1=O.CCN1C(=O)CCC1=O XMFKFYVREMCLFK-UHFFFAOYSA-N 0.000 description 1
- FHNMAOLQZHUPIJ-UHFFFAOYSA-N CC(C)C(=O)ON1C(=O)CCC1=O Chemical compound CC(C)C(=O)ON1C(=O)CCC1=O FHNMAOLQZHUPIJ-UHFFFAOYSA-N 0.000 description 1
- LYKBIMNJPFCHCY-UHFFFAOYSA-N CCCOCC(COC(=O)CCCC(=O)ON1C(=O)CCC1=O)OCCC Chemical compound CCCOCC(COC(=O)CCCC(=O)ON1C(=O)CCC1=O)OCCC LYKBIMNJPFCHCY-UHFFFAOYSA-N 0.000 description 1
- FGWMKAWTYWONHC-UHFFFAOYSA-N NOCCOCCOCCOCCOCCOCCON Chemical compound NOCCOCCOCCOCCOCCOCCON FGWMKAWTYWONHC-UHFFFAOYSA-N 0.000 description 1
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/36—Blood coagulation or fibrinolysis factors
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12N—MICROORGANISMS OR ENZYMES; COMPOSITIONS THEREOF; PROPAGATING, PRESERVING, OR MAINTAINING MICROORGANISMS; MUTATION OR GENETIC ENGINEERING; CULTURE MEDIA
- C12N9/00—Enzymes; Proenzymes; Compositions thereof; Processes for preparing, activating, inhibiting, separating or purifying enzymes
- C12N9/96—Stabilising an enzyme by forming an adduct or a composition; Forming enzyme conjugates
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/36—Blood coagulation or fibrinolysis factors
- A61K38/37—Factors VIII
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/43—Enzymes; Proenzymes; Derivatives thereof
- A61K38/46—Hydrolases (3)
- A61K38/48—Hydrolases (3) acting on peptide bonds (3.4)
- A61K38/482—Serine endopeptidases (3.4.21)
- A61K38/4846—Factor VII (3.4.21.21); Factor IX (3.4.21.22); Factor Xa (3.4.21.6); Factor XI (3.4.21.27); Factor XII (3.4.21.38)
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/50—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates
- A61K47/51—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent
- A61K47/56—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent the modifying agent being an organic macromolecular compound, e.g. an oligomeric, polymeric or dendrimeric molecule
- A61K47/59—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent the modifying agent being an organic macromolecular compound, e.g. an oligomeric, polymeric or dendrimeric molecule obtained otherwise than by reactions only involving carbon-to-carbon unsaturated bonds, e.g. polyureas or polyurethanes
- A61K47/60—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent the modifying agent being an organic macromolecular compound, e.g. an oligomeric, polymeric or dendrimeric molecule obtained otherwise than by reactions only involving carbon-to-carbon unsaturated bonds, e.g. polyureas or polyurethanes the organic macromolecular compound being a polyoxyalkylene oligomer, polymer or dendrimer, e.g. PEG, PPG, PEO or polyglycerol
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/50—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates
- A61K47/51—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent
- A61K47/56—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent the modifying agent being an organic macromolecular compound, e.g. an oligomeric, polymeric or dendrimeric molecule
- A61K47/61—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent the modifying agent being an organic macromolecular compound, e.g. an oligomeric, polymeric or dendrimeric molecule the organic macromolecular compound being a polysaccharide or a derivative thereof
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P43/00—Drugs for specific purposes, not provided for in groups A61P1/00-A61P41/00
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P7/00—Drugs for disorders of the blood or the extracellular fluid
- A61P7/04—Antihaemorrhagics; Procoagulants; Haemostatic agents; Antifibrinolytic agents
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K1/00—General methods for the preparation of peptides, i.e. processes for the organic chemical preparation of peptides or proteins of any length
- C07K1/107—General methods for the preparation of peptides, i.e. processes for the organic chemical preparation of peptides or proteins of any length by chemical modification of precursor peptides
-
- C—CHEMISTRY; METALLURGY
- C08—ORGANIC MACROMOLECULAR COMPOUNDS; THEIR PREPARATION OR CHEMICAL WORKING-UP; COMPOSITIONS BASED THEREON
- C08B—POLYSACCHARIDES; DERIVATIVES THEREOF
- C08B37/00—Preparation of polysaccharides not provided for in groups C08B1/00 - C08B35/00; Derivatives thereof
- C08B37/0006—Homoglycans, i.e. polysaccharides having a main chain consisting of one single sugar, e.g. colominic acid
-
- C—CHEMISTRY; METALLURGY
- C08—ORGANIC MACROMOLECULAR COMPOUNDS; THEIR PREPARATION OR CHEMICAL WORKING-UP; COMPOSITIONS BASED THEREON
- C08J—WORKING-UP; GENERAL PROCESSES OF COMPOUNDING; AFTER-TREATMENT NOT COVERED BY SUBCLASSES C08B, C08C, C08F, C08G or C08H
- C08J7/00—Chemical treatment or coating of shaped articles made of macromolecular substances
- C08J7/12—Chemical modification
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12N—MICROORGANISMS OR ENZYMES; COMPOSITIONS THEREOF; PROPAGATING, PRESERVING, OR MAINTAINING MICROORGANISMS; MUTATION OR GENETIC ENGINEERING; CULTURE MEDIA
- C12N9/00—Enzymes; Proenzymes; Compositions thereof; Processes for preparing, activating, inhibiting, separating or purifying enzymes
- C12N9/14—Hydrolases (3)
- C12N9/48—Hydrolases (3) acting on peptide bonds (3.4)
- C12N9/50—Proteinases, e.g. Endopeptidases (3.4.21-3.4.25)
- C12N9/64—Proteinases, e.g. Endopeptidases (3.4.21-3.4.25) derived from animal tissue
- C12N9/6421—Proteinases, e.g. Endopeptidases (3.4.21-3.4.25) derived from animal tissue from mammals
- C12N9/6424—Serine endopeptidases (3.4.21)
- C12N9/6437—Coagulation factor VIIa (3.4.21.21)
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12N—MICROORGANISMS OR ENZYMES; COMPOSITIONS THEREOF; PROPAGATING, PRESERVING, OR MAINTAINING MICROORGANISMS; MUTATION OR GENETIC ENGINEERING; CULTURE MEDIA
- C12N9/00—Enzymes; Proenzymes; Compositions thereof; Processes for preparing, activating, inhibiting, separating or purifying enzymes
- C12N9/14—Hydrolases (3)
- C12N9/48—Hydrolases (3) acting on peptide bonds (3.4)
- C12N9/50—Proteinases, e.g. Endopeptidases (3.4.21-3.4.25)
- C12N9/64—Proteinases, e.g. Endopeptidases (3.4.21-3.4.25) derived from animal tissue
- C12N9/6421—Proteinases, e.g. Endopeptidases (3.4.21-3.4.25) derived from animal tissue from mammals
- C12N9/6424—Serine endopeptidases (3.4.21)
- C12N9/644—Coagulation factor IXa (3.4.21.22)
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12Y—ENZYMES
- C12Y304/00—Hydrolases acting on peptide bonds, i.e. peptidases (3.4)
- C12Y304/21—Serine endopeptidases (3.4.21)
- C12Y304/21021—Coagulation factor VIIa (3.4.21.21)
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12Y—ENZYMES
- C12Y304/00—Hydrolases acting on peptide bonds, i.e. peptidases (3.4)
- C12Y304/21—Serine endopeptidases (3.4.21)
- C12Y304/21022—Coagulation factor IXa (3.4.21.22)
Definitions
- the present invention relates to materials and methods for conjugating a water soluble polymer to a blood coagulation protein.
- Therapeutic polypeptides such as blood coagulation proteins including Factor IX (FIX), Factor VIII (FVIII), Factor VIIa (FVIIa), Von Willebrand Factor (VWF), Factor FV (FV), Factor X (FX), Factor XI (FXI), Factor XII (FXII), thrombin (FII), protein C, protein S, tPA, PAI-1, tissue factor (TF) and ADAMTS 13 protease are rapidly degraded by proteolytic enzymes and neutralized by antibodies. This reduces their half-life and circulation time, thereby limiting their therapeutic effectiveness. Relatively high doses and frequent administration are necessary to reach and sustain the desired therapeutic or prophylactic effect of these coagulation proteins. As a consequence, adequate dose regulation is difficult to obtain and the need of frequent intravenous administrations imposes restrictions on the patient's way of living.
- PEGylation of polypeptide drugs protects them in circulation and improves their pharmacodynamic and pharmacokinetic profiles (Harris and Chess, Nat Rev Drug Discov. 2003; 2:214-21).
- the PEGylation process attaches repeating units of ethylene glycol (polyethylene glycol (PEG)) to a polypeptide drug.
- PEG molecules have a large hydrodynamic volume (5-10 times the size of globular proteins), are highly water soluble and hydrated, non-toxic, non-immunogenic and rapidly cleared from the body.
- PEGylation of molecules can lead to increased resistance of drugs to enzymatic degradation, increased half-life in vivo, reduced dosing frequency, decreased immunogenicity, increased physical and thermal stability, increased solubility, increased liquid stability, and reduced aggregation.
- the first PEGylated drugs were approved by the FDA in the early 1990s. Since then, the FDA has approved several PEGylated drugs for oral, injectable, and topical administration.
- PSA Polysialic acid
- CA colominic acid
- PSA acid is biodegradable.
- the preparation of conjugates by forming a covalent linkage between the water soluble polymer and the therapeutic protein can be carried out by a variety of chemical methods. For example, coupling of PEG-derivatives to peptides or proteins is reviewed by Roberts et al. (Adv Drug Deliv Rev 2002; 54:459-76).
- One approach for coupling water soluble polymers to therapeutic proteins is the conjugation of the polymers via the carbohydrate moieties of the protein.
- Vicinal hydroxyl (OH) groups of carbohydrates in proteins can be easily oxidized with sodium periodate (NaIO4) to form active aldehyde groups (Rothfus et Smith, J Biol Chem 1963; 238:1402-10; van Lenten et Ashwell, J Biol Chem 1971; 246:1889-94). Subsequently the polymer can be coupled to the aldehyde groups of the carbohydrate by use of reagents containing, for example, an active hydrazide group (Wilchek M and Bayer E A, Methods Enzymol 1987; 138:429-42). A more recent technology is the use of reagents containing aminooxy groups which react with aldehydes to form oxime linkages (WO 96/40662, WO2008/025856).
- the present invention provides materials and methods for conjugating polymers to proteins that improves the protein's pharmacodynamic and/or pharmacokinetic properties while minimizing the costs associated with the various reagents.
- a method of conjugating a water soluble polymer to an oxidized carbohydrate moiety of a blood coagulation protein comprising contacting the oxidized carbohydrate moiety with an activated water soluble polymer under conditions that allow conjugation; the blood coagulation protein selected from the group consisting of Factor IX (FIX), Factor VIII (FVIII), Factor VIIa (FVIIa), Von Willebrand Factor (VWF), Factor FV (FV), Factor X (FX), Factor XI (FXI), Factor XII (FXII), thrombin (FII), protein C, protein S, tPA, PAI-1, tissue factor (TF) and ADAMTS 13 protease or a biologically active fragment, derivative or variant thereof; the water soluble polymer containing an active aminooxy group and is selected from the group consisting of polyethylene glycol (PEG), branched PEG, polysialic acid (PSA), carbohydrate,
- PEG polyethylene
- the water soluble polymer according to the aforementioned method is PSA.
- the PSA is comprised of about 5-500 or 10-300 sialic acid units.
- the blood coagulation protein according to the aforementioned method is FIX.
- the blood coagulation protein according to the aforementioned method is FVIIa.
- the blood coagulation protein according to the aforementioned method is FVIII.
- the aforementioned method is provided wherein the oxidizing agent is sodium periodate (NaIO4).
- the oxidized carbohydrate moiety of the blood coagulation protein according to the aforementioned method is located in the activation peptide of the blood coagulation protein.
- the aforementioned method is provided wherein the PSA is prepared by reacting an activated aminooxy linker with oxidized PSA;
- the PSA is oxidized by incubation with a oxidizing agent to form a terminal aldehyde group at the non-reducing end of the PSA.
- the activated aminooxy linker comprises 1-50 ethylene glycol units.
- an aforementioned method is provided wherein the aminooxy linker is 3-oxa-pentane-1,5-dioxyamine.
- the oxidizing agent is NaIO 4 .
- the aforementioned method wherein the contacting of the oxidized carbohydrate moiety with the activated water soluble polymer occurs in a buffer comprising a nucleophilic catalyst selected from the group consisting of aniline and aniline derivatives.
- an aforementioned method further comprising the step of reducing an oxime linkage in the conjugated blood coagulation protein by incubating the conjugated blood coagulation protein in a buffer comprising a reducing compound selected from the group consisting of sodium cyanoborohydride (NaCNBH3) and ascorbic acid (vitamin C).
- a reducing compound selected from the group consisting of sodium cyanoborohydride (NaCNBH3) and ascorbic acid (vitamin C).
- the reducing compound is sodium cyanoborohydride (NaCNBH3).
- a modified blood coagulation protein produced by an aforementioned method is provided.
- a modified FIX comprising a FIX molecule or a biologically active fragment, derivative or variant thereof; and at least one aminooxy PSA bound to the FIX molecule, wherein said aminooxy PSA is attached to the FIX via one or more carbohydrate moieties.
- a modified FVIIa comprising a FVIIa molecule or a biologically active fragment, derivative or variant thereof; and at least one aminooxy PSA bound to the FVIIa molecule, wherein said aminooxy PSA is attached to the FVIIa via one or more carbohydrate moieties.
- a modified FVIII comprising a FVIII molecule or a biologically active fragment, derivative or variant thereof; and at least one aminooxy PSA bound to the FVIII molecule, wherein said aminooxy PSA is attached to the FVIII via one or more carbohydrate moieties.
- a modified FIX comprising a FIX molecule or a biologically active fragment, derivative or variant thereof; and at least one aminooxy PEG bound to the FIX molecule, wherein said aminooxy PEG is attached to the FIX via one or more carbohydrate moieties.
- a modified FVIIa comprising a FVIIa molecule or a biologically active fragment, derivative or variant thereof; and at least one aminooxy PEG bound to the FVIIa molecule, wherein said aminooxy PEG is attached to the FVIIa via one or more carbohydrate moieties.
- a modified FVIII comprising a FVIII molecule or a biologically active fragment, derivative or variant thereof; and at least one aminooxy PEG bound to the FVIII molecule, wherein said aminooxy PEG is attached to the FVIII via one or more carbohydrate moieties.
- a water soluble polymer comprising an active aminooxy linker; said water soluble polymer selected from the group consisting of polyethylene glycol (PEG), branched PEG, polysialic acid (PSA), carbohydrate, polysaccharides, pullulane, chitosan, hyaluronic acid, chondroitin sulfate, dermatan sulfate, starch, dextran, carboxymethyl-dextran, polyalkylene oxide (PAO), polyalkylene glycol (PAG), polypropylene glycol (PPG), polyoxazoline, poly acryloylmorpholine, polyvinyl alcohol (PVA), polycarboxylate, polyvinylpyrrolidone, polyphosphazene, polyoxazoline, polyethylene-co-maleic acid anhydride, polystyrene-co-maleic acid anhydride, poly(1-hydroxymethylethylene hydroxymethylformal) (PHF), 2-methacrylo
- activated aminooxy linker comprises 1-50 ethylene glycol units.
- FIG. 1 shows the primary structure of coagulation Factor IX.
- FIG. 2 shows the coupling of oxidized rFIX to aminooxy-PSA.
- FIG. 3 shows the synthesis of the water soluble di-aminoxy linkers 3-oxa-pentane-1,5-dioxyamine and 3,6,9-trioxa-undecane-1,11-dioxyamine.
- FIG. 4 shows the preparation of aminooxy-PSA.
- FIG. 5 shows the analytical characterization of the PSA-rFIX conjugate employing SDS-PAGE and Coomassie staining.
- FIG. 6 shows the analytical characterization of the PSA-rFIX conjugate employing detection with anti-FIX and anti-PSA antibodies.
- FIG. 7 shows activity of native rFIX and PSA-rFIX conjugate relative to time post infusions.
- FIG. 8 shows PSA-rFVIII and Advate levels relative to time post infusion.
- polymeric compounds such as polyethylene glycol (PEG), branched PEG, polysialic acid (PSA), carbohydrate, polysaccharides, pullulane, chitosan, hyaluronic acid, chondroitin sulfate, dermatan sulfate, starch, dextran, carboxymethyl-dextran, polyalkylene oxide (PAO), polyalkylene glycol (PAG), polypropylene glycol (PPG), polyoxazoline, polyacryloylmorpholine, polyvinyl alcohol (PVA), polycarboxylate, polyvinylpyrrolidone, polyphosphazene, polyoxazoline, polyethylene-co-maleic acid anhydride, polystyrene-co-maleic acid anhydride, poly(1-hydroxymethylethylene hydroxymethylformal) (PHF), 2-methacryloyloxy-2′-ethyl
- PEG polyethylene glycol
- PSA polysialic acid
- the properties of the resulting conjugates generally strongly depend on the structure and the size of the polymer.
- polymers with a defined and narrow size distribution are usually preferred in the art.
- Synthetic polymers like PEG can be manufactured easily with a narrow size distribution, while PSA can be purified in such a manner that results in a final PSA preparation with a narrow size distribution.
- PEGylation reagents with defined polymer chains and narrow size distribution are on the market and commercially available for a reasonable price.
- a soluble polymer such as through polysialylation is one approach to improve the properties of a blood coagulation protein such as FIX, as well as other coagulation proteins (e.g., VWF, FVIIa (see, e US 2008/0221032A1, incorporated herein by reference) and FVIII).
- FIX blood coagulation protein
- other coagulation proteins e.g., VWF, FVIIa (see, e US 2008/0221032A1, incorporated herein by reference) and FVIII).
- blood coagulation proteins including, but not limited to, Factor IX (FIX), Factor VIII (FVIII), Factor VIIa (FVIIa), Von Willebrand Factor (VWF), Factor FV (FV), Factor X (FX), Factor XI, Factor XII (FXII), thrombin (FII), protein C, protein S, tPA, PAI-1, tissue factor (TF) and ADAMTS 13 protease are contemplated by the invention.
- blood coagulation protein refers to any Factor IX (FIX), Factor VIII (FVIII), Factor VIIa (FVIIa), Von Willebrand Factor (VWF), Factor FV (FV), Factor X (FX), Factor XII (FXII), thrombin (FII), protein C, protein S, tPA, PAI-1, tissue factor (TF) and ADAMTS 13 protease which exhibits biological activity that is associated with that particular native blood coagulation protein.
- FIX Factor IX
- FVIII Factor VIIa
- VWF Von Willebrand Factor
- FV Factor FV
- FX Factor X
- FXII Factor XII
- thrombin FII
- the blood coagulation cascade is divided into three distinct segments: the intrinsic, extrinsic, and common pathways (Schenone et al., Curr Opin Hematol. 2004; 11:272-7).
- the cascade involves a series of serine protease enzymes (zymogens) and protein cofactors. When required, an inactive zymogen precursor is converted into the active form, which consequently converts the next enzyme in the cascade.
- the intrinsic pathway requires the clotting factors VIII, IX, X, XI, and XII. Initiation of the intrinsic pathway occurs when prekallikrein, high-molecular-weight kininogen, factor XI (FXI) and factor XII (FXII) are exposed to a negatively charged surface. Also required are calcium ions and phospholipids secreted from platelets.
- the extrinsic pathway is initiated when the vascular lumen of blood vessels is damaged.
- the membrane glycoprotein tissue factor is exposed and then binds to circulating factor VII (FVII) and to small preexisting amounts of its activated form FVIIa. This binding facilitates full conversion of FVII to FVIIa and subsequently, in the presence of calcium and phospholipids, the conversion of factor IX (FIX) to factor IXa (FIXa) and factor X (FX) to factor Xa (FXa).
- FVIIa The association of FVIIa with tissue factor enhances the proteolytic activity by bringing the binding sites of FVII for the substrate (FIX and FX) into closer proximity and by inducing a conformational change, which enhances the enzymatic activity of FVIIa.
- FX Factor XI a
- FVIIa Conversion of FVII to FVIIa is also catalyzed by a number of proteases, including thrombin, FIXa, FXa, factor XIa (FXIa), and factor XIIa (FXIIa).
- tissue factor pathway inhibitor targets FVIIa/tissue factor/FXa product complex.
- the starting material of the present invention is a blood coagulation protein, which can be derived from human plasma, or produced by recombinant engineering techniques, as described in U.S. Pat. No. 4,757,006; U.S. Pat. No. 5,733,873; U.S. Pat. No. 5,198,349; U.S. Pat. No. 5,250,421; U.S. Pat. No. 5,919,766; and EP 306 968.
- the term blood coagulation protein refers to any blood coagulation protein molecule which exhibits biological activity that is associated with the native blood coagulation protein.
- the blood coagulation protein molecule is a full-length blood coagulation protein.
- Blood coagulation protein molecules contemplated include full-length proteins, precursors of full length proteins, biologically active subunits or fragments of full length proteins, as well as biologically active derivatives and variants of any of these forms of blood coagulation proteins.
- blood coagulation protein include those that (1) have an amino acid sequence that has greater than about 60%, about 65%, about 70%, about 75%, about 80%, about 85%, about 90%, about 91%, about 92%, about 93%, about 94%, about 95%, about 96%, about 97%, about 98% or about 99% or greater amino acid sequence identity, over a region of at least about 25, about 50, about 100, about 200, about 300, about 400, or more amino acids, to a polypeptide encoded by a referenced nucleic acid or an amino acid sequence described herein; and/or (2) specifically bind to antibodies, e.g., polyclonal or monoclonal antibodies, generated against an immunogen comprising a referenced amino acid sequence as described herein, an immunogenic fragment thereof, and
- the term “recombinant blood coagulation protein” includes any blood coagulation protein obtained via recombinant DNA technology. In certain embodiments, the term encompasses proteins as described herein.
- endogenous blood coagulation protein includes a blood coagulation protein which originates from the mammal intended to receive treatment.
- the term also includes blood coagulation protein transcribed from a transgene or any other foreign DNA present in said mammal.
- exogenous blood coagulation protein includes a blood coagulation protein which does not originate from the mammal intended to receive treatment.
- plasma-derived blood coagulation protein or “plasmatic” includes all forms of the protein found in blood obtained from a mammal having the property participating in the coagulation pathway.
- biologically active derivative or “biologically active variant” includes any derivative or variant of a molecule having substantially the same functional and/or biological properties of said molecule, such as binding properties, and/or the same structural basis, such as a peptidic backbone or a basic polymeric unit.
- polypeptide variant refers to a polypeptide sharing substantially similar structure and having the same biological activity as a reference polypeptide.
- Variants or analogs differ in the composition of their amino acid sequences compared to the naturally-occurring polypeptide from which the analog is derived, based on one or more mutations involving (i) deletion of one or more amino acid residues at one or more termini of the polypeptide and/or one or more internal regions of the naturally-occurring polypeptide sequence (e.g., fragments), (ii) insertion or addition of one or more amino acids at one or more termini (typically an “addition” or “fusion”) of the polypeptide and/or one or more internal regions (typically an “insertion”) of the naturally-occurring polypeptide sequence or (iii) substitution of one or more amino acids for other amino acids in the naturally-occurring polypeptide sequence.
- a “derivative” refers to a polypeptide sharing the same or substantially similar structure as a reference polypeptide that has been modified, e.g., chemically.
- Variant or analog polypeptides include insertion variants, wherein one or more amino acid residues are added to a blood coagulation protein amino acid sequence of the invention. Insertions may be located at either or both termini of the protein, and/or may be positioned within internal regions of the blood coagulation protein amino acid sequence. Insertion variants, with additional residues at either or both termini, include for example, fusion proteins and proteins including amino acid tags or other amino acid labels.
- the blood coagulation protein molecule optionally contains an N-terminal Met, especially when the molecule is expressed recombinantly in a bacterial cell such as E. coli.
- one or more amino acid residues in a blood coagulation protein polypeptide as described herein are removed.
- Deletions can be effected at one or both termini of the blood coagulation protein polypeptide, and/or with removal of one or more residues within the blood coagulation protein amino acid sequence.
- Deletion variants therefore, include fragments of a blood coagulation protein polypeptide sequence.
- substitution variants one or more amino acid residues of a blood coagulation protein polypeptide are removed and replaced with alternative residues.
- the substitutions are conservative in nature and conservative substitutions of this type are well known in the art.
- the invention embraces substitutions that are also non-conservative. Exemplary conservative substitutions are described in Lehninger, [Biochemistry, 2nd Edition; Worth Publishers, Inc., New York (1975), pp. 71-77] and are set out immediately below.
- Nucleic acids encoding a blood coagulation protein of the invention include, for example and without limitation, genes, pre-mRNAs, mRNAs, cDNAs, polymorphic variants, alleles, synthetic and naturally-occurring mutants.
- Polynucleotides encoding a blood coagulation protein of the invention also include, without limitation, those that (1) specifically hybridize under stringent hybridization conditions to a nucleic acid encoding a referenced amino acid sequence as described herein, and conservatively modified variants thereof; (2) have a nucleic acid sequence that has greater than about 95%, about 96%, about 97%, about 98%, about 99%, or higher nucleotide sequence identity, over a region of at least about 25, about 50, about 100, about 150, about 200, about 250, about 500, about 1000, or more nucleotides (up to the full length sequence of 1218 nucleotides of the mature protein), to a reference nucleic acid sequence as described herein.
- Exemplary “stringent hybridization” conditions include hybridization at 42° C. in 50% formamide, 5 ⁇ SSC, 20 mM Na.PO4, pH 6.8; and washing in 1 ⁇ SSC u
- a “naturally-occurring” polynucleotide or polypeptide sequence is typically from a mammal including, but not limited to, primate, e.g., human; rodent, e.g., rat, mouse, hamster; cow, pig, horse, sheep, or any mammal.
- the nucleic acids and proteins of the invention can be recombinant molecules (e.g., heterologous and encoding the wild type sequence or a variant thereof, or non-naturally occurring).
- polypeptides and polynucleotides are exemplified by the following blood coagulation proteins.
- FVII also known as stable factor or proconvertin
- FVII is a vitamin K-dependent serine protease glycoprotein with a pivotal role in hemostasis and coagulation (Eigenbrot, Curr Protein Pept Sci. 2002; 3:287-99).
- FVII is synthesized in the liver and secreted as a single-chain glycoprotein of 48 kD.
- FVII shares with all vitamin K-dependent serine protease glycoproteins a similar protein domain structure consisting of an amino-terminal gamma-carboxyglutamic acid (Gla) domain with 9-12 residues responsible for the interaction of the protein with lipid membranes, a carboxy-terminal serine protease domain (catalytic domain), and two epidermal growth factor-like domains containing a calcium ion binding site that mediates interaction with tissue factor.
- Gamma-glutamyl carboxylase catalyzes carboxylation of Gla residues in the amino-terminal portion of the molecule.
- the carboxylase is dependent on a reduced form of vitamin K for its action, which is oxidized to the epoxide form.
- Vitamin K epoxide reductase is required to convert the epoxide form of vitamin K back to the reduced form.
- the major proportion of FVII circulates in plasma in zymogen form, and activation of this form results in cleavage of the peptide bond between arginine 152 and isoleucine 153.
- the resulting activated FVIIa consists of a NH 2 -derived light chain (20 kD) and a COOH terminal-derived heavy chain (30 kD) linked via a single disulfide bond (Cys 135 to Cys 262).
- the light chain contains the membrane-binding Gla domain, while the heavy chain contains the catalytic domain.
- the plasma concentration of FVII determined by genetic and environmental factors is about 0.5 mg/mL (Pinotti et al., Blood. 2000; 95:3423-8). Different FVII genotypes can result in several-fold differences in mean FVII levels. Plasma FVII levels are elevated during pregnancy in healthy females and also increase with age and are higher in females and in persons with hypertriglyceridemia. FVII has the shortest half-life of all procoagulant factors (3-6 h). The mean plasma concentration of FVIIa is 3.6 ng/mL in healthy individuals and the circulating half-life of FVIIa is relatively long (2.5 h) compared with other coagulation factors.
- Hereditary FVII deficiency is a rare autosomal recessive bleeding disorder with a prevalence estimated to be 1 case per 500,000 persons in the general population (Acharya et al., J Thromb Haemost. 2004; 2248-56). Acquired FVII deficiency from inhibitors is also very rare. Cases have also been reported with the deficiency occurring in association with drugs such as cephalosporins, penicillins, and oral anticoagulants. Furthermore, acquired FVII deficiency has been reported to occur spontaneously or with other conditions, such as myeloma, sepsis, aplastic anemia, with interleukin-2 and antithymocyte globulin therapy.
- Reference polynucleotide and polypeptide sequences include, e.g., GenBank Accession Nos. J02933 for the genomic sequence, M13232 for the cDNA (Hagen et al. PNAS 1986; 83: 2412-6), and P08709 for the polypeptide sequence (references incorporated herein in their entireties).
- GenBank Accession Nos. J02933 for the genomic sequence
- M13232 for the cDNA Hagen et al. PNAS 1986; 83: 2412-6
- P08709 for the polypeptide sequence
- FIX is a vitamin K-dependent plasma protein that participates in the intrinsic pathway of blood coagulation by converting FX to its active form in the presence of calcium ions, phospholipids and FVIIIa.
- the predominant catalytic capability of FIX is as a serine protease with specificity for a particular arginine-isoleucine bond within FX.
- Activation of FIX occurs by FXIa which causes excision of the activation peptide from FIX to produce an activated FIX molecule comprising two chains held by one or more disulphide bonds. Defects in FIX are the cause of recessive X-linked hemophilia B.
- Hemophilia A and B are inherited diseases characterized by deficiencies in FVIII and FIX polypeptides, respectively.
- the underlying cause of the deficiencies is frequently the result of mutations in FVIII and FIX genes, both of which are located on the X chromosome.
- Traditional therapy for hemophilias often involves intravenous administration of pooled plasma or semi-purified coagulation proteins from normal individuals. These preparations can be contaminated by pathogenic agents or viruses, such as infectious prions, HIV, parvovirus, hepatitis A, and hepatitis C. Hence, there is an urgent need for therapeutic agents that do not require the use of human serum.
- the level of the decrease in FIX activity is directly proportional to the severity of hemophilia B.
- the current treatment of hemophilia B consists of the replacement of the missing protein by plasma-derived or recombinant FIX (so-called FIX substitution or replacement treatment or therapy).
- Polynucleotide and polypeptide sequences of FIX can be found for example in the UniProtKB/Swiss-Prot Accession No. P00740, U.S. Pat. No. 6,531,298 and in FIG. 1 .
- Coagulation factor VIII (FVIII) circulates in plasma at a very low concentration and is bound non-covalently to Von Willebrand factor (VWF). During hemostasis, FVIII is separated from VWF and acts as a cofactor for activated factor IX (FIXa)-mediated FX activation by enhancing the rate of activation in the presence of calcium and phospholipids or cellular membranes.
- VWF Von Willebrand factor
- FVIII is synthesized as a single-chain precursor of approximately 270-330 kD with the domain structure A1-A2-B-A3-C1-C2.
- FVIII is composed of a heavy chain (A1-A2-B) and a light chain (A3-C1-C2).
- the molecular mass of the light chain is 80 kD whereas, due to proteolysis within the B domain, the heavy chain is in the range of 90-220 kD.
- FVIII is also synthesized as a recombinant protein for therapeutic use in bleeding disorders.
- Various in vitro assays have been devised to determine the potential efficacy of recombinant FVIII (rFVIII) as a therapeutic medicine. These assays mimic the in vivo effects of endogenous FVIII.
- In vitro thrombin treatment of FVIII results in a rapid increase and subsequent decrease in its procoagulant activity, as measured by in vitro assays. This activation and inactivation coincides with specific limited proteolysis both in the heavy and the light chains, which alter the availability of different binding epitopes in FVIII, e.g. allowing FVIII to dissociate from VWF and bind to a phospholipid surface or altering the binding ability to certain monoclonal antibodies.
- the lack or dysfunction of FVIII is associated with the most frequent bleeding disorder, hemophilia A.
- the treatment of choice for the management of hemophilia A is replacement therapy with plasma derived or rFVIII concentrates. Patients with severe haemophilia A with FVIII levels below 1%, are generally on prophylactic therapy with the aim of keeping FVIII above 1% between doses. Taking into account the average half-lives of the various FVIII products in the circulation, this result can usually be achieved by giving FVIII two to three times a week.
- Reference polynucleotide and polypeptide sequences include, e.g., UniProtKB/Swiss-Prot P00451 (FA8_HUMAN); Gitschier J et al., Characterization of the human Factor VIII gene, Nature, 312(5992): 326-30 (1984); Vehar G H et al., Structure of human Factor VIII, Nature, 312(5992):337-42 (1984); Thompson A R. Structure and Function of the Factor VIII gene and protein, Semin Thromb Hemost, 2003:29; 11-29 (2002).
- Von Willebrand factor is a glycoprotein circulating in plasma as a series of multimers ranging in size from about 500 to 20,000 kD.
- Multimeric forms of VWF are composed of 250 kD polypeptide subunits linked together by disulfide bonds. VWF mediates initial platelet adhesion to the sub-endothelium of the damaged vessel wall. Only the larger multimers exhibit hemostatic activity. It is assumed that endothelial cells secrete large polymeric forms of VWF and those forms of VWF which have a low molecular weight (low molecular weight VWF) arise from proteolytic cleavage.
- the multimers having large molecular masses are stored in the Weibel-Pallade bodies of endothelial cells and liberated upon stimulation.
- VWF is synthesized by endothelial cells and megakaryocytes as prepro-VWF that consists to a large extent of repeated domains.
- pro-VWF dimerizes through disulfide linkages at its C-terminal region.
- the dimers serve as protomers for multimerization, which is governed by disulfide linkages between the free end termini.
- the assembly to multimers is followed by the proteolytic removal of the propeptide sequence (Leyte et al., Biochem. J. 274 (1991), 257-261).
- the primary translation product predicted from the cloned cDNA of VWF is a 2813-residue precursor polypeptide (prepro-VWF).
- the prepro-VWF consists of a 22 amino acid signal peptide and a 741 amino acid propeptide, with the mature VWF comprising 2050 amino acids (Ruggeri Z. A., and Ware, J., FASEB J., 308-316 (1993).
- VWD type 3 is the most severe form in which VWF is completely missing, and VWD type 1 relates to a quantitative loss of VWF and its phenotype can be very mild.
- VWD type 2 relates to qualitative defects of VWF and can be as severe as VWD type 3.
- VWD type 2 has many sub forms, some being associated with the loss or the decrease of high molecular weight multimers.
- Von Willebrand disease type 2a (VWD-2A) is characterized by a loss of both intermediate and large multimers.
- VWD-2B is characterized by a loss of highest-molecular-weight multimers.
- Other diseases and disorders related to VWF are known in the art.
- polynucleotide and amino acid sequences of prepro-VWF are available at GenBank Accession Nos. NM — 000552 and NP — 000543, respectively.
- Production of a blood coagulation protein includes any method known in the art for (i) the production of recombinant DNA by genetic engineering, (ii) introducing recombinant DNA into prokaryotic or eukaryotic cells by, for example and without limitation, transfection, electroporation or microinjection, (iii) cultivating said transformed cells, (iv) expressing blood coagulation protein, e.g. constitutively or upon induction, and (v) isolating said blood coagulation protein, e.g. from the culture medium or by harvesting the transformed cells, in order to obtain purified blood coagulation protein.
- the blood coagulation protein is produced by expression in a suitable prokaryotic or eukaryotic host system characterized by producing a pharmacologically acceptable blood coagulation protein molecule.
- suitable prokaryotic or eukaryotic host system characterized by producing a pharmacologically acceptable blood coagulation protein molecule.
- eukaryotic cells are mammalian cells, such as CHO, COS, HEK 293, BHK, SK-Hep, and HepG2.
- vectors are used for the preparation of the blood coagulation protein and are selected from eukaryotic and prokaryotic expression vectors.
- vectors for prokaryotic expression include plasmids such as, and without limitation, pRSET, pET, and pBAD, wherein the promoters used in prokaryotic expression vectors include one or more of, and without limitation, lac, trc, trp, recA, or araBAD.
- vectors for eukaryotic expression include: (i) for expression in yeast, vectors such as, and without limitation, pAO, pPIC, pYES, or pMET, using promoters such as, and without limitation, AOX1, GAP, GAL1, or AUG1; (ii) for expression in insect cells, vectors such as and without limitation, pMT, pAc5, pIB, pMIB, or pBAC, using promoters such as and without limitation PH, p10, MT, Ac5, OpIE2, gp64, or polh, and (iii) for expression in mammalian cells, vectors such as and without limitation pSVL, pCMV, pRc/RSV, pcDNA3, or pBPV, and vectors derived from, in one aspect, viral systems such as and without limitation vaccinia virus, adeno-associated viruses, herpes viruses, or retroviruses, using promoters such as and without limitation C
- a conjugated blood coagulation protein of the present invention may be administered by injection, such as intravenous, intramuscular, or intraperitoneal injection.
- compositions comprising a conjugated blood coagulation protein of the present invention to human or test animals
- the compositions comprise one or more pharmaceutically acceptable carriers.
- pharmaceutically acceptable carriers include any and all clinically useful solvents, dispersion media, coatings, antibacterial and antifungal agents, isotonic and absorption delaying agents and the like, including those agents disclosed above.
- an effective amount includes a dose suitable for treating a mammal having a bleeding disorder as described herein.
- compositions may be administered orally, topically, transdermally, parenterally, by inhalation spray, vaginally, rectally, or by intracranial injection.
- parenteral as used herein includes subcutaneous injections, intravenous, intramuscular, intracisternal injection, or infusion techniques. Administration by intravenous, intradermal, intramuscular, intramammary, intraperitoneal, intrathecal, retrobulbar, intrapulmonary injection and or surgical implantation at a particular site is contemplated as well.
- compositions are essentially free of pyrogens, as well as other impurities that could be harmful to the recipient.
- Single or multiple administrations of the compositions can be carried out with the dose levels and pattern being selected by the treating physician.
- the appropriate dosage will depend on the type of disease to be treated, as described above, the severity and course of the disease, whether drug is administered for preventive or therapeutic purposes, previous therapy, the patient's clinical history and response to the drug, and the discretion of the attending physician.
- the present invention also relates to a pharmaceutical composition
- a pharmaceutical composition comprising an effective amount of a conjugated blood coagulation protein as defined herein.
- the pharmaceutical composition may further comprise a pharmaceutically acceptable carrier, diluent, salt, buffer, or excipient.
- the pharmaceutical composition can be used for treating the above-defined bleeding disorders.
- the pharmaceutical composition of the invention may be a solution or a lyophilized product. Solutions of the pharmaceutical composition may be subjected to any suitable lyophilization process.
- kits which comprise a composition of the invention packaged in a manner which facilitates its use for administration to subjects.
- a kit includes a compound or composition described herein (e.g., a composition comprising a conjugated blood coagulation protein), packaged in a container such as a sealed bottle or vessel, with a label affixed to the container or included in the package that describes use of the compound or composition in practicing the method.
- the kit contains a first container having a composition comprising a conjugated blood coagulation protein and a second container having a physiologically acceptable reconstitution solution for the composition in the first container.
- the compound or composition is packaged in a unit dosage form.
- the kit may further include a device suitable for administering the composition according to a specific route of administration.
- the kit contains a label that describes use of the therapeutic protein or peptide composition.
- a blood coagulation protein derivative i.e., a conjugated blood coagulation protein
- a water-soluble polymer including, but not limited to, polyethylene glycol (PEG), branched PEG, polysialic acid (PSA), carbohydrate, polysaccharides, pullulane, chitosan, hyaluronic acid, chondroitin sulfate, dermatan sulfate, starch, dextran, carboxymethyl-dextran, polyalkylene oxide (PAO), polyalkylene glycol (PAG), polypropylene glycol (PPG) polyoxazoline, poly acryloylmorpholine, polyvinyl alcohol (PVA), polycarboxylate, polyvinylpyrrolidone, polyphosphazene, polyoxazoline, polyethylene-co-maleic acid anhydride, polystyrene-co-maleic acid anhydride, poly(O)hydroxymethylethylene hydroxymethyl
- the water soluble polymer is consisting of sialic acid molecule having a molecular weight range of 350 to 120,000, 500 to 100,000, 1000 to 80,000, 1500 to 60,000, 2,000 to 45,000 Da, 3,000 to 35,000 Da, and 5,000 to 25,000 Da.
- the coupling of the water soluble polymer can be carried out by direct coupling to the protein or via linker molecules.
- a chemical linker is MBPH (4-[4-N-Maleimidophenyl]butyric acid hydrazide) containing a carbohydrate-selective hydrazide and a sulfhydryl-reactive maleimide group (Chamow et al., J Biol Chem 1992; 267: 15916-22).
- MBPH 4-[4-N-Maleimidophenyl]butyric acid hydrazide
- Other exemplary and preferred linkers are described below.
- the derivative retains the full functional activity of native therapeutic blood coagulation protein products, and provides an extended half-life in vivo, as compared to native therapeutic blood coagulation protein products. In another embodiment, the derivative retains at least 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44.
- the biological activities of the derivative and native blood coagulation protein are determined by the ratios of chromogenic activity to blood coagulation factor antigen value (blood coagulation factor:Chr:blood coagulation factor:Ag).
- the half-life of the construct is decreased or increased 0.5, 0.6, 0.7, 0.8, 0.9, 1.0, 1.1, 1.2, 1.3, 1.4, 1.5, 2, 3, 4, 5, 6, 7, 8, 9, or 10-fold relative to the in vivo half-life of native blood coagulation protein.
- sialic acid moieties includes sialic acid monomers or polymers (“polysaccharides”) which are soluble in an aqueous solution or suspension and have little or no negative impact, such as side effects, to mammals upon administration of the PSA-blood coagulation protein conjugate in a pharmaceutically effective amount.
- the polymers are characterized, in one aspect, as having 1, 2, 3, 4, 5, 10, 20, 30, 40, 50, 60, 70, 80, 90, 100, 200, 300, 400, or 500 sialic acid units. In certain aspects, different sialic acid units are combined in a chain.
- the sialic acid portion of the polysaccharide compound is highly hydrophilic, and in another embodiment the entire compound is highly hydrophilic. Hydrophilicity is conferred primarily by the pendant carboxyl groups of the sialic acid units, as well as the hydroxyl groups.
- the saccharide unit may contain other functional groups, such as, amine, hydroxyl or sulphate groups, or combinations thereof. These groups may be present on naturally-occurring saccharide compounds, or introduced into derivative polysaccharide compounds.
- the naturally occurring polymer PSA is available as a polydisperse preparation showing a broad size distribution (e.g. Sigma C-5762) and high polydispersity (PD). Because the polysaccharides are usually produced in bacteria carrying the inherent risk of copurifying endotoxins, the purification of long sialic acid polymer chains may raise the probability of increased endotoxin content. Short PSA molecules with 1-4 sialic acid units can also be synthetically prepared (Kang S H et al., Chem. Commun. 2000; 227-8; Ress D K and Linhardt R J, Current Organic Synthesis. 2004; 1:31-46), thus minimizing the risk of high endotoxin levels.
- Polysaccharide compounds of particular use for the invention are, in one aspect, those produced by bacteria. Some of these naturally-occurring polysaccharides are known as glycolipids. In one embodiment, the polysaccharide compounds are substantially free of terminal galactose units.
- blood coagulation factor e.g., FVIII, FVIIa, FIX, or other blood coagulation factor molecules are conjugated to a water soluble polymer by any of a variety of chemical methods (Roberts J M et al., Advan Drug Delivery Rev 2002; 54:459-76).
- FVIII, FVIIa, or FIX is modified by the conjugation of PEG to free amino groups of the protein using N-hydroxysuccinimide (NHS) esters.
- NHS N-hydroxysuccinimide
- water soluble polymer for example PEG
- PEG is coupled to free SH groups using maleimide chemistry or the coupling of PEG hydrazides or PEG amines to carbohydrate moieties of the FVIII, FVIIa, or FIX after prior oxidation.
- the conjugation is in one aspect performed by direct coupling (or coupling via linker systems) of the water soluble polymer to blood coagulation factor, e.g., FVIII. FVIIa, or FIX, under formation of stable bonds.
- blood coagulation factor e.g., FVIII. FVIIa, or FIX
- degradable, releasable or hydrolysable linker systems are used in certain aspects the present invention (Tsubery et al. J Biol Chem 2004; 279: 38118-24/Greenwald et al., J Med Chem 1999; 42:3657-67/Zhao et al., Bioconj Chem 2006; 17:341-51/WO2006/138572A2/U.S. Pat. No. 7,259,224B2/U.S. Pat. No. 7,060,259B2).
- a blood coagulation factor e.g., FVIII, FVIIa, or FIX
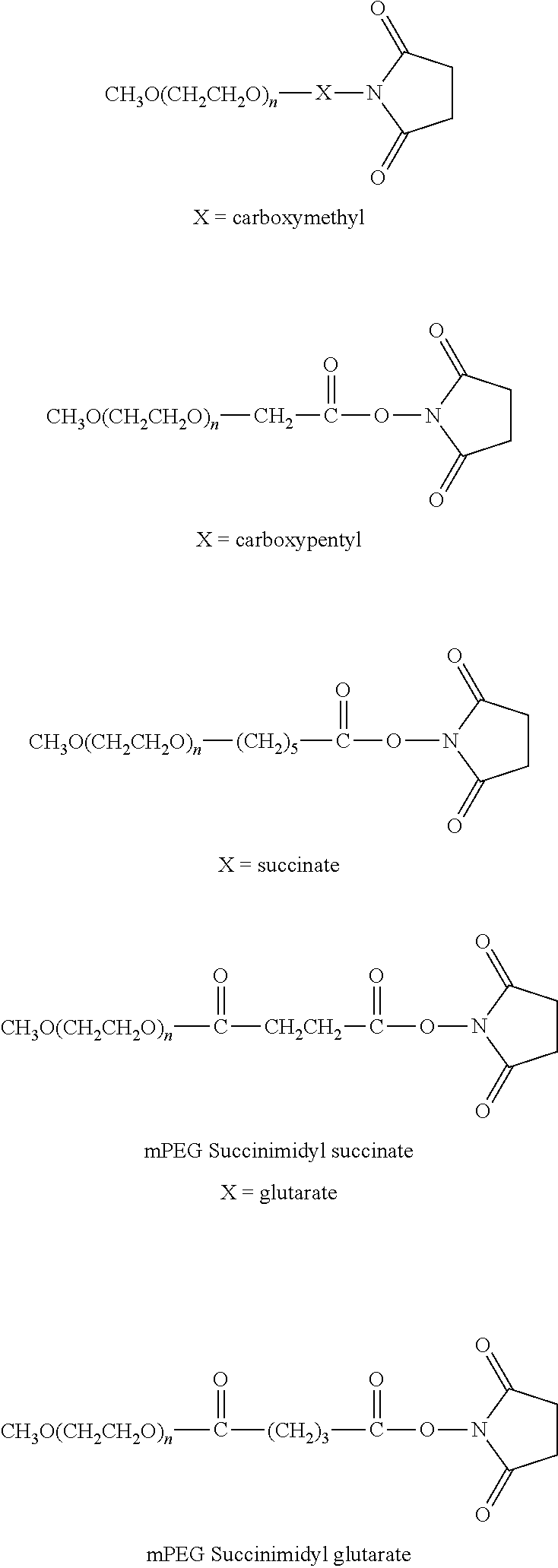
- polyethylene glycol derivatives containing an active N-hydroxysuccinimide ester such as succinimidyl succinate, succinimidyl glutarate or succinimidyl propionate.
- NHS N-hydroxysuccinimide ester
- these derivatives react with the lysine residues of FVIII, FVIIa, or FIX under mild conditions by forming a stable amide bond.
- the chain length of the PEG derivative is 5,000 Da.
- PEG derivatives with chain lengths of 500 to 2,000 Da, 2,000 to 5,000 Da, greater than 5,000 up to 10,000 Da or greater than 10,000 up to 20,000 Da, or greater than 20,000 up to 150,000 Da are used in various embodiments, including linear and branched structures.
- PEGylation of amino groups are, without limitation, the chemical conjugation with PEG carbonates by forming urethane bonds, or the reaction with aldehydes or ketones by reductive amination forming secondary amide bonds.
- a blood coagulation factor e.g., FVIII, FVIIa, FIX, or other blood coagulation factor, molecule is chemically modified using PEG derivatives that are commercially available. These PEG derivatives in alternative aspects have a linear or branched structures. Examples of PEG-derivatives containing NHS groups are listed below.
- PEG derivatives are non-limiting examples of those commercially available from Nektar Therapeutics (Huntsville, Ala.; see www.nektar.com/PEG reagent catalog; Nektar Advanced PEGylation, price list 2005-2006):
- PEG derivatives are commercially available from NOF Corporation (Tokyo, Japan; see www.nof.co.jp/english: Catalogue 2005)
- propane derivatives show a glycerol backbone with a 1,2 substitution pattern.
- branched PEG derivatives based on glycerol structures with 1,3 substitution or other branched structures described in US2003/0143596A1 are also contemplated.
- PEG derivatives with degradable for example, hydrolysable linkers
- degradable linkers for example, hydrolysable linkers
- the PE FVIII, FVIIa, FIX, or other blood coagulation factor of this invention exhibits functional activity, combined with an extended half-life in vivo.
- the PEGylated rFVIII, FVIIa, FIX, or other blood coagulation factor seems to be more resistant against thrombin inactivation.
- a blood coagulation protein may be covalently linked to the polysaccharide compounds by any of various techniques known to those of skill in the art.
- sialic acid moieties are bound to a blood coagulation protein, e.g., FIX, FVIII, FVIIa or VWF, for example by the method described in U.S. Pat. No. 4,356,170, which is herein incorporated by reference.
- Exemplary techniques include linkage through a peptide bond between a carboxyl group on one of either the blood coagulation protein or polysaccharide and an amine group of the blood coagulation protein or polysaccharide, or an ester linkage between a carboxyl group of the blood coagulation protein or polysaccharide and a hydroxyl group of the blood coagulation protein or polysaccharide.
- Another linkage by which the blood coagulation protein is covalently bonded to the polysaccharide compound is via a Schiff base, between a free amino group on the blood coagulation protein being reacted with an aldehyde group formed at the non-reducing end of the polysaccharide by periodate oxidation (Jennings H J and Lugowski C, J. Immunol. 1981; 127:1011-8; Fernandes A I and Gregoriadis G, Biochim Biophys Acta. 1997; 1341; 26-34).
- the generated Schiff base is in one aspect stabilized by specific reduction with NaCNBH3 to form a secondary amine.
- Bifunctional reagents can be used for linking two amino or two hydroxyl groups.
- PSA containing an amino group is coupled to amino groups of the protein with reagents like BS3 (Bis(sulfosuccinimidyl)suberate/Pierce, Rockford, Ill.).
- reagents like BS3 (Bis(sulfosuccinimidyl)suberate/Pierce, Rockford, Ill.).
- heterobifunctional cross linking reagents like Sulfo-EMCS(N- ⁇ -Maleimidocaproyloxy) sulfosuccinimide ester/Pierce) is used for instance to link amine and thiol groups.
- a PSA hydrazide is prepared and coupled to the carbohydrate moiety of the protein after prior oxidation and generation of aldehyde functions.
- a free amine group of the therapeutic protein reacts with the 1-carboxyl group of the sialic acid residue to form a peptidyl bond or an ester linkage is formed between the 1-carboxylic acid group and a hydroxyl or other suitable active group on a blood coagulation protein.
- a carboxyl group forms a peptide linkage with deacetylated 5-amino group
- an aldehyde group of a molecule of a blood coagulation protein forms a Schiff base with the N-deacetylated 5-amino group of a sialic acid residue.
- the polysaccharide compound is associated in a non-covalent manner with a blood coagulation protein.
- the polysaccharide compound and the pharmaceutically active compound are in one aspect linked via hydrophobic interactions.
- Other non-covalent associations include electrostatic interactions, with oppositely charged ions attracting each other.
- the blood coagulation protein is linked to or associated with the polysaccharide compound in stoichiometric amounts (e.g., 1:1, 1:2, 1:3, 1:4, 1:5, 1:6, 1:7, 1:7, 1:8, 1:9, or 1:10, etc.).
- 1-6, 7-12 or 13-20 polysaccharides are linked to the blood coagulation protein.
- 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 or more polysaccharides are linked to the blood coagulation protein.
- the blood coagulation protein is modified to introduce glycosylation sites (i.e., sites other than the native glycosylation sites). Such modification may be accomplished using standard molecular biological techniques known in the art.
- the blood coagulation protein prior to conjugation to a water soluble polymer via one or more carbohydrate moieties, may be glycosylated in vivo or in vitro. These glycosylated sites can serve as targets for conjugation of the proteins with water soluble polymers (US Patent Application No. 20090028822, US Patent Application No. 2009/0093399, US Patent Application No. 2009/0081188, US Patent Application No. 2007/0254836, US Patent Application No. 2006/0111279, and DeFrees S. et al., Glycobiology, 2006, 16, 9, 833-43).
- the reaction of hydroxylamine or hydroxylamine derivatives with aldehydes (e.g., on a carbohydrate moiety following oxidation by sodium periodate) to form an oxime group is applied to the preparation of conjugates of blood coagulation protein.
- a glycoprotein e.g., a blood coagulation protein according to the present invention
- a oxidizing agent such as sodium periodate (NaIO 4 ) (Rothfus J A et Smith E L., J Biol Chem 1963, 238, 1402-10; and Van Lenten L and Ashwell G., J Biol Chem 1971, 246, 1889-94).
- the periodate oxidation of glycoproteins is based on the classical Malaprade reaction described in 1928, the oxidation of vicinal diols with periodate to form an active aldehyde group (Malaprade L., Analytical application, Bull Soc Chim France, 1928, 43, 683-96). Additional examples for such an oxidizing agent are lead tetraacetate (Pb(OAc) 4 ), manganese acetate (MnO(Ac) 3 ), cobalt acetate (Co(OAc) 2 ), thallium acetate (TlOAc), cerium sulfate (Ce(SO 4 ) 2 ) (U.S. Pat. No.
- oxidizing agent a mild oxidizing compound which is capable of oxidizing vicinal diols in carbohydrates, thereby generating active aldehyde groups under physiological reaction conditions is meant.
- the second step is the coupling of the polymer containing an aminooxy group to the oxidized carbohydrate moiety to form an oxime linkage.
- this step can be carried out in the presence of catalytic amounts of the nucleophilic catalyst aniline or aniline derivatives (Dirksen A et Dawson P E, Bioconjugate Chem. 2008; Zeng Y et al., Nature Methods 2009; 6:207-9).
- the aniline catalysis dramatically accelerates the oxime ligation allowing the use of very low concentrations of the reagents.
- the oxime linkage is stabilized by reduction with NaCNBH3 to form an alkoxyamine linkage ( FIG. 2 ).
- reaction steps to conjugate a water soluble polymer to a blood coagulation protein are carried out separately and sequentially (i.e., starting materials (e.g., blood coagulation protein, water soluble polymer, etc), reagents (e.g., oxidizing agents, aniline, etc) and reaction products (e.g., oxidized carbohydrate on a blood coagulation protein, activated aminooxy water soluble polymer, etc) are separated between individual reaction steps).
- starting materials e.g., blood coagulation protein, water soluble polymer, etc
- reagents e.g., oxidizing agents, aniline, etc
- reaction products e.g., oxidized carbohydrate on a blood coagulation protein, activated aminooxy water soluble polymer, etc
- EP 1681303A1 HASylated erythropoietin
- WO 2005/014024 conjugates of a polymer and a protein linked by an oxime linking group
- WO96/40662 aminooxy-containing linker compounds and their application in conjugates
- WO 2008/025856 Modified proteins
- Kubler-Kielb J et Kubler-Kielb J et.
- the water soluble polymer which is linked according to the aminooxy technology described herein to an oxidized carbohydrate moiety of a blood coagulation protein include, but are not limited to polyethylene glycol (PEG), branched PEG, polysialic acid (PSA), carbohydrate, polysaccharides, pullulane, chitosan, hyaluronic acid, chondroitin sulfate, dermatan sulfate, starch, dextran, carboxymethyl-dextran, polyalkylene oxide (PAO), polyalkylene glycol (PAG), polypropylene glycol (PPG) polyoxazoline, poly acryloylmorpholine, polyvinyl alcohol (PVA), polycarboxylate, polyvinylpyrrolidone, polyphosphazene, polyoxazoline, polyethylene-co-maleic acid anhydride, polyst
- UF/DF ultrafiltration/diafiltration procedure
- the excess PSA reagent was removed by hydrophobic interaction chromatography (HIC).
- HIC hydrophobic interaction chromatography
- the conductivity of the cooled reaction mixture was raised to 180 mS/cm and loaded onto a 5 ml HiTrap Butyl FF (GE Healthcare, Fairfield, Conn.) HIC column (1.6 ⁇ 2.5 cm), pre-equilibrated with 50 mM HEPES, 3M sodium chloride, 6.7 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- the conjugate was eluted within 2.4 column volumes (CV) with 50 mM HEPES, 6.7 mM calcium chloride, 0.005% Tween 80, pH 7.4 at a flow rate of 5 ml/min.
- the preparation was analytically characterized by measuring total protein (BCA) and FIX chromogenic activity.
- BCA total protein
- FIX FIX chromogenic activity
- FIG. 5 The analytical characterization of the PSA-rFIX conjugate by SDS-PAGE with Coomassie staining is illustrated in FIG. 5 .
- FIG. 6 An SDS-PAGE followed by Western blot employing anti-FIX and anti-PSA antibodies is shown in FIG. 6 .
- the conductivity of the cooled reaction mixture was raised to 180 mS/cm and loaded onto a 5 ml HiTrap Butyl FF (GE Healthcare, Fairfield, Conn.) HIC column (1.6 ⁇ 2.5 cm), pre-equilibrated with 50 mM HEPES, 3M sodium chloride, 6.7 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- the conjugate was eluted with a linear gradient to 50 mM HEPES, 6.7 mM calcium chloride, 0.005% Tween 80, pH 7.4 in 20 CV with at a flow rate of 5 ml/min.
- the excess PSA reagent was removed by means of HIC.
- the conductivity of the cooled reaction mixture was raised to 180 mS/cm and loaded onto a 5 ml HiTrap Butyl FF (GE Healthcare, Fairfield, Conn.) HIC column (1.6 ⁇ 2.5 cm), pre-equilibrated with 50 mM HEPES, 3M sodium chloride, 6.7 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- the conjugate was eluted within 2.4 CV with 50 mM HEPES, 6.7 mM calcium chloride, 0.005% Tween 80, pH 7.4 at a flow rate of 5 ml/min.
- the ionic strength was increased by adding a buffer containing 8M ammonium acetate (8M ammonium acetate, 50 mM Hepes, 5 mM CaCl 2 , 350 mM NaCl, 0.01% Tween 80, pH 6.9) to get a final concentration of 2.5M ammonium acetate.
- a buffer containing 8M ammonium acetate 8M ammonium acetate, 50 mM Hepes, 5 mM CaCl 2 , 350 mM NaCl, 0.01% Tween 80, pH 6.9
- equilibration buffer 2.5M ammonium acetate, 50 mM Hepes, 5 mM CaCl 2 , 350 mM NaCl, 0.01% Tween 80, pH 6.9.
- the product was eluted with elution buffer (50 mM Hepes, 5 mM CaCl 2 , 0.01% Tween 80, pH 7.4), and the eluate was concentrated by centrifugal filtration using Vivaspin (Sartorius, Goettingen, Germany) devices with 30,000 MWCO.
- elution buffer 50 mM Hepes, 5 mM CaCl 2 , 0.01% Tween 80, pH 7.4
- FIX-deficient mice were injected with either rFIX or PSA-rFIX (prepared according to Example 4) in formulation buffer (10 mM histidine, 260 mM glycine, 29 mM sucrose, 0.005% Tween 80, pH 6.8) in a volume dose of 10 ml/kg bodyweight.
- formulation buffer 10 mM histidine, 260 mM glycine, 29 mM sucrose, 0.005% Tween 80, pH 6.8
- FIX activity was determined with a chromogenic FIX assay (Biophen FIX assay, Hyphen Biomed, Neuville-sur-Oise, France) and elimination curves were constructed ( FIG. 7 ). Actual FIX activity doses were 123 IU FIX/kg for PSA-rFIX and 143 IU FIX/kg for rFIX. Pharmacokinetic parameters were calculated with program R (The R Foundation for Statistical Computing, 2008). In vivo recovery was 13% for rFIX and 29% for PSA-rFIX.
- Polysialylation as described herein may be extended to other coagulation proteins.
- the above polysialylation as described in Examples 5, 6 and 9 with aminooxy-PSA is repeated with coagulation proteins such as FVIII, FVIIa and VWF.
- An Aminooxy-PSA reagent is prepared by use of a maleimido/aminooxy linker system (Toyokuni et al., Bioconjugate Chem 2003; 14, 1253-9).
- PSA-SH (20 kD) containing a free terminal SH-group is prepared using a two step procedure: a) Preparation of PSA-NH 2 by reductive amination of oxidized PSA with NH 4 Cl according to WO05016973A1 and b) introduction of a sulfhydryl group by reaction of the terminal primary amino group with 2-iminothiolane (Traut's reagent/Pierce, Rockford, Ill.) as described in U.S. Pat. No. 7,645,860.
- PSA-SH is coupled to the maleimido-group of the linker at pH 7.5 in PBS-buffer using a 10 fold molar excess of the linker and a PSA-SH concentration of 50 mg/ml.
- the reaction mixture is incubated for 2 hours under gentle shaking at room temperature. Then the excess linker reagent is removed and the aminooxy-PSA is buffer exchanged into oxidation buffer (50 mM sodium phosphate, pH 6.0) by diafiltration.
- the buffer is exchanged 25 times employing a Pellicon XL5 kD regenerated cellulose membrane (Millipore, Billerica, Mass.).
- rFIX is oxidized in 50 mM sodium phosphate buffer, pH 6.0 employing 100 uM sodium periodate in the buffer. The mixture was shaken in the dark for 1 h at 4° C. and quenched for 15 min at room temperature by the addition of glycerol to a final concentration of 5 mM. Low molecular weight contaminates were removed by means of size exclusion chromatography (SEC) employing PD-10 desalting columns (GE Healthcare, Fairfield, Conn.). Oxidized rFIX is then spiked with aniline to obtain a final concentration of 10 mM and mixed with the aminooxy-PSA reagent to achieve a 5 fold molar excess of PSA. The reaction mixture was incubated for 2 hours under gentle shaking in the dark at room temperature.
- SEC size exclusion chromatography
- the excess of PSA reagent and free rFIX is removed by means of HIC.
- the conductivity of the reaction mixture is raised to 180 mS/cm and loaded onto a column filled with 48 ml Butyl-Sepharose FF (GE Healthcare, Fairfield, Conn.) pre-equilibrated with 50 mM Hepes, 3 M sodium chloride, 6.7 mM calcium chloride, 0.01% Tween 80, pH 6.9. Subsequently the conjugate is eluted with a linear gradient of 60% elution buffer (50 mM Hepes, 6.7 mM calcium chloride, pH 7.4) in 40 CV.
- 60% elution buffer 50 mM Hepes, 6.7 mM calcium chloride, pH 7.4
- PSA-rFIX containing fractions are collected and subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Millipore).
- the preparation is analytically characterized by measuring total protein (BCA) and FIX chromogenic activity.
- BCA total protein
- FIX chromogenic activity For the PSA-rFIX conjugates prepared with both variants a specific activity of >50% in comparison to native rFIX is determined.
- An Aminooxy-PSA reagent was prepared according to Example 3. The final product was diafiltrated against buffer, pH 7.2 (50 mM Hepes) using a 5 kD membrane (regenerated cellulose, Millipore), frozen at ⁇ 80° C. and lyophilized. After lyophilization the reagent was dissolved in the appropriate volume of water and used for preparation of PSA-protein conjugates via carbohydrate modification.
- a PSA-FVIII conjugate was prepared according Example 8.
- the conjugate showed a specific activity of 6237 IU/mg (FVIII activity determined by the chromogenic assay; total protein determined by the Bradford assay) and had a polysialylation degree of 6.7 (mole PSA per mole FVIII) as measured by the Resorcinol assay (Svennerholm L, Biochim Biophys Acta 1957; 24: 604-11).
- FVIII deficient mice described in detail by Bi et al. were used as a model of severe human hemophilia A.
- Groups of 6 mice received a bolus injection (200 IU FVIII/kg) via the tail vein with either PSA-rFVIII prepared according to Example 8 or native rFVIII (ADVATE, Baxter Healthcare Corporation) in a dose of 200 IU FVIII/kg bodyweight.
- Citrate plasma by heart puncture after anesthesia was prepared from the respective groups 5 minutes, 3, 6, 9, 16, 24, 32 and 42 hours after injection.
- FVIII activity levels were measured in plasma samples by use of the chromogenic assay. The results of this experiment are summarized in Table 3 and illustrated in FIG. 8 .
- 3-oxa-pentane-1,5 dioxyamine was synthesized according to Botyryn et al (Tetrahedron 1997; 53:5485-92) in a two step organic synthesis as outlined in Example 1.
- the Dichloromethane layer was dried over Na 2 SO 4 and then evaporated to dryness under reduced pressure and dried in high vacuum to give 64.5 g of 3-oxapentane-1,5-dioxy-endo-2′,3′-dicarboxydiimidenorbornene as a white-yellow solid (intermediate 1).
- the crude product was further purified by column chromatography (Silicagel 60; isocratic elution with Dichloromethane/Methanol mixture, 9+1) to yield 11.7 g of the pure final product 3-oxa-pentane-1,5-dioxyamine.
- rFIX is polysialylated by use of a PSA hydrazide reagent, which was prepared by reaction of oxidized PSA with adipic acid dihydrazide (ADH).
- rFIX is polysialylated by use of a PSA hydrazide reagent as described in Step 1.
- rFIX concentration 1 mg/ml
- NaIO 4 concentration: 80 ⁇ M
- the reaction is stopped by addition of glycerol and the oxidized FIX is subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Vivaspin).
- the oxidized rFIX is then polysialylated at pH 6.5 using a 200-fold molar excess of reagent and a protein concentration of 1 mg/ml.
- rFIX and the polysialyation reagent are incubated for 2 hours under gentle shaking in the dark at room temperature. Finally, the PSA-rFIX conjugate is purified by HIC.
- the conductivity of the reaction mixture is raised to 130 mS/cm by adding a buffer containing ammonium acetate (50 mM Hepes, 350 mM NaCl, 5 mM Calcium chloride, 8M ammonium acetate, 0.0) % Tween 80, pH 6.9) and loaded onto a HiTrap Butyl FF column (5 ml, GE Healthcare, Fairfield, Conn.) pre-equilibrated with 50 mM Hepes, 2.5M ammonium acetate, 350 mM sodium chloride, 5 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- a buffer containing ammonium acetate 50 mM Hepes, 350 mM NaCl, 5 mM Calcium chloride, 8M ammonium a
- the conjugate is eluted with 50 mM Hepes, 5 mM calcium chloride, 0.01% Tween 80, pH 7.4. Finally the PSA-rFIX containing fractions are collected and subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Vivaspin). For the PEG-rFIX conjugate, a specific activity of >50% in comparison to native rFIX is determined (chromogenic assay).
- rFIX 123 mg rFIX are dissolved in 60 ml phosphate buffer (50 mM NaPO 4 , pH 6.5) buffer. Then 1.2 ml of an aqueous sodium periodate solution (10 mM) is added and the mixture is incubated for 1 h in the dark at 4° C. under gentle stirring. Subsequently the reaction is quenched for 15 min at RT by the addition of 600 ⁇ l of 1M aqueous glycerol solution. The mixture is subsequently subjected to UF/DF employing a Pellicon XL Ultracel 30 kD membrane.
- the UF/D F retentate (63.4 ml), containing oxidized rFIX, is further diluted with 59.6 ml phosphate buffer (50 mM NaPO 4 , pH 6.0) and mixed with 6.5 ml of an aqueous aniline solution (200 mM) and incubated for 30 min at RT. Then 12.3 ml of the PSA-hydrazide reagent (prepared according Example 16) is added to give a 5 fold molar reagent excess. This mixture is incubated for 2 h at RT in the dark under gentle stirring.
- the excess of the PSA-hydrazide reagent and free rFIX is removed by means of HIC.
- the conductivity of the reaction mixture is raised to 180 mS/cm and loaded onto a column filled with 48 ml Butyl-Sepharose FF (GE Healthcare, Fairfield, Conn.) pre-equilibrated with 50 mM Hepes, 3M sodium chloride, 6.7 mM calcium chloride, 0.01% Tween 80, pH 6.9. Subsequently the conjugate is eluted with 50 mM Hepes, 5 mM calcium chloride, 0.01% Tween 80, pH 7.4.
- PSA-rFIX containing fractions are collected and subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Millipore).
- the preparation is analytically characterized by measuring total protein (BCA) and FIX chromogenic activity.
- BCA total protein
- FIX chromogenic activity For the PSA-rFIX conjugate a specific activity of >50% in comparison to native rFIX is determined.
- rFIX 140 mg rFIX was dissolved in 62 ml phosphate buffer (50 mM NaPO 4 , pH 6.0) buffer. Then 1.92 ml of an aqueous sodium periodate solution (10 mM) were added and the mixture was incubated for 1 h in the dark at 4° C. under gentle stirring and quenched for 15 min at RT by the addition of 64 ⁇ l of an 1M aqueous glycerol solution. Subsequently the mixture was subjected to UF/DF employing a Pellicon XL Ultracel 30 kD membrane.
- the free rFIX is removed by means of anion exchange chromatography (AIEC).
- the reaction mixture is diluted with 20 ml Buffer A (50 mM Hepes, 5 mM CaCl 2 , pH 7.5) and loaded onto a Q-Sepharose FF 26/10 column (GE Healthcare, Fairfield, Conn.) pre-equilibrated with Buffer A. Then the column is eluted with Buffer B (50 mM Hepes, 1M NaCl, 5 mM CaCl 2 , pH 7.5). Free rFIX elutes at a conductivity between 12-25 mS/cm and the conjugate between 27-45 mS/cm.
- the conductivity of the conjugate containing fractions are subsequently raised to 190 mS/cm by addition of Buffer C (50 mM Hepes, 5M NaCl, 5 mM CaCl 2 , pH 6.9) and loaded onto a Butyl Sepharose FF 26/10 column (GE Healthcare, Fairfield, Conn.) pre-equilibrated with Buffer D (50 mM Hepes, 3M NaCl, 5 mM CaCl 2 , pH 6.9). Free PSA-reagent is washed out within 5 CV Buffer D. Subsequently the conjugate is eluted with 100% Buffer E (50 mM Hepes, 5 mM CaCl 2 , pH 7.4).
- Buffer C 50 mM Hepes, 5M NaCl, 5 mM CaCl 2 , pH 6.9
- Buffer D 50 mM Hepes, 3M NaCl, 5 mM CaCl 2 , pH 6.9
- the conjugate containing fractions are concentrated by UF/DF using a 10 kD membrane made of regenerated cellulose (88 cm 2 , cut-off 10 kD/Millipore).
- the final diafiltration step is performed against histidine buffer, pH 7.2 containing 150 mM NaCl and 5 mM CaCl 2 .
- the preparation is analytically characterized by measuring total protein (BCA) and FIX chromogenic activity. For the PSA-rFIX conjugate a specific activity of >50% in comparison to native rFIX is determined.
- a solution of 10 mg rFVIIa in 5 ml reaction buffer (50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0) is mixed with an aqueous solution of NaIO 4 (final concentration: 100 ⁇ M) and incubated for 1 h at 4° C. under gentle stirring in the dark and quenched by the addition of an aqueous solution of cysteine (final concentration: 1 mM) for 15 min.
- the reaction mixture is subsequently subjected to UF/DF.
- a 30 fold molar excess of Aminooxy reagent (prepared according to Example 1) is added. The coupling reaction is performed for 2 hours at room temperature in the dark under gentle shaking.
- the excess of aminooxy reagent is removed by HIC.
- the conductivity of the reaction mixture is raised to 130 mS/cm by adding a buffer containing ammonium acetate (50 mM Hepes, 350 mM NaCl, 5 mM Calcium chloride, 8 M ammonium acetate, 0.01% Tween 80, pH 6.9) and loaded onto a HiTrap Butyl FF column (5 ml, GE Healthcare, Fairfield, Conn.) pre-equilibrated with 50 mM Hepes, 2.5 M ammonium acetate, 350 mM sodium chloride, 5 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- a buffer containing ammonium acetate 50 mM Hepes, 350 mM NaCl, 5 mM Calcium chloride, 8 M ammonium acetate, 0.01% Tween 80, pH 6.9
- HiTrap Butyl FF column 5 ml, GE Healthcare, Fairfield, Conn
- the conjugate is eluted with 50 mM Hepes, 5 mM calcium chloride, 0.01% Tween 80, pH 7.4 by a linear gradient of 100% elution buffer in 20 CV.
- the PSA-rFVIIa containing fractions are collected and subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Vivaspin).
- the preparation is analytically characterized by measuring total protein (BCA) and FVIIa chromogenic activity (Staclot assay, Diagnostica Stago, Asnieres, France) and shows a specific activity of >20% compared to the rFVIIa starting material.
- the conductivity of the cooled reaction mixture is raised to 180 mS/cm and loaded onto a 5 ml HiTrap Butyl FF (GE Healthcare, Fairfield, Conn.) HOC column (1.6 ⁇ 2.5 cm), pre-equilibrated with 50 mM Hepes, 3M sodium chloride, 6.7 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- the conjugate is eluted with a linear gradient to 50 mM HEPES, 6.7 mM calcium chloride, 0.005% Tween 80, pH 7.4 in 20 CV with at a flow rate of 5 ml/min.
- a branched PEG-aldehyde (MW 40 kD) is used for coupling to the diaminooxy linker, which is prepared as described in Example 1.
- This PEG-aldehyde reagent is available from NOF (NOF Corp., Tokyo, Japan). 500 mg of PEG-aldehyde is dissolved in 8 ml 50 mM sodium acetate buffer, pH 5.5. Then 100 mg 3-oxa-pentane-1,5-dioxyamine is added. After shaking for 2 hrs at room temperature, 44 mg sodium cyanoborohydride is added.
- reaction mix After shaking for another 4 hrs at 4° C., the reaction mix is loaded into a Slide-A-Lyzer (Pierce, Rockford, Ill.) dialysis cassette (3.5 kD membrane, regenerated cellulose) and dialyzed against PBS pH 7.2 for 4 days. The product is frozen at ⁇ 80° C.
- rFIX is PEGylated by use of a linear 20 kD PEGylation reagent containing an aminooxy group.
- An example of this type of reagent is the Sunbright® CA series from NOF (NOF Corp., Tokyo, Japan).
- rFIX is oxidized at a protein concentration of 2 mg/ml with NaIO 4 (final: concentration: 100 ⁇ M) for 1 hour under gentle shaking in the dark at 4° C. in reaction buffer (50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0) and quenched by the addition of an aqueous solution of glycerol (final concentration: 1 mM) for 15 min.
- reaction mixture is subsequently subjected to UF/DF.
- rFVIII is PEGylated by use of a linear 20 kD PEGylation reagent containing an aminooxy group.
- An example of this type of reagent is the Sunbright® CA series from NOF (NOF Corp., Tokyo, Japan).
- rFVIII is oxidized at a protein concentration of 1 mg/ml with NaIO 4 (final: concentration: 100 ⁇ M) for 1 hour under gentle shaking in the dark at 4° C. in reaction buffer (50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0) and quenched by the addition of an aqueous solution of cysteine (final concentration: 1 mM) for 15 min.
- the reaction mixture is subsequently subjected to UF/DF.
- the conjugate is eluted with 50 mM Hepes buffer containing 5 mM CaCl 2 and 500 mM sodium chloride, pH 7.4 and is then subjected to UF/DF using a 30 kD membrane.
- the analytical characterization of the conjugate by FVIII chromogenic assay and determination of total protein (BCA assay) shows a specific activity of >60% compared to the rFVIII starting material.
- rFVIIa is PEGylated by use of a linear 20 kD PEGylation reagent containing an aminooxy group.
- An example of this type of reagent is the Sunbright® CA series from NOF (NOF Corp., Tokyo, Japan).
- rFVIIa is oxidized at a protein concentration of 2 mg/ml with NaIO 4 (final: concentration: 100 ⁇ M) for 1 hour under gentle shaking in the dark at 4° C. in reaction buffer (50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0) and quenched by the addition of an aqueous solution of glycerol (final concentration: 1 mM) for 15 min.
- reaction mixture is subsequently subjected to UF/DF.
- a 5 fold molar excess of Aminooxy reagent and aniline (a nucleophilic catalyst, final concentration: 10 mM) are added.
- the coupling reaction is performed for 2 hours at room temperature in the dark under gentle shaking.
- the PEG-rFVIIa conjugate is purified by ion-exchange chromatography on Q-Sepharose FF. 1.5 mg protein/ml gel is loaded on the column pre equilibrated with 20 mM Hepes buffer containing 1 mM CaCl 2 , pH 7.4.
- the conjugate is eluted with 20 mM Hepes buffer containing 1 mM CaCl 2 and 500 mM sodium chloride, pH 7.4 and is then subjected to UF/DF using a 30 kD membrane.
- the analytical characterization of the conjugate by measuring FVIIa activity shows a specific activity of >25% compared to the rFVIIa starting material.
- rFIX is PEGylated by use of a linear 20 kD PEGylation reagent containing a hydrazide group.
- An example of this type of reagent is the Sunbright® HZ series from NOF (NOF Corp., Tokyo, Japan).
- rFIX is oxidized at a protein concentration of 2 mg/ml with NaIO 4 (final: concentration: 100 ⁇ M) for 1 hour under gentle shaking in the dark at 4° C. in reaction buffer (50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0) and quenched by the addition of an aqueous solution of glycerol (final concentration: 1 mM) for 15 min.
- the reaction mixture is subsequently subjected to UF/DF.
- a 50 fold molar excess of Hydrazide reagent and aniline (a nucleophilic catalyst, final concentration: 10 mM) are added.
- the coupling reaction is performed for 2 hours at room temperature in the dark under gentle shaking.
- the PEG-rFIX conjugate is purified by ion-exchange chromatography on Q-Sepharose FF.
- the reaction mixture is loaded onto the column (1.5 mg protein/ml gel), which is preequilibrated with 50 mM Tris-buffer, pH 8.0.
- the conjugate is eluted with 20 CV Tris-buffer, pH 8.0 (50 mM Tris,) M NaCl) and is then subjected to UF/DF using a 30 kD membrane.
- the preparation is analytically characterized by measuring total protein (BCA) and FIX chromogenic activity.
- BCA total protein
- FIX FIX chromogenic activity
- reaction buffer 50 mM Hepes, 350 mM sodium chloride, 5 mM calcium chloride, 0.01% Tween 80, pH 6
- reaction buffer 50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0
- reaction buffer 50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0
- an aqueous solution of cysteine final concentration: 1 mM
- the conductivity of the reaction mixture is raised to 130 mS/cm by adding a buffer containing ammonium acetate (50 mM Hepes, 350 mM sodium chloride, 5 mM calcium chloride, 8 M ammonium acetate, 0.01% Tween 80, pH 6.9) and loaded onto a column filled with 53 ml Butyl-Sepharose FF (GE Healthcare, Fairfield, Conn.) pre-equilibrated with 50 mM Hepes, 2.5 M ammonium acetate, 350 mM sodium chloride, 5 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- a buffer containing ammonium acetate 50 mM Hepes, 350 mM sodium chloride, 5 mM calcium chloride, 8 M ammonium acetate, 0.01% Tween 80, pH 6.9
- the conjugate is eluted with 50 mM Hepes, 5 mM calcium chloride, 0.01% Tween 80, pH 7.4.
- the PSA-rFIX containing fractions are collected and subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Millipore, Billerica, Mass.).
- the preparation is analytically characterized by measuring total protein (BCA) and FVIII chromogenic activity.
- BCA total protein
- FVIII chromogenic activity For the PSA-rFVIII conjugate a specific activity of 80% in comparison to native rFVIII is determined.
- reaction buffer 50 mM Hepes, 350 mM sodium chloride, 5 mM calcium chloride, 0.01% Tween 80, pH 6
- reaction buffer 50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0
- reaction buffer 50 mM Hepes, 150 mM sodium chloride, 5 mM calcium chloride, pH 6.0
- an aqueous solution of cysteine final concentration: 1 mM
- the conductivity of the reaction mixture is raised to 130 mS/cm by adding a buffer containing ammonium acetate (50 mM Hepes, 350 mM sodium chloride, 5 mM calcium chloride, 8 M ammonium acetate, 0.01% Tween 80, pH 6.9) and loaded onto a column filled with 53 ml Butyl-Sepharose FF (GE Healthcare, Fairfield, Conn.) pre-equilibrated with 50 mM Hepes, 2.5 M ammonium acetate, 350 mM sodium chloride, 5 mM calcium chloride, 0.01% Tween 80, pH 6.9.
- a buffer containing ammonium acetate 50 mM Hepes, 350 mM sodium chloride, 5 mM calcium chloride, 8 M ammonium acetate, 0.01% Tween 80, pH 6.9
- the conjugate is eluted with 50 mM Hepes, 5 mM calcium chloride, 0.01% Tween 80, pH 7.4.
- the PSA-rFIX containing fractions are collected and subjected to UF/DF by use of a 30 kD membrane made of regenerated cellulose (Millipore, Billerica, Mass.).
- the preparation is analytically characterized by measuring total protein (BCA) and FVIII chromogenic activity.
- BCA total protein
- FVIII chromogenic activity For the PSA-rFVIII conjugate a specific activity of 80% in comparison to native rFVIII is determined.
- PEGylation of a blood coagulation proteins may be extended to a branched or linear PEGylation reagent as described in Example 21, which is made of an aldehyde and a suitable linker containing an active aminooxy group.
Abstract
Description
-
- wherein the aminooxy linker is selected from the group consisting of:
- a 3-oxa-pentane-1,5-dioxyamine linker of the formula:
-
-
- and
- a 3,6,9-trioxa-undecane-1,1′-dioxyamine linker of the formula:
-
-
- and
- a 3,6,9-trioxa-undecane-1,1)-dioxyamine linker of the formula:
| CONSERVATIVE SUBSTITUTIONS |
| SIDE CHAIN | |||
| CHARACTERISTIC | AMINO ACID | ||
| Non-polar (hydrophobic): | |||
| A. Aliphatic | A L I V P | ||
| B. Aromatic | F W | ||
| C. Sulfur-containing | M | ||
| D. Borderline | G | ||
| Uncharged-polar: | |||
| A. Hydroxyl | S T Y | ||
| B. Amides | N Q | ||
| C. Sulfhydryl | C | ||
| D. Borderline | G | ||
| Positively charged (basic) | K R H | ||
| Negatively charged (acidic) | D E | ||
| CONSERVATIVE SUBSTITUTIONS II |
| EXEMPLARY | |||
| ORIGINAL RESIDUE | SUBSTITUTION | ||
| Ala (A) | Val, Leu, Ile | ||
| Arg (R) | Lys, Gln, Asn | ||
| Asn (N) | Gln, His, Lys, Arg | ||
| Asp (D) | Glu | ||
| Cys (C) | Ser | ||
| Gln (Q) | Asn | ||
| Glu (E) | Asp | ||
| His (H) | Asn, Gln, Lys, Arg | ||
| Ile (I) | Leu, Val, Met, Ala, Phe, | ||
| Leu (L) | Ile, Val, Met, Ala, Phe | ||
| Lys (K) | Arg, Gln, Asn | ||
| Met (M) | Leu, Phe, Ile | ||
| Phe (F) | Leu, Val, Ile, Ala | ||
| Pro (P) | Gly | ||
| Ser (S) | Thr | ||
| Thr (T) | Ser | ||
| Trp (W) | Tyr | ||
| Tyr (Y) | Trp, Phe, Thr, Ser | ||
| Val (V) | Ile, Leu, Met, Phe, Ala | ||
| TABLE 1 | ||||
| Specific | ||||
| BCA | FIX:Chrom | Specific Activity | Activity | |
| Item | [mg/ml] | [IU/ml] | [IU FIX:Chrom/mg BCA | [%] |
| rFIX | 8.58 | 1221 | 142.3 | 100 |
| PSA-rFIX | 1.15 | 92.2 | 80.2 | 56.4 |
| TABLE 2 | |||||||
| In vivo | |||||||
| recovery | AUC | Increase | Terminal | Increase | Increase | ||
| Item | [%] | [(IU/ml)/(IU/kg)] | factor | HL [h] | factor | MRT [h] | factor |
| rFIX | 13 | 0.0100 | =1 | 8.0 | =1 | 7.3 | =1 |
| PSA-rFIX | 29 | 0.0650 | 6.4x | 9.6 | 1.2x | 12.3 | 1.7x |
| TABLE 3 | |||||
| In vivo | AUC 0-24 | Terminal | Mean | ||
| recovery | (IU/ml · h)/ | half- | residence time | Clearance CL | |
| Item | IVR % | IU/kg | life (h) | MRT (h) | (ml/h/kg) |
| PSA- |
71 | 0.161 | 7.2 | 11.1 | 6.0 |
| rFVIII control | 58 | 0.054 | 4.4 | 5.4 | 17.1 |
| (Advate) | |||||
Claims (9)
Priority Applications (17)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| KR1020127003344A KR101759300B1 (en) | 2009-07-27 | 2010-07-26 | Glycopolysialylation of non-blood coagulation proteins |
| KR1020127003964A KR101832937B1 (en) | 2009-07-27 | 2010-07-26 | Blood coagulation protein conjugates |
| US12/843,542 US8637640B2 (en) | 2009-07-27 | 2010-07-26 | Blood coagulation protein conjugates |
| US13/194,038 US8642737B2 (en) | 2010-07-26 | 2011-07-29 | Nucleophilic catalysts for oxime linkage |
| US13/329,002 US8945897B2 (en) | 2010-07-26 | 2011-12-16 | Materials and methods for conjugating a water soluble fatty acid derivative to a protein |
| US13/488,043 US8809501B2 (en) | 2009-07-27 | 2012-06-04 | Nucleophilic catalysts for oxime linkage |
| US14/136,233 US9492555B2 (en) | 2009-07-27 | 2013-12-20 | Nucleophilic catalysts for oxime linkage |
| US14/136,266 US20140107320A1 (en) | 2009-07-27 | 2013-12-20 | Blood coagulation protein conjugates |
| US14/333,824 US9731024B2 (en) | 2009-07-27 | 2014-07-17 | Nucleophilic catalysts for oxime linkage |
| US14/988,931 US20160120994A1 (en) | 2009-07-27 | 2016-01-06 | Blood coagulation protein conjugates |
| US15/249,657 US10350301B2 (en) | 2009-07-27 | 2016-08-29 | Blood coagulation protein conjugates |
| US15/281,616 US10414793B2 (en) | 2009-07-27 | 2016-09-30 | Nucleophilic catalysts for oxime linkage |
| US15/644,129 US10576160B2 (en) | 2009-07-27 | 2017-07-07 | Nucleophilic catalysts for oxime linkage |
| US16/447,134 US11040109B2 (en) | 2009-07-27 | 2019-06-20 | Blood coagulation protein conjugates |
| US16/532,212 US20200017543A1 (en) | 2009-07-27 | 2019-08-05 | Nucleophilic catalysts for oxime linkage |
| US16/748,296 US11564992B2 (en) | 2009-07-27 | 2020-01-21 | Nucleophilic catalysts for oxime linkage |
| US17/168,695 US20210163527A1 (en) | 2009-07-27 | 2021-02-05 | Nucleophilic catalysts for oxime linkage |
Applications Claiming Priority (4)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US22882809P | 2009-07-27 | 2009-07-27 | |
| US34713610P | 2010-05-21 | 2010-05-21 | |
| US12/843,542 US8637640B2 (en) | 2009-07-27 | 2010-07-26 | Blood coagulation protein conjugates |
| PCT/US2010/043242 WO2011017055A2 (en) | 2009-07-27 | 2010-07-26 | Blood coagulation protein conjugates |
Related Child Applications (3)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US13/194,038 Continuation-In-Part US8642737B2 (en) | 2009-07-27 | 2011-07-29 | Nucleophilic catalysts for oxime linkage |
| US13/329,002 Continuation-In-Part US8945897B2 (en) | 2010-07-26 | 2011-12-16 | Materials and methods for conjugating a water soluble fatty acid derivative to a protein |
| US14/136,266 Continuation US20140107320A1 (en) | 2009-07-27 | 2013-12-20 | Blood coagulation protein conjugates |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| US20110028693A1 US20110028693A1 (en) | 2011-02-03 |
| US8637640B2 true US8637640B2 (en) | 2014-01-28 |
Family
ID=46582462
Family Applications (3)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US12/843,542 Active 2031-02-15 US8637640B2 (en) | 2009-07-27 | 2010-07-26 | Blood coagulation protein conjugates |
| US14/136,266 Abandoned US20140107320A1 (en) | 2009-07-27 | 2013-12-20 | Blood coagulation protein conjugates |
| US14/988,931 Abandoned US20160120994A1 (en) | 2009-07-27 | 2016-01-06 | Blood coagulation protein conjugates |
Family Applications After (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US14/136,266 Abandoned US20140107320A1 (en) | 2009-07-27 | 2013-12-20 | Blood coagulation protein conjugates |
| US14/988,931 Abandoned US20160120994A1 (en) | 2009-07-27 | 2016-01-06 | Blood coagulation protein conjugates |
Country Status (22)
| Country | Link |
|---|---|
| US (3) | US8637640B2 (en) |
| EP (1) | EP2459224B1 (en) |
| JP (1) | JP5908401B2 (en) |
| KR (3) | KR101832937B1 (en) |
| CN (1) | CN102497884A (en) |
| AR (1) | AR077600A1 (en) |
| AU (1) | AU2010281453C1 (en) |
| BR (1) | BR112012001814A8 (en) |
| CA (1) | CA2769326A1 (en) |
| CY (1) | CY1117880T1 (en) |
| DK (1) | DK2459224T3 (en) |
| ES (1) | ES2597954T3 (en) |
| GB (1) | GB2472303A (en) |
| HK (1) | HK1171691A1 (en) |
| HR (1) | HRP20160916T1 (en) |
| MX (1) | MX2012001207A (en) |
| NZ (1) | NZ598056A (en) |
| RU (1) | RU2595442C2 (en) |
| SG (1) | SG178141A1 (en) |
| SM (1) | SMT201600314B (en) |
| TW (1) | TWI537006B (en) |
| WO (1) | WO2011017055A2 (en) |
Cited By (5)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| WO2017096383A1 (en) | 2015-12-03 | 2017-06-08 | Baxalta Incorporated | Factor viii with extended half-life and reduced ligand-binding properties |
| US10350301B2 (en) * | 2009-07-27 | 2019-07-16 | Baxalta Incorporated | Blood coagulation protein conjugates |
| US11767526B2 (en) | 2019-01-23 | 2023-09-26 | Regeneron Pharmaceuticals, Inc. | Treatment of ophthalmic conditions with angiopoietin-like 7 (ANGPTL7) inhibitors |
| US11845989B2 (en) | 2019-01-23 | 2023-12-19 | Regeneron Pharmaceuticals, Inc. | Treatment of ophthalmic conditions with angiopoietin-like 7 (ANGPTL7) inhibitors |
| US11865134B2 (en) | 2021-02-26 | 2024-01-09 | Regeneron Pharmaceuticals, Inc. | Treatment of inflammation with glucocorticoids and angiopoietin-like 7 (ANGPTL7) inhibitors |
Families Citing this family (17)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| CN101557830B (en) | 2006-12-15 | 2016-06-08 | 巴克斯特国际公司 | There is the factor VIIa-Polysialic acid conjugate of the Half-life in vivo of prolongation |
| KR101832937B1 (en) | 2009-07-27 | 2018-02-28 | 박스알타 인코퍼레이티드 | Blood coagulation protein conjugates |
| US8809501B2 (en) | 2009-07-27 | 2014-08-19 | Baxter International Inc. | Nucleophilic catalysts for oxime linkage |
| US8642737B2 (en) | 2010-07-26 | 2014-02-04 | Baxter International Inc. | Nucleophilic catalysts for oxime linkage |
| RU2533619C2 (en) | 2009-07-27 | 2014-11-20 | Лайпоксен Текнолоджиз Лимитед | Glycopolysialylation of proteins, which are not blood clotting proteins |
| PL2536399T3 (en) * | 2010-02-21 | 2020-06-29 | Bayer Healthcare Llc | Method for activation and conjugation of biomolecules |
| EP4023247A1 (en) * | 2010-07-30 | 2022-07-06 | Takeda Pharmaceutical Company Limited | Nucleophilic catalysts for oxime linkage |
| AU2015275284C1 (en) * | 2010-07-30 | 2018-04-05 | Takeda Pharmaceutical Company Limited | Nucleophilic Catalysts for Oxime Linkage |
| TR201904997T4 (en) | 2011-05-18 | 2019-05-21 | Baxalta GmbH | Activity assays due to modification. |
| NZ628014A (en) * | 2012-02-15 | 2016-09-30 | Biogen Ma Inc | Recombinant factor viii proteins |
| MY190257A (en) * | 2012-04-16 | 2022-04-11 | Cantab Biopharmaceuticals Patents Ltd | Optimised subcutaneous therapeutic agents |
| AU2013204754C1 (en) * | 2012-05-16 | 2018-10-11 | Takeda Pharmaceutical Company Limited | Nucleophilic Catalysts for Oxime Linkage |
| EP2828088B1 (en) | 2012-07-03 | 2020-05-27 | Hewlett-Packard Development Company, L.P. | Fluid ejection apparatus |
| CN105801870B (en) * | 2016-04-08 | 2018-08-21 | 北京华熙海御科技有限公司 | The preparation method and products obtained therefrom of a kind of poly sialic acid-hyaluronic acid plural gel and application |
| CN109475639A (en) * | 2016-07-22 | 2019-03-15 | 尼克塔治疗公司 | Conjugates with the bonded Factor VIB moiety containing oxime |
| KR20190086269A (en) * | 2018-01-12 | 2019-07-22 | 재단법인 목암생명과학연구소 | Long-acting recombinant glycoproteins and menufacturing method thereof |
| CN111450080A (en) * | 2020-03-31 | 2020-07-28 | 天津大学 | Synthesis method of IgA nephropathy treatment nano preparation |
Citations (114)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4179337A (en) * | 1973-07-20 | 1979-12-18 | Davis Frank F | Non-immunogenic polypeptides |
| US4757006A (en) | 1983-10-28 | 1988-07-12 | Genetics Institute, Inc. | Human factor VIII:C gene and recombinant methods for production |
| EP0306968A2 (en) | 1987-09-10 | 1989-03-15 | Juridical Foundation The Chemo-Sero-Therapeutic Research Institute | Process for producing recombinant human factor VIII:C |
| US4966999A (en) | 1988-06-07 | 1990-10-30 | Cytogen Corporation | Radiohalogenated compounds for site specific labeling |
| US4970300A (en) | 1985-02-01 | 1990-11-13 | New York University | Modified factor VIII |
| WO1991009122A1 (en) | 1989-12-15 | 1991-06-27 | Kabivitrum Ab | A recombinant human factor viii derivative |
| US5122614A (en) * | 1989-04-19 | 1992-06-16 | Enzon, Inc. | Active carbonates of polyalkylene oxides for modification of polypeptides |
| WO1992016555A1 (en) | 1991-03-18 | 1992-10-01 | Enzon, Inc. | Hydrazine containing conjugates of polypeptides and glycopolypeptides with polymers |
| US5153265A (en) | 1988-01-20 | 1992-10-06 | Cetus Corporation | Conjugation of polymer to colony stimulating factor-1 |
| US5198493A (en) | 1990-09-13 | 1993-03-30 | Berol Nobel Ab | Method of covalently bonding biopolymer to a solid hydrophilic organic polymer |
| US5198349A (en) | 1986-01-03 | 1993-03-30 | Genetics Institute, Inc. | Method for producing factor VIII:C and analogs |
| US5250421A (en) | 1986-01-03 | 1993-10-05 | Genetics Institute, Inc. | Method for producing factor VIII:C-type proteins |
| WO1994005332A2 (en) | 1992-09-01 | 1994-03-17 | Berlex Laboratories, Inc. | Glycolation of glycosylated macromolecules |
| US5298643A (en) * | 1992-12-22 | 1994-03-29 | Enzon, Inc. | Aryl imidate activated polyalkylene oxides |
| EP0605963A2 (en) | 1992-12-09 | 1994-07-13 | Ortho Pharmaceutical Corporation | Peg hydrazone and peg oxime linkage forming reagents and protein derivatives thereof |
| WO1994015625A1 (en) * | 1993-01-15 | 1994-07-21 | Enzon, Inc. | Factor viii - polymeric conjugates |
| WO1994028024A1 (en) | 1993-06-01 | 1994-12-08 | Enzon, Inc. | Carbohydrate-modified polymer conjugates with erythropoietic activity |
| WO1994029370A1 (en) | 1993-06-08 | 1994-12-22 | Enzon, Inc. | Factor ix - polymeric conjugates |
| WO1995001804A1 (en) | 1993-07-05 | 1995-01-19 | Pharmacia Ab | A coagulation factor viii formulation |
| US5492821A (en) | 1990-11-14 | 1996-02-20 | Cargill, Inc. | Stabilized polyacrylic saccharide protein conjugates |
| WO1996040731A1 (en) | 1995-06-07 | 1996-12-19 | Mount Sinai School Of Medicine Of The City University Of New York | Pegylated modified proteins |
| WO1996041813A2 (en) | 1994-11-09 | 1996-12-27 | Offord Robin E | Functionalized polymers for site-specific attachment |
| WO1997011957A1 (en) | 1995-09-29 | 1997-04-03 | Pharmacia & Upjohn Ab | Conjugates of a polypeptide and a biocompatible polymer |
| US5733873A (en) | 1992-10-02 | 1998-03-31 | Pharmacia & Upjohn Ab | Composition comprising coagulation factor VIII formulation, process for its preparation and use of a surfactant as stabilizer |
| WO1999028455A1 (en) | 1997-12-03 | 1999-06-10 | Roche Diagnostics Gmbh | Method for preparing polypeptides with appropriate glycosilation |
| WO1999032134A1 (en) | 1997-12-19 | 1999-07-01 | Enzon, Inc. | Substantially pure histidine-linked protein polymer conjugates |
| WO2000012587A2 (en) | 1998-08-28 | 2000-03-09 | Gryphon Sciences | Polyamide chains of precise length, methods to manufacture them and their conjugates |
| US6037452A (en) * | 1992-04-10 | 2000-03-14 | Alpha Therapeutic Corporation | Poly(alkylene oxide)-Factor VIII or Factor IX conjugate |
| WO2000023114A2 (en) | 1998-10-16 | 2000-04-27 | Biogen, Inc. | Polymer conjugates of interferon beta- 1a and their uses |
| WO2000048635A1 (en) | 1999-02-22 | 2000-08-24 | Baxter International Inc. | Novel albumin-free factor viii formulations |
| US6183738B1 (en) | 1997-05-12 | 2001-02-06 | Phoenix Pharamacologics, Inc. | Modified arginine deiminase |
| WO2001083725A1 (en) | 2000-05-03 | 2001-11-08 | Novo Nordisk A/S | Human coagulation factor vii variants |
| WO2001082943A2 (en) | 2000-05-03 | 2001-11-08 | Novo Nordisk A/S | Subcutaneous administration of coagulation factor vii |
| WO2002002764A2 (en) | 2000-06-30 | 2002-01-10 | Regents Of The University Of Minnesota | High molecular weight derivatives of vitamin k-dependent polypeptides |
| WO2002022776A2 (en) | 2000-09-13 | 2002-03-21 | Novo Nordisk A/S | Human coagulation factor vii variants |
| WO2002029025A2 (en) | 2000-10-02 | 2002-04-11 | Novo Nordisk A/S | Factor vii glycoforms |
| US20020110535A1 (en) | 2000-06-08 | 2002-08-15 | Jones David S. | Multivalent platform molecules comprising high molecular weight polyethylene oxide |
| WO2002077218A1 (en) | 2001-03-22 | 2002-10-03 | Novo Nordisk Health Care Ag | Coagulation factor vii derivatives |
| WO2003031464A2 (en) | 2001-10-10 | 2003-04-17 | Neose Technologies, Inc. | Remodeling and glycoconjugation of peptides |
| WO2003046150A2 (en) | 2001-11-28 | 2003-06-05 | Neose Technologies, Inc. | Glycoprotein remodeling using endoglycanases |
| WO2003045980A2 (en) | 2001-11-28 | 2003-06-05 | Neose Technologies, Inc. | Glycopeptide remodeling using amidases |
| US6586398B1 (en) | 2000-04-07 | 2003-07-01 | Amgen, Inc. | Chemically modified novel erythropoietin stimulating protein compositions and methods |
| US20030143596A1 (en) | 2001-11-07 | 2003-07-31 | Shearwater Corporation | Branched polymers and their conjugates |
| WO2004000366A1 (en) | 2002-06-21 | 2003-12-31 | Novo Nordisk Health Care Ag | Pegylated factor vii glycoforms |
| US6692931B1 (en) | 1998-11-16 | 2004-02-17 | Werner Reutter | Recombinant glycoproteins, method for the production thereof, medicaments containing said glycoproteins and use thereof |
| WO2004014424A1 (en) | 2002-08-13 | 2004-02-19 | Enzon, Inc. | Releasable polymeric conjugates based on aliphatic biodegradable linkers |
| US20040063911A1 (en) | 2001-10-10 | 2004-04-01 | Neose Technologies, Inc. | Protein remodeling methods and proteins/peptides produced by the methods |
| WO2004030617A2 (en) | 2002-09-30 | 2004-04-15 | Mountain View Pharmaceuticals, Inc. | Polymer conjugates with decreased antigenicity, methods of preparation and uses thereof |
| US6743908B2 (en) | 1997-04-30 | 2004-06-01 | Enzon, Inc. | Single-chain antigen-binding proteins capable of glycosylation, production and uses thereof |
| WO2004060965A2 (en) | 2002-12-31 | 2004-07-22 | Nektar Therapeutics Al, Corporation | Hydrolytically stable maleimide-terminated polymers |
| WO2004075923A2 (en) | 2003-02-26 | 2004-09-10 | Nektar Therapeutics Al, Corporation | Polymer-factor viii moiety conjugates |
| US6806063B2 (en) | 2000-02-11 | 2004-10-19 | Maxygen Aps | Factor VII or VIIa-like molecules |
| WO2004089280A2 (en) | 2003-04-08 | 2004-10-21 | Yeda Research And Development Co. Ltd. | Reversible pegylated drugs |
| WO2004108070A2 (en) | 2003-05-30 | 2004-12-16 | Enzon, Inc. | Releasable polymeric conjugates based on aliphatic biodegradable linkers |
| WO2005014035A2 (en) | 2003-08-08 | 2005-02-17 | Novo Nordisk Health Care Ag | Use of galactose oxidase for selective chemical conjugation of protractor molecules to proteins of therapeutic interest |
| WO2005014024A2 (en) | 2003-08-08 | 2005-02-17 | Fresenius Kabi Deutschland Gmbh | Conjugates of a polymer and a protein linked by an oxime linking group |
| WO2005055950A2 (en) | 2003-12-03 | 2005-06-23 | Neose Technologies, Inc. | Glycopegylated factor ix |
| US6913915B2 (en) | 2001-08-02 | 2005-07-05 | Phoenix Pharmacologics, Inc. | PEG-modified uricase |
| WO2005070138A2 (en) | 2004-01-08 | 2005-08-04 | Neose Technologies, Inc. | O-linked glycosylation of peptides |
| US20060019877A1 (en) | 2002-09-11 | 2006-01-26 | Conradt Harald S | Hasylated polypeptides |
| WO2006013202A2 (en) | 2004-08-02 | 2006-02-09 | Novo Nordisk Health Care Ag | Conjugation of fvii |
| WO2006016168A2 (en) | 2004-08-12 | 2006-02-16 | Lipoxen Technologies Limited | Sialic acid derivatives |
| WO2006020372A2 (en) | 2004-07-23 | 2006-02-23 | Neose Technologies, Inc. | Enzymatic modification of glycopeptides |
| US20060088906A1 (en) | 2001-10-10 | 2006-04-27 | Neose Technologies, Inc. | Erythropoietin: remodeling and glycoconjugation of erythropoietin |
| WO2006053299A2 (en) | 2004-11-12 | 2006-05-18 | Bayer Healthcare Llc | Site-directed modification of fviii |
| WO2006071801A2 (en) | 2004-12-27 | 2006-07-06 | Baxter International Inc | Polymer-von willebrand factor-conjugates |
| WO2006074279A1 (en) | 2005-01-06 | 2006-07-13 | Neose Technologies, Inc. | Glycoconjugation using saccharyl fragments |
| US7118737B2 (en) | 2000-09-08 | 2006-10-10 | Amylin Pharmaceuticals, Inc. | Polymer-modified synthetic proteins |
| WO2006127896A2 (en) | 2005-05-25 | 2006-11-30 | Neose Technologies, Inc. | Glycopegylated factor ix |
| WO2006134173A2 (en) | 2005-06-17 | 2006-12-21 | Novo Nordisk Health Care Ag | Selective reduction and derivatization of engineered proteins comprising at least one non-native cysteine |
| US20060286634A1 (en) | 1997-06-04 | 2006-12-21 | Oxford Biomedica (Uk) Limited | Vector |
| WO2007022784A2 (en) | 2005-08-26 | 2007-03-01 | Maxygen Holdings Ltd. | Liquid factor vii composition |
| US7230081B1 (en) | 1999-11-12 | 2007-06-12 | Maxygen Holdings, Ltd. | Interferon gamma conjugates |
| WO2007076062A2 (en) | 2005-12-21 | 2007-07-05 | Wyeth | Protein formulations with reduced viscosity and uses thereof |
| US20070244301A1 (en) | 2006-03-31 | 2007-10-18 | Juergen Siekmann | Pegylated factor VIII |
| WO2007140282A1 (en) | 2006-05-24 | 2007-12-06 | Peg Biosciences | Peg linker compounds and biologically active conjugates thereof |
| WO2008012540A1 (en) | 2006-07-25 | 2008-01-31 | Lipoxen Technologies Limited | N-terminal polysialylation |
| US7338788B2 (en) | 1999-08-27 | 2008-03-04 | Maxygen Aps | Interferon-β variants and conjugates |
| WO2008025856A2 (en) | 2006-09-01 | 2008-03-06 | Novo Nordisk Health Care Ag | Modified glycoproteins |
| WO2008035373A2 (en) | 2006-07-13 | 2008-03-27 | Serum Institute Of India Ltd | Highly pure polysialic acid and process for preperation thereof |
| WO2008057683A2 (en) | 2006-10-03 | 2008-05-15 | Novo Nordisk A/S | Methods for the purification of polypeptide conjugates |
| US20080146771A1 (en) | 2002-12-31 | 2008-06-19 | Antoni Kozlowski | Maleamic acid polymer derivatives and their bioconjugates |
| WO2008074032A1 (en) | 2006-12-15 | 2008-06-19 | Baxter International Inc. | Factor viia- (poly) sialic acid conjugate having prolonged in vivo half-life |
| WO2008081024A1 (en) | 2007-01-03 | 2008-07-10 | Novo Nordisk Health Care Ag | Subcutaneous administration of coagulation factor viia-related popypeptdes |
| WO2008119815A1 (en) | 2007-04-02 | 2008-10-09 | Novo Nordisk A/S | Subcutaneous administration of coagulation factor ix |
| US20080260755A1 (en) | 2006-06-14 | 2008-10-23 | Hubert Metzner | Proteolytically cleavable fusion proteins with high molar specific activity |
| WO2009000522A1 (en) | 2007-06-26 | 2008-12-31 | Baxter International Inc. | Hydrolysable polymeric fmoc-linker |
| WO2009006620A1 (en) | 2007-07-03 | 2009-01-08 | Children's Hospital & Research Center At Oakland | Oligosialic acid derivatives, methods of manufacture, and immunological uses |
| US20090076237A1 (en) * | 2006-03-31 | 2009-03-19 | Baxter Healthcare S.A. | Factor VIII Polymer Conjugates |
| WO2009047500A1 (en) | 2007-10-09 | 2009-04-16 | Polytherics Limited | Novel conjugated proteins and peptides |
| WO2009089396A2 (en) | 2008-01-08 | 2009-07-16 | Neose Technologies, Inc. | Glycoconjugation of polypeptides using oligosaccharyltransferases |
| WO2009108806A1 (en) | 2008-02-27 | 2009-09-03 | Novo Nordisk A/S | Conjugated factor viii molecules |
| WO2009130602A2 (en) | 2008-04-24 | 2009-10-29 | Celtic Pharma Peg Ltd. | Factor ix conjugates with extended half-lives |
| WO2009141433A1 (en) | 2008-05-23 | 2009-11-26 | Novo Nordisk Health Care Ag | Low viscosity compositions comprising a pegylated gla-domain containing protein |
| WO2009141418A1 (en) | 2008-05-23 | 2009-11-26 | Novo Nordisk A/S | Formulations of peg-functionalised serine proteases with high concentrations of an aromatic preservative |
| WO2009149303A1 (en) | 2008-06-04 | 2009-12-10 | Bayer Healthcare Llc | Fviii muteins for treatment of von willebrand disease |
| WO2010010324A1 (en) | 2008-07-21 | 2010-01-28 | Polytherics Limited | Novel reagents and method for conjugating biological molecules |
| WO2010062768A1 (en) | 2008-11-03 | 2010-06-03 | Bayer Healthcare Llc | Method for the treatment of hemophilia |
| WO2010083536A1 (en) | 2009-01-19 | 2010-07-22 | Bayer Healthcare Llc | Protein conjugate having an endopeptidase-cleavable bioprotective moiety |
| WO2010100430A1 (en) | 2009-03-04 | 2010-09-10 | Polytherics Limited | Conjugated proteins and peptides |
| WO2010102886A1 (en) | 2009-02-19 | 2010-09-16 | Novo Nordisk A/S | Modification of factor viii |
| WO2010120365A2 (en) | 2009-04-16 | 2010-10-21 | Wu Nian | Protein-carrier conjugates |
| WO2010131015A1 (en) | 2009-05-15 | 2010-11-18 | Almac Sciences (Scotland) Limited | Method of labelling interferons with peg |
| WO2011012850A2 (en) | 2009-07-27 | 2011-02-03 | Lipoxen Technologies Limited | Glycopolysialylation of non-blood coagulation proteins |
| WO2011014890A1 (en) | 2009-07-31 | 2011-02-03 | Bayer Healthcare Llc | Modified factor ix polypeptides and uses thereof |
| WO2011017055A2 (en) | 2009-07-27 | 2011-02-10 | Baxter International Inc. | Blood coagulation protein conjugates |
| WO2011018496A2 (en) | 2009-08-13 | 2011-02-17 | Leibniz-Institut für Polymerforschung Dresden e. V. | Method for modifying and functionalizing saccharides |
| WO2011037896A2 (en) | 2009-09-25 | 2011-03-31 | Vybion, Inc. | Polypeptide modification |
| WO2011064247A1 (en) | 2009-11-24 | 2011-06-03 | Novo Nordisk Health Care Ag | Method of purifying pegylated proteins |
| WO2011101267A1 (en) | 2010-02-16 | 2011-08-25 | Novo Nordisk A/S | Conjugated fviii variants |
| WO2011135307A1 (en) | 2010-04-30 | 2011-11-03 | Leverton Licence Holdings Limited | Conjugated blood coagulation factor viii |
| WO2011135308A1 (en) | 2010-04-30 | 2011-11-03 | Leverton Licence Holdings Limited | Conjugated blood coagulation factor viia |
| WO2012068134A1 (en) | 2010-11-15 | 2012-05-24 | Biogen Idec Inc. | Enrichment and concentration of select product isoforms by overloaded bind and elute chromatography |
| WO2013009627A2 (en) | 2011-07-08 | 2013-01-17 | Biogen Idec Hemophilia Inc. | Factor viii chimeric and hybrid polypeptides, and methods of use thereof |
Family Cites Families (20)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| JPS54113492A (en) | 1978-02-24 | 1979-09-05 | Sanyo Chem Ind Ltd | Preparation of glucoprotein derivative |
| US4356170A (en) | 1981-05-27 | 1982-10-26 | Canadian Patents & Development Ltd. | Immunogenic polysaccharide-protein conjugates |
| US5846951A (en) | 1991-06-06 | 1998-12-08 | The School Of Pharmacy, University Of London | Pharmaceutical compositions |
| NO934477L (en) * | 1992-12-09 | 1994-06-10 | Ortho Pharma Corp | PEG hydrazone and PEG oxime-binding reagents and protein derivatives thereof |
| WO1996040662A2 (en) | 1995-06-07 | 1996-12-19 | Cellpro, Incorporated | Aminooxy-containing linker compounds and their application in conjugates |
| WO1999003496A1 (en) | 1997-07-21 | 1999-01-28 | The University Of North Carolina At Chapel Hill | Factor ix antihemophilic factor with increased clotting activity |
| US7074878B1 (en) | 1999-12-10 | 2006-07-11 | Harris J Milton | Hydrolytically degradable polymers and hydrogels made therefrom |
| US6413507B1 (en) | 1999-12-23 | 2002-07-02 | Shearwater Corporation | Hydrolytically degradable carbamate derivatives of poly (ethylene glycol) |
| US7265084B2 (en) | 2001-10-10 | 2007-09-04 | Neose Technologies, Inc. | Glycopegylation methods and proteins/peptides produced by the methods |
| EP1681303B1 (en) | 2002-09-11 | 2013-09-04 | Fresenius Kabi Deutschland GmbH | HASylated polypeptides, especially HASylated erythropoietin |
| KR101113726B1 (en) | 2003-08-12 | 2012-02-27 | 리폭센 테크놀로지즈 리미티드 | Sialic acid derivatives for protein derivatisation and conjugation |
| EP1654289B1 (en) | 2003-08-12 | 2007-10-03 | Lipoxen Technologies Limited | Polysialic acid derivatives |
| DK1653994T3 (en) * | 2003-08-12 | 2010-03-15 | Tigenix Nv | Use of CXCL6 chemokine in the prevention or recovery of cartilage defects |
| US8633157B2 (en) | 2003-11-24 | 2014-01-21 | Novo Nordisk A/S | Glycopegylated erythropoietin |
| US20060040856A1 (en) | 2003-12-03 | 2006-02-23 | Neose Technologies, Inc. | Glycopegylated factor IX |
| EP1694274B1 (en) | 2003-12-03 | 2013-04-24 | BioGeneriX AG | Glycopegylated granulocyte colony stimulating factor |
| US20060109877A1 (en) * | 2004-06-21 | 2006-05-25 | Caton John W | External cavity laser with adaptive fiber bragg grating (FBG) for minimizing noise related to stimulated brillouin scattering (SBS) in dispersive fiber links |
| CN101039965A (en) * | 2004-08-12 | 2007-09-19 | 利普生技术有限公司 | Sialic acid derivatives |
| WO2006031811A2 (en) | 2004-09-10 | 2006-03-23 | Neose Technologies, Inc. | Glycopegylated interferon alpha |
| RS53968B1 (en) | 2005-06-16 | 2015-08-31 | Nektar Therapeutics | Conjugates having a degradable linkage and polymeric reagents useful in preparing such conjugates |
-
2010
- 2010-07-26 KR KR1020127003964A patent/KR101832937B1/en active IP Right Grant
- 2010-07-26 DK DK10738119.6T patent/DK2459224T3/en active
- 2010-07-26 WO PCT/US2010/043242 patent/WO2011017055A2/en active Application Filing
- 2010-07-26 RU RU2012106589/15A patent/RU2595442C2/en not_active IP Right Cessation
- 2010-07-26 KR KR1020187005130A patent/KR102068133B1/en active IP Right Grant
- 2010-07-26 ES ES10738119.6T patent/ES2597954T3/en active Active
- 2010-07-26 GB GB1012482A patent/GB2472303A/en not_active Withdrawn
- 2010-07-26 KR KR1020127003344A patent/KR101759300B1/en active IP Right Grant
- 2010-07-26 AU AU2010281453A patent/AU2010281453C1/en active Active
- 2010-07-26 BR BR112012001814A patent/BR112012001814A8/en not_active Application Discontinuation
- 2010-07-26 US US12/843,542 patent/US8637640B2/en active Active
- 2010-07-26 NZ NZ598056A patent/NZ598056A/en unknown
- 2010-07-26 MX MX2012001207A patent/MX2012001207A/en active IP Right Grant
- 2010-07-26 CN CN2010800370028A patent/CN102497884A/en active Pending
- 2010-07-26 SG SG2012006094A patent/SG178141A1/en unknown
- 2010-07-26 CA CA2769326A patent/CA2769326A1/en not_active Abandoned
- 2010-07-26 EP EP10738119.6A patent/EP2459224B1/en active Active
- 2010-07-26 JP JP2012522940A patent/JP5908401B2/en active Active
- 2010-07-26 TW TW099124493A patent/TWI537006B/en active
- 2010-07-27 AR ARP100102720A patent/AR077600A1/en active IP Right Grant
-
2012
- 2012-12-06 HK HK12112611.0A patent/HK1171691A1/en unknown
-
2013
- 2013-12-20 US US14/136,266 patent/US20140107320A1/en not_active Abandoned
-
2016
- 2016-01-06 US US14/988,931 patent/US20160120994A1/en not_active Abandoned
- 2016-07-21 HR HRP20160916TT patent/HRP20160916T1/en unknown
- 2016-08-10 CY CY20161100787T patent/CY1117880T1/en unknown
- 2016-09-09 SM SM201600314T patent/SMT201600314B/en unknown
Patent Citations (127)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4179337A (en) * | 1973-07-20 | 1979-12-18 | Davis Frank F | Non-immunogenic polypeptides |
| US4757006A (en) | 1983-10-28 | 1988-07-12 | Genetics Institute, Inc. | Human factor VIII:C gene and recombinant methods for production |
| US4970300A (en) | 1985-02-01 | 1990-11-13 | New York University | Modified factor VIII |
| US5250421A (en) | 1986-01-03 | 1993-10-05 | Genetics Institute, Inc. | Method for producing factor VIII:C-type proteins |
| US5198349A (en) | 1986-01-03 | 1993-03-30 | Genetics Institute, Inc. | Method for producing factor VIII:C and analogs |
| EP0306968A2 (en) | 1987-09-10 | 1989-03-15 | Juridical Foundation The Chemo-Sero-Therapeutic Research Institute | Process for producing recombinant human factor VIII:C |
| US5153265A (en) | 1988-01-20 | 1992-10-06 | Cetus Corporation | Conjugation of polymer to colony stimulating factor-1 |
| US4966999A (en) | 1988-06-07 | 1990-10-30 | Cytogen Corporation | Radiohalogenated compounds for site specific labeling |
| US5122614A (en) * | 1989-04-19 | 1992-06-16 | Enzon, Inc. | Active carbonates of polyalkylene oxides for modification of polypeptides |
| WO1991009122A1 (en) | 1989-12-15 | 1991-06-27 | Kabivitrum Ab | A recombinant human factor viii derivative |
| US5198493A (en) | 1990-09-13 | 1993-03-30 | Berol Nobel Ab | Method of covalently bonding biopolymer to a solid hydrophilic organic polymer |
| US5492821A (en) | 1990-11-14 | 1996-02-20 | Cargill, Inc. | Stabilized polyacrylic saccharide protein conjugates |
| WO1992016555A1 (en) | 1991-03-18 | 1992-10-01 | Enzon, Inc. | Hydrazine containing conjugates of polypeptides and glycopolypeptides with polymers |
| US6037452A (en) * | 1992-04-10 | 2000-03-14 | Alpha Therapeutic Corporation | Poly(alkylene oxide)-Factor VIII or Factor IX conjugate |
| WO1994005332A2 (en) | 1992-09-01 | 1994-03-17 | Berlex Laboratories, Inc. | Glycolation of glycosylated macromolecules |
| US5733873A (en) | 1992-10-02 | 1998-03-31 | Pharmacia & Upjohn Ab | Composition comprising coagulation factor VIII formulation, process for its preparation and use of a surfactant as stabilizer |
| US5919766A (en) | 1992-10-02 | 1999-07-06 | Pharmacia & Upjohn Aktiebolag | Composition comprising coagulation factor VIII formulation, process for its preparation and use of a surfactant as stabilizer |
| EP0605963A2 (en) | 1992-12-09 | 1994-07-13 | Ortho Pharmaceutical Corporation | Peg hydrazone and peg oxime linkage forming reagents and protein derivatives thereof |
| US5298643A (en) * | 1992-12-22 | 1994-03-29 | Enzon, Inc. | Aryl imidate activated polyalkylene oxides |
| WO1994015625A1 (en) * | 1993-01-15 | 1994-07-21 | Enzon, Inc. | Factor viii - polymeric conjugates |
| WO1994028024A1 (en) | 1993-06-01 | 1994-12-08 | Enzon, Inc. | Carbohydrate-modified polymer conjugates with erythropoietic activity |
| WO1994029370A1 (en) | 1993-06-08 | 1994-12-22 | Enzon, Inc. | Factor ix - polymeric conjugates |
| US5621039A (en) | 1993-06-08 | 1997-04-15 | Hallahan; Terrence W. | Factor IX- polymeric conjugates |
| US5969040A (en) | 1993-06-08 | 1999-10-19 | Hallahan; Terrence W. | Factor IX -- polymeric conjugates |
| WO1995001804A1 (en) | 1993-07-05 | 1995-01-19 | Pharmacia Ab | A coagulation factor viii formulation |
| WO1996041813A2 (en) | 1994-11-09 | 1996-12-27 | Offord Robin E | Functionalized polymers for site-specific attachment |
| WO1996040731A1 (en) | 1995-06-07 | 1996-12-19 | Mount Sinai School Of Medicine Of The City University Of New York | Pegylated modified proteins |
| WO1997011957A1 (en) | 1995-09-29 | 1997-04-03 | Pharmacia & Upjohn Ab | Conjugates of a polypeptide and a biocompatible polymer |
| EP1258497A2 (en) | 1995-09-29 | 2002-11-20 | Biovitrum Ab | Conjugates of factor VIII and a biocompatible polymer |
| EP1260582A1 (en) | 1995-09-29 | 2002-11-27 | Biovitrum Ab | Conjugates of factor IX and a biocompatible polymer |
| US6048720A (en) | 1995-09-29 | 2000-04-11 | Pharmacia & Upjohn Ab | Conjugates of a polypeptide and a biocompatible polymer |
| US6743908B2 (en) | 1997-04-30 | 2004-06-01 | Enzon, Inc. | Single-chain antigen-binding proteins capable of glycosylation, production and uses thereof |
| US6872393B2 (en) | 1997-04-30 | 2005-03-29 | Enzon, Inc. | Polyalkylene oxide-modified single chain polypeptides |
| US6183738B1 (en) | 1997-05-12 | 2001-02-06 | Phoenix Pharamacologics, Inc. | Modified arginine deiminase |
| US20060286634A1 (en) | 1997-06-04 | 2006-12-21 | Oxford Biomedica (Uk) Limited | Vector |
| WO1999028455A1 (en) | 1997-12-03 | 1999-06-10 | Roche Diagnostics Gmbh | Method for preparing polypeptides with appropriate glycosilation |
| WO1999032134A1 (en) | 1997-12-19 | 1999-07-01 | Enzon, Inc. | Substantially pure histidine-linked protein polymer conjugates |
| WO2000012587A2 (en) | 1998-08-28 | 2000-03-09 | Gryphon Sciences | Polyamide chains of precise length, methods to manufacture them and their conjugates |
| WO2000023114A2 (en) | 1998-10-16 | 2000-04-27 | Biogen, Inc. | Polymer conjugates of interferon beta- 1a and their uses |
| US6692931B1 (en) | 1998-11-16 | 2004-02-17 | Werner Reutter | Recombinant glycoproteins, method for the production thereof, medicaments containing said glycoproteins and use thereof |
| WO2000048635A1 (en) | 1999-02-22 | 2000-08-24 | Baxter International Inc. | Novel albumin-free factor viii formulations |
| US7338788B2 (en) | 1999-08-27 | 2008-03-04 | Maxygen Aps | Interferon-β variants and conjugates |
| US7230081B1 (en) | 1999-11-12 | 2007-06-12 | Maxygen Holdings, Ltd. | Interferon gamma conjugates |
| US6806063B2 (en) | 2000-02-11 | 2004-10-19 | Maxygen Aps | Factor VII or VIIa-like molecules |
| US6586398B1 (en) | 2000-04-07 | 2003-07-01 | Amgen, Inc. | Chemically modified novel erythropoietin stimulating protein compositions and methods |
| WO2001082943A2 (en) | 2000-05-03 | 2001-11-08 | Novo Nordisk A/S | Subcutaneous administration of coagulation factor vii |
| WO2001083725A1 (en) | 2000-05-03 | 2001-11-08 | Novo Nordisk A/S | Human coagulation factor vii variants |
| US20020110535A1 (en) | 2000-06-08 | 2002-08-15 | Jones David S. | Multivalent platform molecules comprising high molecular weight polyethylene oxide |
| WO2002002764A2 (en) | 2000-06-30 | 2002-01-10 | Regents Of The University Of Minnesota | High molecular weight derivatives of vitamin k-dependent polypeptides |
| US7118737B2 (en) | 2000-09-08 | 2006-10-10 | Amylin Pharmaceuticals, Inc. | Polymer-modified synthetic proteins |
| WO2002022776A2 (en) | 2000-09-13 | 2002-03-21 | Novo Nordisk A/S | Human coagulation factor vii variants |
| WO2002029025A2 (en) | 2000-10-02 | 2002-04-11 | Novo Nordisk A/S | Factor vii glycoforms |
| WO2002077218A1 (en) | 2001-03-22 | 2002-10-03 | Novo Nordisk Health Care Ag | Coagulation factor vii derivatives |
| US6913915B2 (en) | 2001-08-02 | 2005-07-05 | Phoenix Pharmacologics, Inc. | PEG-modified uricase |
| US20060088906A1 (en) | 2001-10-10 | 2006-04-27 | Neose Technologies, Inc. | Erythropoietin: remodeling and glycoconjugation of erythropoietin |
| US20040063911A1 (en) | 2001-10-10 | 2004-04-01 | Neose Technologies, Inc. | Protein remodeling methods and proteins/peptides produced by the methods |
| US20050106658A1 (en) | 2001-10-10 | 2005-05-19 | Defrees Shawn | Remodeling and glycoconjugation of peptides |
| US20040137557A1 (en) | 2001-10-10 | 2004-07-15 | Neose Technologies, Inc. | Remodeling and glycoconjugation of peptides |
| WO2003031464A2 (en) | 2001-10-10 | 2003-04-17 | Neose Technologies, Inc. | Remodeling and glycoconjugation of peptides |
| US20030143596A1 (en) | 2001-11-07 | 2003-07-31 | Shearwater Corporation | Branched polymers and their conjugates |
| WO2003046150A2 (en) | 2001-11-28 | 2003-06-05 | Neose Technologies, Inc. | Glycoprotein remodeling using endoglycanases |
| WO2003045980A2 (en) | 2001-11-28 | 2003-06-05 | Neose Technologies, Inc. | Glycopeptide remodeling using amidases |
| WO2004000366A1 (en) | 2002-06-21 | 2003-12-31 | Novo Nordisk Health Care Ag | Pegylated factor vii glycoforms |
| WO2004014424A1 (en) | 2002-08-13 | 2004-02-19 | Enzon, Inc. | Releasable polymeric conjugates based on aliphatic biodegradable linkers |
| US20060019877A1 (en) | 2002-09-11 | 2006-01-26 | Conradt Harald S | Hasylated polypeptides |
| WO2004030617A2 (en) | 2002-09-30 | 2004-04-15 | Mountain View Pharmaceuticals, Inc. | Polymer conjugates with decreased antigenicity, methods of preparation and uses thereof |
| WO2004060965A2 (en) | 2002-12-31 | 2004-07-22 | Nektar Therapeutics Al, Corporation | Hydrolytically stable maleimide-terminated polymers |
| US20080146771A1 (en) | 2002-12-31 | 2008-06-19 | Antoni Kozlowski | Maleamic acid polymer derivatives and their bioconjugates |
| US20040235734A1 (en) | 2003-02-26 | 2004-11-25 | Bossard Mary J. | Polymer-factor VIII moiety conjugates |
| US7199223B2 (en) * | 2003-02-26 | 2007-04-03 | Nektar Therapeutics Al, Corporation | Polymer-factor VIII moiety conjugates |
| WO2004075923A2 (en) | 2003-02-26 | 2004-09-10 | Nektar Therapeutics Al, Corporation | Polymer-factor viii moiety conjugates |
| WO2004089280A2 (en) | 2003-04-08 | 2004-10-21 | Yeda Research And Development Co. Ltd. | Reversible pegylated drugs |
| WO2004108070A2 (en) | 2003-05-30 | 2004-12-16 | Enzon, Inc. | Releasable polymeric conjugates based on aliphatic biodegradable linkers |
| WO2005014035A2 (en) | 2003-08-08 | 2005-02-17 | Novo Nordisk Health Care Ag | Use of galactose oxidase for selective chemical conjugation of protractor molecules to proteins of therapeutic interest |
| WO2005014024A2 (en) | 2003-08-08 | 2005-02-17 | Fresenius Kabi Deutschland Gmbh | Conjugates of a polymer and a protein linked by an oxime linking group |
| WO2005055950A2 (en) | 2003-12-03 | 2005-06-23 | Neose Technologies, Inc. | Glycopegylated factor ix |
| WO2005070138A2 (en) | 2004-01-08 | 2005-08-04 | Neose Technologies, Inc. | O-linked glycosylation of peptides |
| WO2006020372A2 (en) | 2004-07-23 | 2006-02-23 | Neose Technologies, Inc. | Enzymatic modification of glycopeptides |
| WO2006013202A2 (en) | 2004-08-02 | 2006-02-09 | Novo Nordisk Health Care Ag | Conjugation of fvii |
| WO2006016168A2 (en) | 2004-08-12 | 2006-02-16 | Lipoxen Technologies Limited | Sialic acid derivatives |
| WO2006053299A2 (en) | 2004-11-12 | 2006-05-18 | Bayer Healthcare Llc | Site-directed modification of fviii |
| WO2006071801A2 (en) | 2004-12-27 | 2006-07-06 | Baxter International Inc | Polymer-von willebrand factor-conjugates |
| WO2006074279A1 (en) | 2005-01-06 | 2006-07-13 | Neose Technologies, Inc. | Glycoconjugation using saccharyl fragments |
| WO2006127896A2 (en) | 2005-05-25 | 2006-11-30 | Neose Technologies, Inc. | Glycopegylated factor ix |
| WO2006134173A2 (en) | 2005-06-17 | 2006-12-21 | Novo Nordisk Health Care Ag | Selective reduction and derivatization of engineered proteins comprising at least one non-native cysteine |
| WO2007022784A2 (en) | 2005-08-26 | 2007-03-01 | Maxygen Holdings Ltd. | Liquid factor vii composition |
| WO2007076062A2 (en) | 2005-12-21 | 2007-07-05 | Wyeth | Protein formulations with reduced viscosity and uses thereof |
| CA2647314A1 (en) | 2006-03-31 | 2007-11-08 | Baxter International Inc. | Pegylated factor viii |
| US20090076237A1 (en) * | 2006-03-31 | 2009-03-19 | Baxter Healthcare S.A. | Factor VIII Polymer Conjugates |
| US20070244301A1 (en) | 2006-03-31 | 2007-10-18 | Juergen Siekmann | Pegylated factor VIII |
| WO2007140282A1 (en) | 2006-05-24 | 2007-12-06 | Peg Biosciences | Peg linker compounds and biologically active conjugates thereof |
| US20080260755A1 (en) | 2006-06-14 | 2008-10-23 | Hubert Metzner | Proteolytically cleavable fusion proteins with high molar specific activity |
| WO2008035373A2 (en) | 2006-07-13 | 2008-03-27 | Serum Institute Of India Ltd | Highly pure polysialic acid and process for preperation thereof |
| WO2008012540A1 (en) | 2006-07-25 | 2008-01-31 | Lipoxen Technologies Limited | N-terminal polysialylation |
| WO2008025856A2 (en) | 2006-09-01 | 2008-03-06 | Novo Nordisk Health Care Ag | Modified glycoproteins |
| WO2008057683A2 (en) | 2006-10-03 | 2008-05-15 | Novo Nordisk A/S | Methods for the purification of polypeptide conjugates |
| WO2008074032A1 (en) | 2006-12-15 | 2008-06-19 | Baxter International Inc. | Factor viia- (poly) sialic acid conjugate having prolonged in vivo half-life |
| WO2008081024A1 (en) | 2007-01-03 | 2008-07-10 | Novo Nordisk Health Care Ag | Subcutaneous administration of coagulation factor viia-related popypeptdes |
| WO2008119815A1 (en) | 2007-04-02 | 2008-10-09 | Novo Nordisk A/S | Subcutaneous administration of coagulation factor ix |
| WO2009000522A1 (en) | 2007-06-26 | 2008-12-31 | Baxter International Inc. | Hydrolysable polymeric fmoc-linker |
| WO2009006620A1 (en) | 2007-07-03 | 2009-01-08 | Children's Hospital & Research Center At Oakland | Oligosialic acid derivatives, methods of manufacture, and immunological uses |
| WO2009047500A1 (en) | 2007-10-09 | 2009-04-16 | Polytherics Limited | Novel conjugated proteins and peptides |
| WO2009089396A2 (en) | 2008-01-08 | 2009-07-16 | Neose Technologies, Inc. | Glycoconjugation of polypeptides using oligosaccharyltransferases |
| WO2009108806A1 (en) | 2008-02-27 | 2009-09-03 | Novo Nordisk A/S | Conjugated factor viii molecules |
| WO2009130602A2 (en) | 2008-04-24 | 2009-10-29 | Celtic Pharma Peg Ltd. | Factor ix conjugates with extended half-lives |
| WO2009141433A1 (en) | 2008-05-23 | 2009-11-26 | Novo Nordisk Health Care Ag | Low viscosity compositions comprising a pegylated gla-domain containing protein |
| WO2009141418A1 (en) | 2008-05-23 | 2009-11-26 | Novo Nordisk A/S | Formulations of peg-functionalised serine proteases with high concentrations of an aromatic preservative |
| WO2009149303A1 (en) | 2008-06-04 | 2009-12-10 | Bayer Healthcare Llc | Fviii muteins for treatment of von willebrand disease |
| WO2010010324A1 (en) | 2008-07-21 | 2010-01-28 | Polytherics Limited | Novel reagents and method for conjugating biological molecules |
| WO2010062768A1 (en) | 2008-11-03 | 2010-06-03 | Bayer Healthcare Llc | Method for the treatment of hemophilia |
| WO2010083536A1 (en) | 2009-01-19 | 2010-07-22 | Bayer Healthcare Llc | Protein conjugate having an endopeptidase-cleavable bioprotective moiety |
| WO2010102886A1 (en) | 2009-02-19 | 2010-09-16 | Novo Nordisk A/S | Modification of factor viii |
| WO2010100430A1 (en) | 2009-03-04 | 2010-09-10 | Polytherics Limited | Conjugated proteins and peptides |
| WO2010120365A2 (en) | 2009-04-16 | 2010-10-21 | Wu Nian | Protein-carrier conjugates |
| WO2010131015A1 (en) | 2009-05-15 | 2010-11-18 | Almac Sciences (Scotland) Limited | Method of labelling interferons with peg |
| WO2011012850A2 (en) | 2009-07-27 | 2011-02-03 | Lipoxen Technologies Limited | Glycopolysialylation of non-blood coagulation proteins |
| WO2011017055A2 (en) | 2009-07-27 | 2011-02-10 | Baxter International Inc. | Blood coagulation protein conjugates |
| WO2011014890A1 (en) | 2009-07-31 | 2011-02-03 | Bayer Healthcare Llc | Modified factor ix polypeptides and uses thereof |
| WO2011018496A2 (en) | 2009-08-13 | 2011-02-17 | Leibniz-Institut für Polymerforschung Dresden e. V. | Method for modifying and functionalizing saccharides |
| WO2011037896A2 (en) | 2009-09-25 | 2011-03-31 | Vybion, Inc. | Polypeptide modification |
| WO2011064247A1 (en) | 2009-11-24 | 2011-06-03 | Novo Nordisk Health Care Ag | Method of purifying pegylated proteins |
| WO2011101267A1 (en) | 2010-02-16 | 2011-08-25 | Novo Nordisk A/S | Conjugated fviii variants |
| WO2011101242A1 (en) | 2010-02-16 | 2011-08-25 | Novo Nordisk A/S | Factor viii molecules with reduced vwf binding |
| WO2011135307A1 (en) | 2010-04-30 | 2011-11-03 | Leverton Licence Holdings Limited | Conjugated blood coagulation factor viii |
| WO2011135308A1 (en) | 2010-04-30 | 2011-11-03 | Leverton Licence Holdings Limited | Conjugated blood coagulation factor viia |
| WO2012068134A1 (en) | 2010-11-15 | 2012-05-24 | Biogen Idec Inc. | Enrichment and concentration of select product isoforms by overloaded bind and elute chromatography |
| WO2013009627A2 (en) | 2011-07-08 | 2013-01-17 | Biogen Idec Hemophilia Inc. | Factor viii chimeric and hybrid polypeptides, and methods of use thereof |
Non-Patent Citations (50)
| Title |
|---|
| Abuchowski et al., Cancer therapy with chemically modified enzymes. I. Antitumor properties of polyethylene glycol-asparaginase conjugates. Cancer Biochem. Biophys. 7: 175-86 (1984). |
| Baxter announces collaborations to develop longer acting forms of blood clotting factors. Baxter News (online), Sep. 29, 2005. |
| Bi et al., Target disruption of the mouse factor VIII gene produces a model of Haemophilia A. Nat. Genet. 10: 119-21 (1995). |
| Caliceti et al., Pharmacokinetics of pegylated interferons: What is misleading? Digest. Liver Dis. 36(Suppl. 3): S334-9 (2004). |
| Cordes et al., Nucleophilic catalysis of semicarbazone formation by anilines. J. Am. Chem. Soc., 84: 826-31 (1962). |
| Dirksen et al., Nucleophilic catalysis of hydrazone formation and transimination: Implications for dynamic covalent chemistry. J. Am. Chem. Soc., 128: 15602-3 (2006). |
| Dirksen et al., Nucleophilic catalysis of oxime ligation. Ange. Chem. Int. Ed., 45(45): 7581-4 (2006). |
| Dirksen et al., Rapid oxime and hydrazone ligations with aromatic aldehyres for biomolecular labeling. Bioconj. Chem., 19(12): 2543-8 (2008). |
| Enjolras et al. (2003) J. Thromb. Haemost. 2: 1143-54. * |
| Great Britain Search Report and Written Opinion, GB-1012482.4, dated Nov. 24, 2010. |
| Gregoriadis et al., Improving the therapeutic efficiency of peptides and proteins: A role for polysialic acids. Int. J. Pharma. 300(1-2): 125-30 (2005). |
| Harris et al., Effect of pegylation on pharmaceuticals. Nat. Rev. Drug Discovery. 2: 214-21 (2003). |
| International Preliminary Report on Patentability, PCT/GB2010/001422, dated Jan. 31, 2012. |
| International Preliminary Report on Patentability, PCT/US2009/052103, dated Feb. 1, 2011. |
| International Preliminary Report on Patentability, PCT/US2010/043242, dated Jan. 31, 2012. |
| International Preliminary Report on Patentability, PCT/US2011/045873, dated Feb. 5, 2013. |
| International Search Report and Written Opinion of the International Searching Authority, PCT/GB2010/001422, European Patent Office, dated Feb. 4, 2011. |
| International Search Report and Written Opinion of the International Searching Authority, PCT/US2007/007560, European Patent Office, dated Sep. 18, 2007. |
| International Search Report and Written Opinion of the International Searching Authority, PCT/US2009/052103, European Patent Office, dated Feb. 12, 2010. |
| International Search Report and Written Opinion, PCT/US2010/043242, dated Feb. 10, 2011. |
| Jain et al., Polysialylation: The natural way to improve the stability and pharmacokinestics of protein and peptide drugs http://www.lipoxen.co.uk/media/48760/dds%20and%20s%20pp3-9.pdf. |
| Jenkins et al. (2002) Blood 100(2): 501-8. * |
| Jiang et al., Chemistry for pegylation of protein and peptide molecules, Chin. J. Organ. Chem., 23(12): 1340-7 (2003).-English Abstract. |
| Jiang et al., Chemistry for pegylation of protein and peptide molecules, Chin. J. Organ. Chem., 23(12): 1340-7 (2003).—English Abstract. |
| Kohler, Aniline: A catalyst for sialic acid detection. ChemBioChem, 10: 2147-50 (2009). |
| Kozlowski et al., Development of pegylated interferons for the treatment of chronic Hepatitis C. BioDrugs. 15(7): 419-29 (2001). |
| Lees et al., Versatile and efficient synthesis of protein-polysaccharide conjugate vaccines using aminooxy reagents and oxime chemistry. Vaccine, 24(6): 716-29 (2006). |
| Mukherjee et al. (2008) Haemophilia 14(5): 1076-81. * |
| Nektar Advanced PEGylation Catalog 2005-2006, p. 30 (2005). |
| Nektar Advanced PEGylation Price List 2005-2006, p. 11 (2005). |
| NOF Corporation DDS Catalogue, p. 58 (2005). |
| Roberts et a., Chemistry for peptide and protein pegylation Adv. Drug Del. Rev. 54: 459-76 (2002). |
| Rosen et al., Assay of factor VIII: C with a chromogenic substrate. Scand J. Haematol. 33(Suppl. 40): 139-45 (1984). |
| Rostin et al., B-domain deleted recombinant coagulation factor VIII modified with monomethoxy polyethylene glycol. Bioconjugate Chem. 11: 387-96 (2000). |
| Saenko et al., Strategies towards a longer acting factor VIII. Haemophilia. 12: 42-51 (2006). |
| Sakuragawa et al., Studies on the stability of factor VIII modified by polyethylene glycol. Acta Med. Biol. 36:1-5 (1988). |
| Schmidt et al. (2003) Trends Cardiovasc. Med. 13(1): 39-45. * |
| Seffernick et al., Melamine deaminase and atrazine chlorohydrolase: 98% identical but functionally different. J. Bacteriology. 2405-10 (2001). |
| Severs et al., Characterization of PEGylated factor VIII molecules. Blood. 108: 11-12 (2006). ABSTRACT. |
| Study shows molecular size and structure of PEG interferon molecules, as used in pegintron(R), affect antiviral activity in vitro. Hispanic PR Wire, Oct. 28, 2003. |
| Thygesen et al., Nucleophilic catalysis of carbohydrate oxime formation by anilines. J. Org. Chem., 75: 1752-5 (2010). |
| Tsubery et al., Prolonging the action of protein and peptide drugs by a novel approach of reversible polyethylene glycol modification. J. Biol. Chem. 279(37): 38118-24 (2004). |
| Tsutsumi et al., Site-specific chemical modification with polyethylene glycol of recombinant immunotoxin anti-Tac(Fv)-PE38 (LMB-2) improves antitumor activity and reduces animal toxicity and immunogenicity. Proc. Natl. Acad. Sci. USA. 97: 8548-53 (2000). |
| Urrutigoity et al., Biocatalysis in organic solvents with a polymer-bound horseradish peroxidase. Biocatalysis. 2: 145-9 (1989). |
| Veronese et al., Bioconjugation in pharmaceutical chemistry. IL Farmaco. 54: 497-516 (1999). |
| Wells et al., Additivity of mutational effects in proteins. Biochemistry. 29(37): 8509-17 (1990). |
| Wilchek et al., Labeling glycoconjugates with hydrazide reagents. Methods Enzymol. 138: 429-42 (1987). |
| Yang et al. (2006) Protein Expr. Purif. 50(20): 196-202. * |
| Zalipsky et al., Hydrazide derivatives of poly(ethylene glycol) and their bioconjugates. Poly(ethylene glycol) Chemistry and Biological Applications. Chapter 21, pp. 318-341 (1997). |
| Zeng et al., High-efficiency labeling of sialylated glycoproteins on living cells. Nat. Meth. 6(3):207-9 (2009). |
Cited By (7)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US10350301B2 (en) * | 2009-07-27 | 2019-07-16 | Baxalta Incorporated | Blood coagulation protein conjugates |
| US11040109B2 (en) * | 2009-07-27 | 2021-06-22 | Takeda Pharmaceutical Company Limited | Blood coagulation protein conjugates |
| WO2017096383A1 (en) | 2015-12-03 | 2017-06-08 | Baxalta Incorporated | Factor viii with extended half-life and reduced ligand-binding properties |
| US20190240295A1 (en) * | 2015-12-03 | 2019-08-08 | Baxalta Incorporated | Factor viii with extended half-life and reduced ligand-binding properties |
| US11767526B2 (en) | 2019-01-23 | 2023-09-26 | Regeneron Pharmaceuticals, Inc. | Treatment of ophthalmic conditions with angiopoietin-like 7 (ANGPTL7) inhibitors |
| US11845989B2 (en) | 2019-01-23 | 2023-12-19 | Regeneron Pharmaceuticals, Inc. | Treatment of ophthalmic conditions with angiopoietin-like 7 (ANGPTL7) inhibitors |
| US11865134B2 (en) | 2021-02-26 | 2024-01-09 | Regeneron Pharmaceuticals, Inc. | Treatment of inflammation with glucocorticoids and angiopoietin-like 7 (ANGPTL7) inhibitors |
Also Published As
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US8637640B2 (en) | Blood coagulation protein conjugates | |
| US11040109B2 (en) | Blood coagulation protein conjugates | |
| US10251941B2 (en) | Factor VIIa-polysialic acid conjugates having prolonged in vivo half-life | |
| US20210106691A1 (en) | Therapeutic proteins with increased half-life and methods of preparing same | |
| EP3505186B1 (en) | Nucleophilic catalysts for oxime linkage | |
| US20190240295A1 (en) | Factor viii with extended half-life and reduced ligand-binding properties |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| AS | Assignment |
Owner name: BAXTER HEALTHCARE S.A., SWITZERLAND Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNORS:SIEKMANN, JUERGEN;HAIDER, STEFAN;ROTTENSTEINER, HANSPETER;AND OTHERS;SIGNING DATES FROM 20100928 TO 20101001;REEL/FRAME:025151/0082 Owner name: BAXTER INTERNATIONAL INC., ILLINOIS Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNORS:SIEKMANN, JUERGEN;HAIDER, STEFAN;ROTTENSTEINER, HANSPETER;AND OTHERS;SIGNING DATES FROM 20100928 TO 20101001;REEL/FRAME:025151/0082 |
|
| STCF | Information on status: patent grant |
Free format text: PATENTED CASE |
|
| CC | Certificate of correction | ||
| AS | Assignment |
Owner name: BAXALTA INCORPORATED, ILLINOIS Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNOR:BAXTER HEALTHCARE S.A.;REEL/FRAME:036360/0001 Effective date: 20150811 Owner name: BAXALTA GMBH, SWITZERLAND Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNOR:BAXTER HEALTHCARE S.A.;REEL/FRAME:036360/0001 Effective date: 20150811 Owner name: BAXALTA GMBH, SWITZERLAND Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNOR:BAXTER INTERNATIONAL INC.;REEL/FRAME:036372/0001 Effective date: 20150811 Owner name: BAXALTA INCORPORATED, ILLINOIS Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNOR:BAXTER INTERNATIONAL INC.;REEL/FRAME:036372/0001 Effective date: 20150811 |
|
| AS | Assignment |
Owner name: BAXALTA INCORPORATED, ILLINOIS Free format text: CORRECTIVE ASSIGNMENT TO CORRECT THE CONVEYING PARTIES NAME PREVIOUSLY RECORDED AT REEL: 036360 FRAME: 0001. ASSIGNOR(S) HEREBY CONFIRMS THE ASSIGNMENT;ASSIGNOR:BAXTER HEALTHCARE SA;REEL/FRAME:036621/0554 Effective date: 20150811 Owner name: BAXALTA GMBH, SWITZERLAND Free format text: CORRECTIVE ASSIGNMENT TO CORRECT THE CONVEYING PARTIES NAME PREVIOUSLY RECORDED AT REEL: 036360 FRAME: 0001. ASSIGNOR(S) HEREBY CONFIRMS THE ASSIGNMENT;ASSIGNOR:BAXTER HEALTHCARE SA;REEL/FRAME:036621/0554 Effective date: 20150811 |
|
| FPAY | Fee payment |
Year of fee payment: 4 |
|
| AS | Assignment |
Owner name: TAKEDA PHARMACEUTICAL COMPANY LIMITED, JAPAN Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNORS:BAXALTA GMBH;BAXALTA INCORPORATED;REEL/FRAME:055188/0953 Effective date: 20201205 |
|
| MAFP | Maintenance fee payment |
Free format text: PAYMENT OF MAINTENANCE FEE, 8TH YEAR, LARGE ENTITY (ORIGINAL EVENT CODE: M1552); ENTITY STATUS OF PATENT OWNER: LARGE ENTITY Year of fee payment: 8 |