RELATED APPLICATION
-
This application claims priority to U.S. provisional patent application Ser. No. 60/565,228 filed Apr. 23, 2004, which is expressly incorporated by reference in its entirety.
BACKGROUND OF THE INVENTION
-
(a) Field of the Invention
-
This invention relates to a method of purification for isolating albumin conjugates from a solution comprising both albumin conjugates and unconjugated albumin.
-
(b) Description of Prior Art
-
WO 95/10302 and WO 99/24074 describe the formation of conjugates of albumin wherein the molecule of interest has a reactive functionality coupled thereto that is adapted to covalently bond to albumin, thus forming a conjugate. These conjugates can be formed in vivo, but they can be formed in vitro as well. The formation of the conjugate in vitro involves the addition of a molecule coupled to a reactive functionality to a solution of albumin. The primary end products from this reaction are unconjugated albumin, the albumin conjugate and the unreacted molecule coupled to the reactive functionality.
-
It would be highly desirable to be provided with a method for purifying albumin conjugate from a solution comprising albumin conjugate and unconjugated albumin.
SUMMARY OF THE INVENTION
-
In accordance with the present invention there is provided a method for separating albumin conjugate from unconjugated albumin in a solution comprising albumin conjugate and unconjugated albumin, the method comprising:
-
a) loading the solution onto a hydrophobic solid support equilibrated in aqueous buffer having a high salt content;
b) applying to the support a gradient of decreasing salt content; and
c) collecting eluted albumin conjugate.
-
In a preferred embodiment of the present invention, the albumin conjugate consists of a molecule having a Michael acceptor covalently coupled thereto which bonds to albumin, and more preferably the bond is between the Michael acceptor and cysteine 34 of albumin.
-
In a more preferred embodiment of the present invention, the Michael acceptor is a maleimide group, and more preferably, the maleimide group is maleimide-propionic acid (MPA). The Michael acceptor is optionally coupled to the molecule via a linker. The linker is preferably selected in the group consisting of hydroxyethyl motifs such as (2-amino) ethoxy acetic acid (AEA), ethylenediamine (EDA), 2-[2-(2-amino)ethoxy)]ethoxy acetic acid (AEEA), amino ethoxy ethyl amino succinic acid (AEEAS); one or more alkyl chains (C1-C10) motifs such as glycine, 3-aminopropionic acid (APA), 8-aminooctanoic acid (AOA), octanoic acid (OA), 4-aminobenzoic acid (APhA). Preferred linkers are OA, ADE, AEA, AEEA and AEEAS. A combination of two linkers can also be used such as, for examples, AEEA-EDA, AEEA-AEEA, AEEAS-AEEAS, and AEA-AEEA.
-
In a preferred embodiment of the present invention, the albumin is selected from the group consisting of serum albumin, recombinant albumin and albumin from a genomic source.
-
In a preferred embodiment of the present invention, the albumin is selected from the group consisting of human albumin, rat albumin, mouse albumin, swine albumin, bovine albumin, dog albumin and rabbit albumin, more preferable human serum albumin.
-
In a preferred embodiment, albumin is modified with at least one selected from the group consisting of fatty acids, metal ions, small molecules having high affinity to albumin, and sugars, such as, but not limited to, glucose, lactose and mannose.
-
In a preferred embodiment of the present invention, the molecule is selected from the group consisting of a peptide, DNA, RNA, small organic molecule and a combination thereof. The peptide has preferentially a molecular weight of at least 57 daltons. The peptide is intended to include, but not being limited to, GLP-1, GLP-2, ANP, K5, dynorphin, GRF, insulin, natriuretic peptides, T-20, T-1249, C-34 and PYY. The small molecule is intended to include, but not being limited to, vinorelbine, gemcitabine and paclitaxel. In a more preferred embodiment of the present invention, when the molecule is a DNA, RNA or a small organic molecule, it is covalently attached to the albumin through an acid sensitive covalent bond or a peptide sequence susceptible to proteolytic cleavage, thereby allowing the separation of the molecule from albumin and the entry of the molecule into a cell.
-
In a preferred embodiment of the present invention, the hydrophobic solid support is a column containing a hydrophobic resin such as, but not limited to, octyl sepharose, phenyl sepharose and butyl sepharose and more preferably butyl sepharose.
-
In another embodiment of the present invention, the hydrophobic solid support comprising a hydrophobic ligand such as Cibacron Blue F3G-A, ether or isopropyl groups in association with a support such as polystyrene/divinyl benzene matrix.
-
Substances are separated on the basis of their varying strengths of hydrophobic interactions with hydrophobic ligands immobilized to an uncharged matrix. This technique is usually performed with moderately high concentrations of salts (≈1M) in the start buffer (salt promoted adsorption). Elution is achieved by a linear or stepwise decrease in salt concentration.
-
The type of ligand, the degree of substitution, the pH and the type and concentration of salt used during the adsorption stage have a profound effect on the overall performance (e.g. selectivity and capacity) of a HIC matrix (Hydrophobic Interaction Chromatography matrix).
-
The solvent is one of the most important parameters which influence capacity and selectivity in HIC (Hydrophobic Interaction Chromatography). In general, the adsorption process is more selective than the desorption process. It is therefore important to optimize the start buffer with respect to pH, type of solvent, type of salt and concentration of salt. The addition of various “salting-out” salts to the sample promotes ligand-protein interactions in HIC. As the concentration of salt is increased, the amount of bound protein increases up to the precipitation point for the protein. Each type of salt differs in its ability to promote hydrophobic interactions. The influence of different salts on hydrophobic interaction follows the well-known Hofmeisters series found below:
Hofmeisters Series
Salting-Out Effect
Anions:
-
PO4 3−>SO4 2−>CH3COO−>Cl−>Br−>NO3 −>ClO4 −>I−>SCN−
Chaotropic Effect
Cations:
NH4 +<Rb+<K+<Na+<Cs+<Li+<Mg2+<Ba2+
-
Increasing the salting-out effect strengthens the hydrophobic interactions, whereas increasing the chaotropic effect weakens them. Therefore, ammonium sulfate exhibits a stronger salting-out effect than sodium chloride. The most commonly used salts for HIC are ammonium sulfate ((NH4)2SO4), sodium sulfate ((Na)2SO4)), magnesium sulfate (MgSO4), sodium chloride (NaCl), potassium chloride (KCl), and ammonium acetate (CH3COONH4).
-
Protein binding to HIC adsorbents is promoted by moderate to high concentrations of “salting-out” salts, most of which also have a stabilizing influence on protein structure due to their preferential exclusion from native globular proteins, i.e. the interaction between the salt and the protein surface is thermodynamically unfavorable. The salt concentration should be high enough (e.g. 500-1000 mM) to promote ligand-protein interactions yet below that which causes precipitation of the protein in the sample. In the case of albumin, the salt concentration should be kept below 3M (moles per liter). The principle mechanism of salting-out consists of the salt-induced increase of the surface tension of water (Melander and Horváth, 1977). Thus, a compact structure becomes energetically more favorable because it corresponds to smaller protein-solution interfacial area.
-
Interestingly, we found that under the same conditions (i.e. buffer composed of SO4 2−, PO4 2− or CH3COO− with any counter ion), these salts exhibit their salting-out effect upon essentially all conjugated albumin described herein in a manner different to non-conjugated albumin (i.e. mercaptalbumin and albumin capped with cysteine), thus enabling a consistent chromatographic separation between conjugated albumin versus non-conjugated albumin. That is, we observe that lower concentrations of salt are required to promote interactions between ligand and conjugated albumin than between ligand and non-conjugated albumin. This chromatographic separation is essentially independent of (a) the sequence of albumin (e.g. human, mouse, rat, etc.) (b) the source of albumin (i.e. plasma derived or recombinant) (c) the molecular weight of the conjugated molecule, (d) the position of the Michael acceptor (or maleimide group) within the structure of the molecule, (e) the peptide sequence or chemical structure of the molecule, and (f) the three-dimensional structure of the conjugated molecule, e.g. linear versus loop structure.
-
In a preferred embodiment of the present invention, the salt of the aqueous buffer has a sufficient salting out effect. For providing a sufficient salting out effect, the salt is preferably, but not limited to, phosphate, sulfate and acetate. More preferably, the salt is phosphate or sulfate. The selection of the cation of the buffer is less critical and therefore, such cation can be selected, without limitation, from the group consisting of NH4 +, Rb+, K+, Na+, Cs+, Li+, Mg2+ and Ba2+.
-
The aqueous buffer is preferably ammonium phosphate, ammonium sulfate and magnesium phosphate, and more preferably ammonium sulfate.
-
In a preferred embodiment of the present invention, the buffer pH is between 3.0 and 9.0; more preferably between 6.0 and 8.0, and even more preferably, the pH is 7.0.
-
In a preferred embodiment of the present invention, the buffer and the hydrophobic solid support are at room temperature (about 25° C.) or at 4° C. or in between.
-
Table 1 shows an example of the effect of varying salts for purification of preformed HSA:first GLP-1 analogue conjugate from a solution of HSA using butyl-sepharose resin (structure of the first GLP-1 analogue is described in Example 1 below).
-
| TABLE 1 |
| |
| |
Starting salt |
Starting salt |
| |
concentration of |
concentration of |
| Salt type |
750 mM |
1,750 mM |
| |
| Ammonium phosphate |
Yes |
yes |
| Ammonium sulfate |
Yes |
yes |
| Ammonium chloride |
No |
no |
| Ammonium iodide |
No |
no |
| Ammonium thiocyanate |
No |
no |
| Magnesium sulfate |
No |
yes |
| Magnesium phosphate* |
— |
— |
| Barium sulfate* |
— |
— |
| |
| *means that the salt is not soluble at concentrations of 1750 mM or 750 mM in 20 mM sodium phosphate (pH 7), 5 mM caprylate |
| Yes means that successful resolution is achieved between the HSA:first GLP-1 analogue conjugate and the non-conjugated HSA |
| No means that no separation is achieved between the HSA:first GLP-1 analogue conjugate and the non-conjugated HSA |
-
The term “peptide” is intended to mean an amino acid sequence having a molecular weight of at least 57 daltons. The peptidic sequence can be circular (loop structure) such as ANP, may contain more than one amino acid chain such as insulin or may be linear such as K5, dynorphin A, C-34 and GLP-1.
-
All references herein are hereby incorporated by reference.
BRIEF DESCRIPTION OF THE DRAWINGS
-
FIG. 1 illustrates the purification of the conjugate HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 2 illustrates the purification of the conjugate HSA:first GRF analogue (SEQ ID NO:2) by a preferred embodiment of the method of the present invention;
-
FIG. 3 illustrates the purification of non-conjugated HSA by a preferred embodiment of the method of the present invention;
-
FIG. 4 illustrates the purification of the conjugate rHSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 5 illustrates the purification of HSA cortex by a preferred embodiment of the method of the present invention;
-
FIG. 6 illustrates the purification of the conjugate HSA:K5 analogue (SEQ ID NO:3) by a preferred embodiment of the method of the present invention;
-
FIG. 7 illustrates the purification of the conjugate HSA:first insulin derivative (SEQ ID NO:4) by a preferred embodiment of the method of the present invention;
-
FIG. 8 illustrates the purification of the conjugate HSA:second insulin derivative (SEQ ID NO:5) by a preferred embodiment of the method of the present invention;
-
FIG. 9 illustrates the purification of the conjugate HSA:first C34 analogue (SEQ ID NO:6) by a preferred embodiment of the method of the present invention;
-
FIG. 10 illustrates the purification of the conjugate HSA:second C34 analogue (SEQ ID NO:7) by a preferred embodiment of the method of the present invention;
-
FIG. 11 illustrates the purification of the conjugate HSA:third C34 analogue (SEQ ID NO:8) by a preferred embodiment of the method of the present invention;
-
FIG. 12 illustrates the purification of L-cysteine by a preferred embodiment of the method of the present invention;
-
FIG. 13 illustrates the purification of L-cysteine:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 14 illustrates the purification of the conjugate HSA:second GLP-1 analogue (SEQ ID NO:9) by a preferred embodiment of the method of the present invention;
-
FIG. 15 illustrates the purification of the conjugate HSA:third GLP-1 analogue (SEQ ID NO:10) by a preferred embodiment of the method of the present invention;
-
FIG. 16 illustrates the purification of the conjugate HSA:fourth GLP-1 analogue (SEQ ID NO:11) by a preferred embodiment of the method of the present invention;
-
FIG. 17 illustrates the purification of the conjugate HSA:fifth GLP-1 analogue (SEQ ID NO:12) by a preferred embodiment of the method of the present invention;
-
FIG. 18 illustrates the purification of the conjugate HSA:first Exendin-4 analogue (SEQ ID NO:13) by a preferred embodiment of the method of the present invention;
-
FIG. 19 illustrates the purification of the conjugate HSA:second Exendin-4 analogue (SEQ ID NO:14) by a preferred embodiment of the method of the present invention;
-
FIG. 20 illustrates the purification of HSA:MPA by a preferred embodiment of the method of the present invention;
-
FIG. 21 illustrates the purification of HSA by a preferred embodiment of the method of the present invention;
-
FIG. 22 illustrates the purification of the conjugate HSA:second C34 analogue (SEQ ID NO:3) by a preferred embodiment of the method of the present invention;
-
FIG. 23 illustrates the purification of the conjugate HSA:first Dynorphin A analogue (SEQ ID NO:15) by a preferred embodiment of the method of the present invention;
-
FIG. 24 illustrates the purification of the conjugate HSA:first ANP analogue (SEQ ID NO:16) by a preferred embodiment of the method of the present invention;
-
FIG. 25 illustrates the purification of the conjugate HSA:second Dynorphin A analogue (SEQ ID NO:17) by a preferred embodiment of the method of the present invention;
-
FIG. 26 illustrates the purification of the conjugate HSA:ACE inhibitor (SEQ ID NO:18) by a preferred embodiment of the method of the present invention;
-
FIG. 27 illustrates the purification of the conjugate HSA:sixth GLP-1 analogue (SEQ ID NO:19) by a preferred embodiment of the method of the present invention;
-
FIG. 28 illustrates the purification of the conjugate HSA:seventh GLP-1 analogue (SEQ ID NO:20) by a preferred embodiment of the method of the present invention;
-
FIG. 29 illustrates the purification of the conjugate HSA:eighth GLP-1 analogue (SEQ ID NO:21) by a preferred embodiment of the method of the present invention;
-
FIG. 30 illustrates the purification of the conjugate HSA:ninth GLP-1 analogue (SEQ ID NO:22) by a preferred embodiment of the method of the present invention;
-
FIG. 31 illustrates the purification of the conjugate HSA:tenth GLP-1 analogue (SEQ ID NO:23) by a preferred embodiment of the method of the present invention;
-
FIG. 32 illustrates the purification of the conjugate HSA:eleventh GLP-1 analogue (SEQ ID NO:24) by a preferred embodiment of the method of the present invention;
-
FIG. 33 illustrates the purification of the conjugate HSA:third Exendin-4 analogue (SEQ ID NO:25) by a preferred embodiment of the method of the present invention;
-
FIG. 34 illustrates the purification of the conjugate HSA:twelfth GLP-1 analogue (SEQ ID NO:26) by a preferred embodiment of the method of the present invention;
-
FIG. 35 illustrates the purification of the conjugate HSA:first insulin derivative (SEQ ID NO:4) by a preferred embodiment of the method of the present invention;
-
FIG. 36 illustrates the purification of the conjugate HSA:third insulin derivative (SEQ ID NO:27) by a preferred embodiment of the method of the present invention;
-
FIG. 37 illustrates the purification of the conjugate HSA:second insulin derivative (SEQ ID NO:5) by a preferred embodiment of the method of the present invention;
-
FIG. 38 illustrates the purification of the conjugate HSA:fourth insulin derivative (SEQ ID NO:28) by a preferred embodiment of the method of the present invention;
-
FIG. 39 illustrates the purification of the conjugate HSA:first GRF analogue (SEQ ID NO:2) by a preferred embodiment of the method of the present invention;
-
FIG. 40 illustrates the purification of the conjugate HSA:second GRF analogue (SEQ ID NO:29) by a preferred embodiment of the method of the present invention;
-
FIG. 41 illustrates the purification of the conjugate HSA:third GRF analogue (SEQ ID NO:30) by a preferred embodiment of the method of the present invention;
-
FIG. 42 illustrates the purification of the conjugate HSA:fourth GRF analogue (SEQ ID NO:31) by a preferred embodiment of the method of the present invention;
-
FIG. 43 illustrates the purification of the conjugate HSA:thirteenth GLP-1 analogue CJC 1365 (SEQ ID NO:32) by a preferred embodiment of the method of the present invention;
-
FIG. 44 illustrates the purification of the conjugate HSA lactose:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 45 illustrates the purification of the conjugate HSA:first T20 analogue (SEQ ID NO:33) by a preferred embodiment of the method of the present invention;
-
FIG. 46 illustrates the purification of the conjugate HSA:first T1249 analogue (SEQ ID NO:34) by a preferred embodiment of the method of the present invention;
-
FIG. 47 illustrates the purification of the compound HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 48 illustrates the purification of the compound HSA:first C34 analogue (SEQ ID NO:6) by a preferred embodiment of the method of the present invention;
-
FIG. 49 illustrates the purification of the compound HSA:second GRF analogue (SEQ ID NO:29) by a preferred embodiment of the method of the present invention;
-
FIG. 50 illustrates the purification of the conjugate HSA:vinorelbine analogue conjugate (SEQ ID NO:35) by a preferred embodiment of the method of the present invention;
-
FIG. 51 illustrates the purification of L-cysteine by a preferred embodiment of the method of the present invention;
-
FIG. 52 illustrates the purification of the conjugate L-Cysteine:vinorelbine analogue (SEQ ID NO:35) by a preferred embodiment of the method of the present invention;
-
FIG. 53 illustrates the purification of the conjugate RSA:third Exendin-4 analogue (SEQ ID NO:25) by a preferred embodiment of the method of the present invention;
-
FIG. 54 illustrates the purification of the conjugate HSA:fourth C34 analogue (SEQ ID NO:36) by a preferred embodiment of the method of the present invention;
-
FIG. 55 illustrates the purification of the conjugate HSA:fifth C34 analogue (SEQ ID NO:37) by a preferred embodiment of the method of the present invention;
-
FIG. 56 illustrates the purification of the conjugate HSA:sixth C34 analogue (SEQ ID NO:38) by a preferred embodiment of the method of the present invention;
-
FIG. 57 illustrates the purification of the conjugate HSA:seventh C34 analogue (SEQ ID NO:39) by a preferred embodiment of the method of the present invention;
-
FIG. 58 illustrates the purification of the conjugate HSA:eighth C34 analogue (SEQ ID NO:40) by a preferred embodiment of the method of the present invention;
-
FIG. 59 illustrates the purification of the conjugate HSA:first PYY analogue (SEQ ID NO:41) by a preferred embodiment of the method of the present invention;
-
FIG. 60 illustrates the purification of the conjugate HSA:second PYY analogue (SEQ ID NO:42) by a preferred embodiment of the method of the present invention;
-
FIG. 61 illustrates the purification of the conjugate HSA:fifth insulin derivative (SEQ ID NO:43) by a preferred embodiment of the method of the present invention;
-
FIG. 62 illustrates the purification of the conjugate HSA:sixth insulin derivative (SEQ ID NO:44) by a preferred embodiment of the method of the present invention;
-
FIG. 63 illustrates the purification of the conjugate HSA:seventh insulin derivative (SEQ ID NO:45) by a preferred embodiment of the method of the present invention;
-
FIG. 64 illustrates the purification of the conjugate HSA:third PYY analogue (SEQ ID NO:46) by a preferred embodiment of the method of the present invention;
-
FIG. 65 illustrates the purification of the conjugate HSA:fourth PYY analogue (SEQ ID NO:47) by a preferred embodiment of the method of the present invention;
-
FIG. 66 illustrates the purification of the conjugate HSA:fifth PYY analogue (SEQ ID NO:48) by a preferred embodiment of the method of the present invention;
-
FIG. 67 illustrates the purification of the conjugate HSA:sixth PYY analogue (SEQ ID NO:49) by a preferred embodiment of the method of the present invention;
-
FIG. 68 illustrates the purification of the conjugate HSA:second ANP analogue (SEQ ID NO:50) by a preferred embodiment of the method of the present invention;
-
FIGS. 69A-B illustrates the purification of the conjugate HSA:third ANP analogue CJC 1681 (SEQ ID NO:51) by a preferred embodiment of the method of the present invention;
-
FIG. 70 illustrates the purification of the conjugate HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 71 illustrates the purification of the conjugate HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 72 illustrates the purification of the conjugate HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 73 illustrates the purification of the conjugate HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 74 illustrates the purification of the conjugate HSA:first GLP-1 analogue (SEQ ID NO:1) by a preferred embodiment of the method of the present invention;
-
FIG. 75 illustrates the purification of the conjugate HSA:first GLP-2 analogue (SEQ ID NO:52) by a preferred embodiment of the method of the present invention; and
-
FIG. 76 illustrates the purification of the conjugate RSA:first GLP-2 analogue (SEQ ID NO:52) by a preferred embodiment of the method of the present invention.
DETAILED DESCRIPTION OF A PREFERRED EMBODIMENT OF THE INVENTION
-
In accordance with the present invention, there is provided a method for purifying albumin conjugates from a solution comprising albumin conjugates and unconjugated albumin.
Methods
Preparation of Control (Non-Conjugated) Human Serum Albumin (HSA) and Preformed Albumin Conjugates
-
Each compound with the Michael acceptor was solubilized in nanopure water (or in DMSO if the compound was difficult to solubilize) at a concentration of 10 mM, then diluted to 1 mM into a solution of HSA (25%, 250 mg/ml, Cortex-Biochem, San Leandro, Calif.). The samples were then incubated at 37° C. for 30 min. Prior to their purification, each conjugate solution was diluted to 5% 50 mg/ml HSA in 20 mM sodium phosphate buffer (pH 7) composed of 5 mM sodium octanoate. The initial concentration of salt used in the elution gradient can be added to the buffer for diluting the mixed solution. Preferably, the initial concentration of salt is from about 750 to about 1700 mM (NH4)2SO4.
Procedure for Purification According to a Preferred Embodiment
-
Using an
KTA purifier (Amersham Biosciences, Uppsala, Sweden), each conjugate was loaded at a flow rate of 2.5 ml/min onto a 50 ml column of
butyl sepharose 4 fast flow resin (Amershan Biosciences, Uppsala, Sweden) equilibrated in 20 mM sodium phosphate buffer (pH 7) composed of 5 mM sodium octanoate and 750 mM to 1.7 M (NH
4)
2SO
4. Under these conditions, HSA conjugates having a molecular weight addition of more than 2 kDa relative to non-conjugated HSA adsorbed onto the hydrophobic resin whereas essentially all non-conjugated HSA eluted within the void volume of the column. For molecular weight additions of less than 2 kDa, a higher initial salt content may be used followed by a stepwise gradient of decreasing salt. Each conjugate was further purified from any free unconjugated compound by applying a continuous or non-continuous decreasing gradient of salt (750 to 0 mM (NH
4)
2SO
4) over 4 column volumes. In a preferred embodiment, each purified conjugate was then desalted and concentrated by diafiltration, for instance by using Amicon® ultra centrifugal (30 kDa) filter devices (Millipore Corporation, Bedford, Mass.). Finally, for prolonged storage, each conjugate solution is preferably immersed into liquid nitrogen, and lyophilized using a Labconco freeze dry system (FreeZone®4.5), and stored at −20° C.
Examples of LC/EMS Analysis
-
Following purification, 1 μl of each conjugate sample is preferably injected onto LC/EMS system. The HSA:first GLP-1 analogue (SEQ ID NO:1) conjugate was confirmed by detection of a species of highest abundance with a total mass of 70 160 Da which corresponds to the mass of mercaptalbumin (66 448 Da) where cysteine 34 is in the free thiol form, plus the mass of only one molecule of the first GLP-1 analogue (3 719.9 Da). The structure of the first GLP-1 analogue (SEQ ID NO:1) is described in Example 1 below. This is illustrated in Table 2.
-
| |
TABLE 2 |
| |
|
| |
|
Molecular |
Absolute |
Relative |
| |
Component |
Weight |
Abundance |
Abundance |
| |
|
| |
| |
A |
70160.58 |
321970 |
100.00 |
| |
B |
65862.95 |
70008 |
21.74 |
| |
C |
64545.45 |
62888 |
19.53 |
| |
D |
70320.04 |
41167 |
12.79 |
| |
E |
61287.67 |
16842 |
5.23 |
| |
F |
60623.81 |
16522 |
5.13 |
| |
G |
58090.04 |
12473 |
3.87 |
| |
|
-
The HSA:first GRF analogue (SEQ ID NO:2) conjugate was confirmed by detection of a species of highest abundance with a total mass of 70 086 Da which corresponds to the mass of mercaptalbumin (66 448 Da) where cysteine 34 is in the free thiol form, plus the mass of only one molecule of the first GRF analogue (3648.2 Da). The structure of the first GRF analogue (SEQ ID NO:2) is described in Example 2 below. This is illustrated in Table 3.
-
| |
TABLE 3 |
| |
|
| |
|
Molecular |
Absolute |
Relative |
| |
Component |
Weight |
Abundance |
Abundance |
| |
|
| |
| |
A |
70086.06 |
279413 |
100.00 |
| |
B |
63214.84 |
53333 |
19.09 |
| |
C |
62148.17 |
38582 |
13.81 |
| |
D |
70247.98 |
34870 |
12.48 |
| |
E |
56795.96 |
10523 |
3.77 |
| |
F |
62695.49 |
9813 |
3.51 |
| |
|
-
The following examples illustrate several compounds having a maleimide group as Michael acceptor that have been conjugated to albumin and purified in accordance with the method of the present invention.
-
The following examples are for the purpose of illustrating the present invention and not of limiting its scope.
-
In the following examples, the gradient numbers refer to the following gradient details, where CV means a column volume of 50 ml.
-
Gradient #1: Linear 750-0 mM (NH4)2SO4, over 4 CV, flow rate of 2.5 ml/min.
-
Gradient #2: Step gradient 1.75M-1.2M (NH4)2SO4 over 0.5 CV, followed by 1.2M-875 mM (NH4)2SO4 over 5 CV, and finally 875 mM-0 mM (NH4)2SO4 over 0.5 CV flow rate of 2.5 ml/min.
-
Gradient #3: Linear 900-0 mM (NH4)2SO4 over 4 CV, flow rate of 2.5 ml/min.
-
Gradient #4: Step gradient 1.5M-1.1M (NH4)2SO4 over 0.5 CV, followed by 1.1M-375 mM (NH4)2SO4 over 6 CV, and finally 375 mM-0 mM (NH4)2SO4 over 0.5 CV, flow rate of 2.5 ml/min.
-
Gradient #5: Linear 750-0 mM (NH4)2SO4 over 2 CV, flow rate of 2.5 ml/min.
-
Gradient #6: Step gradient 1.75M-0M (NH4)2SO4 over 6 CV, flow rate of 2.5 ml/min.
-
Gradient #7: Linear 750-0 mM (NH4)2SO4 over 6 CV, flow rate of 2.5 ml/min.
Example 1
Purification of HSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| H(dA)EGTFTSDVSSYLEGQAAKEFIAWLVKGRK(AEEA-MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-1 analogue diluted into 9 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 1 the purified conjugate fraction elutes during the gradient of decreasing (NH4)2SO4 concentration as fraction B (F8-F9), whereas non-conjugated albumin elutes within the void volume of the column (fraction A). The conjugate fraction was concentrated with Ultrafree™ filter 30 kDa and analyzed using LC-EMS.
Example 2
Purification of HSA:First GRF Analogue (SEQ ID NO:2) Conjugate
-
The first GRF analogue is GRF (1-29) dAla2 Gln8 Ala15 Leu27 Lys30 (ε-MPA) CONH2 and has the following sequence:
-
| |
YaDAIFTQSYRKVLAQLSARKLLQDILSRK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GRF analogue diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 2 the purified conjugate fraction appears in fraction B (F6-F7) whereas non-conjugated albumin elutes within the void volume of the column (fraction A). The conjugate fraction was concentrated with Ultrafree™ filter 30 kDa and analyzed using LC-EMS.
Example 3
Purification of Non-Conjugated HSA 1 ml
-
The purification of 1 ml 25% 250 mg/ml non-conjugated HSA (Cortex-Biochem, San Leandro, Calif.) diluted into 9 ml of buffer (pH 7.0) made of 20 mM sodium phosphate buffer, 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #1 described above. Essentially all albumin molecules elute within the void volume and no protein species is observed at 280 nm during (NH4)2SO4 gradient. FIG. 3 illustrates the separation curve obtained.
Example 4
Purification of rHSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown in Example 1.
-
The purification of a conjugate made from reacting 5 ml 5% rHSA (recombinant HSA new century culture grade) with 200 μM first GLP-1 analogue diluted into 5 ml of a buffer made of 20 mM sodium phosphate buffer, 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 4 the purified conjugate fraction appears in fraction B (F7-F8-F9).
Example 5
Purification of HSA 10 ml
-
The purification of 10 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) diluted into 40 ml of a buffer made of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using the gradient #1 described above. Essentially all albumin molecules elute within a void volume and no protein species is observed at 280 nm during (NH4)2SO4 gradient. FIG. 5 illustrates the separation curve obtained.
Example 6
Purification of HSA:K5 Analogue (SEQ ID NO:3) Conjugate
-
The K5 analogue is Ac-K5 Lys8 (ε-MPA)-NH2 and has the following sequence:
-
-
The purification of a conjugate made from reacting 4 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM K5 analogue diluted into 16 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 6 the purified conjugate fraction appears in fraction A with albumin and in fraction B (F6-F7-F8).
Example 7
Purification of HSA:First Insulin Derivative (SEQ ID NO:4) Conjugate
-
The first insulin derivative is human insulin with MPA on position B1 and is represented in FIG. 1 below.
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first insulin derivative diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 7 the purified conjugate fraction appears in fraction B (F6-F7-F8).
Example 8
Purification of HSA:Second Insulin Derivative (SEQ ID NO:5) Conjugate
-
The second insulin derivative is human insulin with MPA on position A1 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second insulin derivative diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 8 the purified conjugate fraction appears in fraction B (F6-F7-F8).
Example 9
Purification of HSA:First C34 Analogue (SEQ ID NO:6) Conjugate
-
The first C34 analogue is MPA-AEEA-C34-CONH2 and has the following sequence:
-
-
The purification of a conjugate made from reacting 5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first C34 analogue diluted into 20 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 9 the purified conjugate fraction appears in fraction F2.
Example 10
Purification of HSA:Second C34 Analogue (SEQ ID NO:7) Conjugate
-
The second C34 analogue is C34 (1-34) Lys35 (ε-AEEA-MPA)-CONH2 and has the following structure:
-
-
The purification of a conjugate made from reacting 5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second C34 analogue diluted into 20 ml of 20 mM sodium phosphate buffer, 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 10 the purified conjugate fraction appears in fraction F2.
Example 11
Purification of HSA:Third C34 Analogue (SEQ ID NO:8) Conjugate
-
The third C34 analogue is C34 (1-34) Lys13 (ε-AEEA-MPA)-CONH2 and has the following structure:
-
-
The purification of a conjugate made from reacting 5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM third C34 analogue diluted into 20 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 11 the purified conjugate fraction appears in fraction F2.
Example 12
Purification of l-Cysteine
-
The purification of 121 mg of 1-cysteine in 2 ml of a buffer made of 20 mM sodium phosphate, 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #5 described above. FIG. 12 illustrates the separation curve obtained, where L-cysteine elutes within the void volume of the column (F3).
Example 13
Purification of L-cysteine:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
The purification of a conjugate made from reacting 121 mg L-cysteine with 36.36 mg first GLP-1 analogue diluted into 2 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #5 described above. FIG. 13 illustrates the separation curve obtained where the excess L-cysteine elutes in F3 (column void volume) and the L-Cysteine:first GLP-1 analogue conjugate elutes in 0 mM (NH4)2SO4.
Example 14
Purification of HSA:Second GLP-1 Analogue (SEQ ID NO:9) Conjugate
-
The second GLP-1 analogue is GLP-1 (7-36) Lys37 (ε-MPA)-NH2 and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQAAKEFIAWLVKGRK(ε-MPA) |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second GLP-1 analogue diluted into 10 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #5 described above. In FIG. 14 the purified conjugate fraction appears in fraction F2.
Example 15
Purification of HSA:Third GLP-1 Analogue (SEQ ID NO:10) Conjugate
-
The third GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-MPA)-NH2 and has the following sequence:
-
| |
H(dA)EGTFTSDVSSYLEGQAAKEFIAWLVKGRK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM third GLP-1 analogue diluted into 10 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #5 described above. In FIG. 15 the purified conjugate fraction appears in fraction F2.
Example 16
Purification of HSA:Fourth GLP-1 Analogue (SEQ ID NO:11) Conjugate
-
The fourth GLP-1 analogue is GLP-1 (7-36) Lys26 (ε-AEEA-AEEA-MPA) and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQMK(ε-AEEA-AEEA-MPA) EFIAWLVKGR |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM fourth GLP-1 analogue diluted into 10 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 16 the purified conjugate fraction appears in fraction F2.
Example 17
Purification of HSA:Fifth GLP-1 Analogue (SEQ ID NO:12) Conjugate
-
The fifth GLP-1 analogue is GLP-1 (7-36) Lys34 (ε-AEEA-AEEA-MPA) and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQAAKEFIAWLVK(ε-AEEA-AEEA-MPA)GR |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM fifth GLP-1 analogue diluted into 10 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 17 the purified conjugate fraction appears in fraction F2.
Example 18
Purification of HSA:First Exendin-4 Analogue (SEQ ID NO:13) Conjugate
-
The first exendin-4 analogue is Exendin-4-(1-39) Lys40 (ε-MPA)-NH2 and has the following sequence:
-
| HGEGTFTSDLSKQMEEEAVRLFIEWLKNGGPSSGAPPPSK(ε-MPA)- |
|
| |
| CONH2 |
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first Exendin-4 analogue diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 18 the purified conjugate fraction appears in fraction F2.
Example 19
Purification of HSA:Second Exendin-4 Analogue (SEQ ID NO:14) Conjugate
-
The second Exendin-4 analogue is Exendin-4 (9-39) Lys40 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| DLSKQMEEEAVRLFIEWLKNGGPSSGAPPPSK(AEEA-MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 3.5 ml 25% HSA cortex with 1 mM second Exendin-4 analogue diluted into 21.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 19 the purified conjugate fraction appears in fraction F2.
Example 20
Purification of HSA:MPA
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 2 mM MPA diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #2 described above. In FIG. 20 the fraction of mercaptalbumin is in fraction A (F5) and capped albumin is in fraction B (F7-F8). The conjugate fraction was concentrated with Amicon™ filter 30 kDa.
Example 21
Purification of HSA
-
The purification of 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using the gradient #2 described above. When using gradient #2, unlike gradients #1 and #5, both conjugated albumin and non-conjugated albumin adsorbs onto the hydrophobic resin during sample loading. FIG. 21 illustrates the separation curve obtained where F4 and F5 are enriched in mercaptalbumin and F6, F7 and F8 are enriched in capped albumin.
Example 22
Purification of HSA:Second C34 Analogue (SEQ ID NO:3) Conjugate
-
The second C34 analogue is C34 (1-34) Lys35 (ε-AEEA-MPA)-CONH2 and his structure is shown in Example 10.
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second C34 analogue diluted into 9 ml of a buffer made of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #2 described above. In FIG. 22 mercaptalbumin appears in fraction A (F5) and capped albumin and the purified conjugated is in fraction B (F7-F8).
Example 23
Purification of HSA:First Dynorphin A Analogue (SEQ ID NO:15) Conjugate
-
The first Dynorphin A analogue is Dyn A (1-13) (MPA)-NH2 and has the following sequence:
-
| |
YGGFLRRIRPKLK(MPA)-CONH2. |
|
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first Dynorphin A analogue diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #2 described above. In FIG. 23 the purified conjugate fraction appears in fraction A (F11-F12)
Example 24
Purification of HSA:First ANP Analogue (SEQ ID NO:16) Conjugate
-
The first ANP analogue is MPA-AEEA-ANP (99-126)-CONH2 and has the following structure:
-
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first ANP analogue diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #2 described above. In FIG. 24 the purified conjugate fraction appears in fraction A (F14).
Example 25
Purification of HSA:Second Dynorphin A Analogue (SEQ ID NO:17) Conjugate
-
The second Dynorphin A analogue is Dyn A (7-13) Lys13 (ε-MPA)-CONH2 and has the following sequence:
-
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second Dynorphin A analogue diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #2 described above. In FIG. 25 the purified conjugate fraction appears in fraction A (F9).
Example 26
Purification of HSA:ACE Inhibitor (SEQ ID NO:18) Conjugate
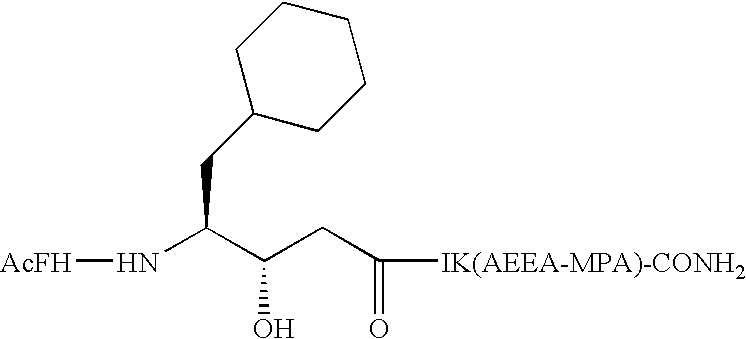
-
The ACE inhibitor used in this example is acetyl-Phe-His-cyclohexylstatyl-Ile-Lys (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM ACE inhibitor diluted into 9 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #2 described above. In FIG. 26 the purified conjugate fraction appears in fraction A (F14).
Example 27
Purification of HSA:Sixth GLP-1 Analogue (SEQ ID NO:19) Conjugate
-
The sixth GLP-1 analogue is GLP-1 (7-36) Lys23 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGK(AEEA-MPA)AAKEFIAWLVKGR-CONH2 |
|
-
The purification of a conjugate made from reacting 3 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM sixth GLP-1 analogue diluted into 22 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 27 the purified conjugate fraction appears in fraction F2.
Example 28
Purification of HSA:Seventh GLP-1 Analogue (SEQ ID NO:20) Conjugate
-
The seventh GLP-1 analogue is GLP-1 (7-36) Lys18 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
HAEGTFTSDVSK(AEEA-MPA)YLEGQAAKEFIAWLVKGR-CONH2 |
|
-
The purification of a conjugate made from reacting 3 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM seventh GLP-1 analogue diluted into 22 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 28 the purified conjugate fraction appears in fraction F2.
Example 29
Purification of HSA:Eighth GLP-1 Analogue (SEQ ID NO:21) Conjugate
-
The eighth GLP-1 analogue is GLP-1 (7-36) Lys26 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQAAK(AEEA-MPA)EFIAWLVKGR-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM eighth GLP-1 analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 29 the purified conjugate fraction appears in fraction F2.
Example 30
Purification of HSA:Ninth GLP-1 Analogue (SEQ ID NO:22) Conjugate
-
The ninth GLP-1 analogue is GLP-1 (7-37) Lys27 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQAAKK(AEEA-MPA)FIAWLVKGR-CONH2 |
|
-
The purification of a conjugate made from reacting 3 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM ninth GLP-1 analogue diluted into 22 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 30 the purified conjugate fraction appears in fraction F2.
Example 31
Purification of HSA:Tenth GLP-1 Analogue (SEQ ID NO:23) Conjugate
-
The tenth GLP-1 analogue is GLP-1 (7-36) Lys37 (ε-AEEA-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQAAKEFIAWLVKGRK-AEEA-AEEA-MPA- |
|
| |
|
| |
CONH2 |
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM tenth GLP-1 analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 31 the purified conjugate fraction appears in fraction F2.
Example 32
Purification of HSA:Eleventh GLP-1 Analogue (SEQ ID NO:24) Conjugate
-
The eleventh GLP-1 analogue is GLP-1 (7-36) Lys37 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
HAEGTFTSDVSSYLEGQAAKEFIAWLVKGRK(AEEA-MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM eleventh GLP-1 analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 32 the purified conjugate fraction appears in fraction F2.
Example 33
Purification of HSA:Third Exendin-4 Analogue (SEQ ID NO:25) Conjugate
-
The third Exendin-4 analogue is Exendin-4-(1-39) Lys40 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| HGEGTFTSDLSKQMEEEAVRLFIEWLKNGGPSSGAPPPSK(ε-AEEA- |
|
| |
| MPA)-CONH2 |
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM third Exendin-4 analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 33 the purified conjugate fraction appears in fraction F2.
Example 34
Purification of HSA:Twelfth GLP-1 Analogue (SEQ ID NO:26) Conjugate
-
The twelfth GLP-1 analogue is GLP-1 (7-36) Lys34 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| HAEGTFTSDVSSYLEGQAAKEFIAWLVK(ε-AEEA-MPA)GR-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM twelfth GLP-1 analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 34 the purified conjugate fraction appears in fraction F2.
Example 35
Purification of HSA:First Insulin Derivative (SEQ ID NO:4) Conjugate
-
The first insulin derivative is human insulin with MPA on position B1 and his structure is detailed in Example 7.
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first insulin derivative diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 35 the purified conjugate fraction appears in fraction F2.
Example 36
Purification of HSA:Third Insulin Derivative (SEQ ID NO:27) Conjugate
-
The third insulin derivative is human insulin with OA-MPA on position B1 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 4 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM third insulin derivative diluted into 21 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 36 the purified conjugate fraction appears in fraction F2.
Example 37
Purification of HSA:Second Insulin Derivative (SEQ ID NO:5) Conjugate
-
The second insulin derivative is human insulin with MPA on position A1 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 3 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second insulin derivative diluted into 22 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 37 the purified conjugate fraction appears in fraction F2.
Example 38
Purification of HSA:Fourth Insulin Derivative (SEQ ID NO:28) Conjugate
-
The fourth insulin derivative is human insulin with MPA on position B29 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 3 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM fourth insulin derivative diluted into 22 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 38 the purified conjugate fraction appears in fraction F2.
Example 39
Purification of HSA:First GRF Analogue (SEQ ID NO:2) Conjugate
-
The first GRF analogue is GRF (1-29) dAla2 Gln8 Ala15 Leu27 Lys30 (ε-MPA) CONH2 and his sequence is shown in Example 2.
-
The purification of a conjugate made from reacting 3.7 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GRF analogue diluted into 22 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 39 the purified conjugate fraction appears in fraction F2.
Example 40
Purification of HSA:Second GRF Analogue (SEQ ID NO:29) Conjugate
-
The second GRF analogue is GRF(1-29) Lys30 (ε-MPA)-CONH2 and has the following sequence:
-
| |
YADAIFTNSYRKVLGQLSARKLLQDIMSRK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM second GRF analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 900 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIG. 40 the purified conjugate fraction appears in fraction F2.
Example 41
Purification of HSA:Third GRF Analogue (SEQ ID NO:30) Conjugate
-
The third GRF analogue is GRF (1-29) dAla2 Gln8 dArg11 Ala15 Leu27 Lys30 (ε-MPA)-CONH2 and has the following sequence:
-
| |
YaDAIFTQSYrKVLAQLSARKLLQDILSRK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM third GRF analogue diluted into 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIG. 41 the purified conjugate fraction appears in fraction F2.
Example 42
Purification of HSA:Fourth GRF Analogue (SEQ ID NO:31) Conjugate
-
The fourth GRF analogue is GRF (1-29) dAla2 Lys30 (ε-MPA)-CONH2 and has the following sequence:
-
| |
YaDAIFTNSYRKVLGQLSARKLLQDIMSRK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 2.5 ml 25% HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM fourth GRF analogue diluted in 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 900 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIG. 42 the purified conjugate fraction appears in fraction F2.
Example 43
Purification of HSA:Thirteenth GLP-1 Analogue CJC 1365 (SEQ ID NO:32) Conjugate
-
The thirteenth GLP-1 analogue is GLP-1 (9-36) Lys37 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| |
EGTFTSDVSSYLEGQAAKEFIAWLVKGRK(ε-AEEA-MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 3.5 ml 25% HSA (Cortex-Biochem, San Leandro, Calif.) and 1 mM thirteenth GLP-1 analogue diluted in 21.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 43 the purified conjugate fraction appears in fraction F2.
Example 44
Purification of HSA Lactose:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
The purification of a conjugate made from reacting 4 ml 25% lactosaminated albumin (HSA pre-incubated with excess lactose at 37° C., pH 7.0) with 200 μM first GLP-1 analogue in 4 ml of a buffer made of 20 mM sodium phosphate, 5 mM sodium caprylate and 750 mM (NH4)2SO4, (pH 7.0) was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 44 the purified lactosaminated conjugate fraction appears in fraction F2.
Example 45
Purification of HSA:First T20 Analogue (SEQ ID NO:33) Conjugate
-
The first T20 analogue is Ac-T20 (1-36) Lys37 (ε-AEEA-MPA)-CONH2 and ahs the following sequence:
-
| |
Ac-YTSLIHSLIEESQNQQEKNEQELLELDKWASLWNWFK(AEEA- |
|
| |
|
| |
MPA)-CONH2 |
-
The purification of a conjugate made from reacting 2.5 ml 25% HSA with 1 mM first T20 analogue in 10 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 45 the purified conjugate fraction appears in fraction F2.
Example 46
Purification of HSA:First T1249 Analogue (SEQ ID NO:34) Conjugate
-
The first T1249 analogue is Ac-T1249 (1-39) Lys40 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| Ac-WQEWEQKITALLEQAQIQQEKNEYELQKLDKWASLWEWFK(AEEA- |
|
| |
| MPA)-CONH2 |
-
The purification of a conjugate made from reacting 2 ml 25% HSA and 1 mM first T1249 analogue in 10.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 46 the purified conjugate fraction appears in fraction F4.
Example 47
Purification of a HSA:First GLP-1 Analogue (SEQ ID NO:1)
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown in Example 1.
-
The purification of 114.45 mg of the preformed conjugate of the first GLP-1 analogue in 12.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #5 described above. FIG. 47 illustrates the separation curve obtained with the conjugate found in fraction F2.
Example 48
Purification of a HSA:First C34 Analogue (SEQ ID NO:6)
-
The first C34 analogue is MPA-AEEA-C34-CONH2 and his sequence is shown above in Example 9.
-
The purification of 114.45 mg of the preformed conjugate of the first C34 analogue in 12.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #5 described above. FIG. 48 illustrates the separation curve obtained with the conjugate found in fraction F2.
Example 49
Purification of a HSA:Second GRF Analogue (SEQ ID NO:29)
-
The second GRF analogue is GRF(1-29) Lys30 (ε-MPA)-CONH2 and his sequence is shown above in Example 40.
-
The purification of 125.53 mg of the preformed conjugate of the second GRF analogue in 12.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, pH 7.0 was performed on a column of Butyl sepharose using gradient #5 described above. FIG. 49 illustrates the separation curve obtained with the conjugate found in fraction F2.
Example 50
Purification of HSA:Vinorelbine Analogue Conjugate (SEQ ID NO:35)
-
The vinorelbine analogue is a molecule of vinorelbine with AEEA-MPA coupled thereto as illustrated in the following structure:
-
-
The purification of a conjugate made from 2.5 ml 25% HSA and 1 mM vinorelbine analogue in 22.5 ml of a buffer made of 20 mM sodium phosphate buffer, 5 mM sodium caprylate and 750 mM (NH4)2SO4, pH 7.0 was performed on a column of Butyl sepharose using gradient #4 described above. In FIG. 50 the purified conjugate fraction appears in fraction F2. The conjugate fraction was concentrated with Amicon™ filter 30 kDa.
Example 51
Purification of L-Cysteine
-
The purification of 2.5 ml 40 mM L-cysteine in 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 1500 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #4 described above. FIG. 51 illustrates the separation curve obtained with L-cysteine eluting within the void volume of the column (fraction F3).
Example 52
Purification of L-Cysteine:Vinorelbine Analogue (SEQ ID NO:35) Conjugate
-
The vinorelbine analogue is a molecule of vinorelbine with AEEA-MPA coupled thereto as illustrated in the structure shown in Example 50.
-
The purification of a conjugate made from reacting 2.5 ml 40 mM L-cysteine with 1 mM vinorelbine analogue in 22.5 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #4 described above. FIG. 52 illustrates the separation curve obtained with the L-cysteine conjugate eluting within fractions F8, F9 and F10.
Example 53
Purification of RSA:Third Exendin-4 Analogue (SEQ ID NO:25) Conjugate
-
The third Exendin-4 analogue is Exendin-4-(1-39) Lys40 (ε-AEEA-MPA)-CONH2 and his sequence shown in Example 33.
-
The purification of a conjugate made from reacting 11 ml 5% RSA (rat serum albumin) with 200 μM third Exendin-4 analogue in 11 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 53 the purified conjugate fraction appears in fraction F2.
Example 54
Purification of HSA:Fourth C34 Analogue (SEQ ID NO:36) Conjugate
-
The fourth C34 analogue is C34 (1-34) Lys13 (ε-MPA)-CONH2 and has the following sequence:
-
| |
WMEWDREINNYTK(MPA)LIHSLIEESQNQQEKNEQELL-CONH2 |
|
-
The purification of a conjugate made from reacting 2 ml 25% HSA with 1 mM fourth C34 analogue in 13 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 54 the purified conjugate fraction appears in fraction F2.
Example 55
Purification of HSA:Fifth C34 Analogue (SEQ ID NO:37) Conjugate
-
The fifth C34 analogue is C34 (1-34) Lys35 (ε-MPA)-CONH2 and has the following sequence:
-
| |
WMEWDREINNYTSLIHSLIEESQNQQEKNEQELLK(MPA)-CONH2 |
|
-
The purification of a conjugate made from 2 ml 25% HSA and 1 mM fifth C34 analogue in 13 ml of a buffer made of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 55 the purified conjugate fraction appears in fraction F2.
Example 56
Purification of HSA:Sixth C34 Analogue (SEQ ID NO:38) Conjugate
-
The sixth C34 analogue MPA-C34 (1-34)-CONH2 and has the following sequence:
-
| |
MPA-WMEWDREINNYTSLIHSLIEESQNQQEKNEQELL-CONH2 |
|
-
The purification of a conjugate made from reacting 2 ml 25% HSA and 1 mM sixth C34 analogue in 13 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 56 the purified conjugate fraction appears in fraction F2.
Example 57
Purification of HSA:Seventh C34 Analogue (SEQ ID NO:39) Conjugate
-
The seventh C34 analogue is Ac-C34 (1-34) Glu2 Lys6 Lys7 Glu9 Glu10 Lys13 Lys14 Glu16 Glu17 Lys20 Lys21 Glu23 Glu24 Lys27 Glu31 Lys34 Lys35 Lys36 (ε-AEEA-MPA)-CONH2 and has the following sequence:
-
| Ac-WEEWOKKIEEYTKKIEELIKKSEEQQKKNEEELKKK(AEEA-MPA)- |
|
| |
| CONH2 |
-
The purification of a conjugate made from reacting 2 ml 25% HSA with 1 mM seventh C34 analogue in 13 ml 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 57 the purified conjugate fraction appears in fraction F2.
Example 58
Purification of HSA:Eighth C34 Analogue (SEQ ID NO:40) Conjugate
-
The eighth C34 analogue is MPA-AEEA-C34 (1-34) Glu2 Lys6 Lys7 Glu9 Glu10 Lys13 Lys14 Glu16 Glu17 Lys20 Lys21 Glu23 Glu24 Lys27 Glu31 Lys34 Lys35-CONH2 and has the following sequence:
-
| MPA-AEEA-WEEWDKKIEEYTKKIEELIKKSEEQQKKNEEELKK-CONH2 |
|
-
The purification of a conjugate made from reacting 2 ml 25% HSA with 1 mM eighth C34 analogue in 13 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 58 the purified conjugate fraction appears in fraction F2.
Example 59
Purification of HSA:First PYY Analogue (SEQ ID NO:41) Conjugate
-
The first PYY analogue is PYY (3-36) Lys4 (ε-OA-MPA)-CONH2 and has the following structure:
-
-
The purification of a conjugate made from reacting 1.5 ml 25% HSA with 1 mM first PYY analogue in 6 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 59 the purified conjugate fraction appears in fraction F2.
Example 60
Purification of HSA:Second PYY Analogue (SEQ ID NO:42) Conjugate
-
The second PYY analogue is MPA-OA-PYY (3-36)-CONH2 and has the following sequence:
-
-
The purification of a conjugate made from reacting 1.5 ml 25% HSA with 1 mM second PYY analogue in 6 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 60 the purified conjugate fraction appears in fraction F2.
Example 61
Purification of HSA:Fifth Insulin Derivative (SEQ ID NO:43) Conjugate
-
The fifth insulin derivative is human insulin with AEEAS-AEEAS-MPA on position B29 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 2 ml 25% HSA with 1 mM fifth insulin derivative in 15 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 61 the purified conjugate fraction appears in fraction F2.
Example 62
Purification of HSA:Sixth Insulin Derivative (SEQ ID NO:44) Conjugate
-
The sixth insulin derivative is human insulin with AEEAS-AEEAS-MPA on position B1 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 2.5 ml 25% HSA with 1 mM sixth insulin derivative in 15 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 62 the purified conjugate fraction appears in fraction F2.
Example 63
Purification of HSA:Seventh Insulin Derivative (SEQ ID NO:45) Conjugate
-
The seventh insulin derivative is human insulin with OA-MPA on position B29 and is represented in FIG. 1 shown above in Example 7.
-
The purification of a conjugate made from reacting 2 ml 25% HSA with 1 mM seventh insulin derivative in 15 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 63 the purified conjugate fraction appears in fraction F2.
Example 64
Purification of HSA:Third PYY Analogue (SEQ ID NO:46) Conjugate
-
The third PYY analogue is MPA-PYY (3-36)-CONH2 and has the following sequence:
-
| |
MPA-NH-IKPEAPGEDASPEELNRYYASLRHYLNLVTRQRY-CONH2 |
|
-
The purification of a conjugate made from reacting 3 ml 25% HSA with 1 mM third PYY analogue in 18 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 64 the purified conjugate fraction appears in fraction F2.
Example 65
Purification of HSA:Fourth PYY Analogue (SEQ ID NO:47) Conjugate
-
The fourth PYY analogue is PYY (3-36) Lys37 (ε-MPA)-CONH2 and has the following sequence:
-
| |
IKPEAPGEDASPEELNRYYASLRHYLNLVTRQRYK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 3 ml 25% HSA with 1 mM fourth PYY analogue in 18 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #1 described above. In FIG. 65 the purified conjugate fraction appears in fraction F2.
Example 66
Purification of HSA:Fifth PYY Analogue (SEQ ID NO:48) Conjugate
-
The fifth PYY analogue is MPA-PYY (22-36)-CONH2 and has the following sequence: (MPA)-ASLRHYLNLVTRQRY-CONH2.
-
The purification of a conjugate made from reacting 6 ml 25% HSA with 1 mM fifth PYY analogue in 36 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 900 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIG. 66 the purified conjugate fraction appears in fraction F2.
Example 67
Purification of HSA:Sixth PYY Analogue (SEQ ID NO:49) Conjugate
-
The sixth PYY analogue is Acetyl-PYY (22-36) Lys37 (ε-MPA)-CONH2 and has the following sequence: Ac-ASLRHYLNLVTRQRYK(MPA)-CONH2.
-
The purification of a conjugate made from reacting 6 ml 25% HSA with 1 mM sixth PYY analogue in 36 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 900 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIG. 67 the purified conjugate fraction appears in fraction F2.
Example 68
Purification of HSA:Second ANP Analogue (SEQ ID NO:50) Conjugate
-
The second ANP analogue is MPA-ANP (99-126)-CONH2 and has the following structure:
-
-
The purification of a conjugate made from reacting 1 ml 25% HSA with 1 mM second ANP analogue in 14 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 750 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIG. 68 the purified conjugate fraction appears in fraction F2.
Example 69
Purification of HSA:Third ANP Analogue (SEQ ID NO:51) Conjugate
-
The third ANP analogue is ANP (99-126) having reacted with MAL-dPEG4™ (Quanta Biodesign, Powell, Ohio, USA) coupled to Ser99. The resulting ANP analogue is MPA-EEEEP-ANP (99-126) where EEEEP is ethoxy ethoxy ethoxy ethoxy propionic acid; and its sequence is the following:
-
-
The purification of a conjugate made from reacting 1 ml 25% HSA with 1 mM CJC 1681 in 14 ml of 20 mM sodium phosphate buffer (pH 7.0), 5 mM sodium caprylate and 900 mM (NH4)2SO4 was performed on a column of Butyl sepharose using gradient #3 described above. In FIGS. 69A and 69B the purified conjugate fraction appears in fraction F2.
Example 70
Purification of HSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-1 analogue diluted into 9 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 1.75M (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #6 described above. In FIG. 70 the purified conjugate fraction appears in fraction B.
Example 71
Purification of HSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-1 analogue diluted into 9 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 1.75M magnesium sulfate, was performed on a column of Butyl sepharose using the gradient #6 described above. In FIG. 71 the purified conjugate fraction appears in fraction F2.
Example 72
Purification of HSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
Example with 750 mM ammonium sulfate The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-1 analogue diluted into 9 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 72 the purified conjugate fraction appears in fraction F2.
Example 73
Purification of HSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
Example with 1.75M ammonium phosphate The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-1 analogue diluted into 9 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 1.75M ammonium phosphate, was performed on a column of Butyl sepharose using the gradient #6 described above. In FIG. 73 the purified conjugate fraction appears in fraction B.
Example 74
Purification of HSA:First GLP-1 Analogue (SEQ ID NO:1) Conjugate
-
The first GLP-1 analogue is GLP-1 (7-36) dAla8 Lys37 (ε-AEEA-MPA)-CONH2 and his sequence is shown above in Example 1.
-
Example with 750 mM ammonium phosphate The purification of a conjugate made from reacting 1 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-1 analogue diluted into 9 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 750 mM ammonium phosphate, was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 74 the purified conjugate fraction appears in fraction F2.
Example 75
Purification of HSA:First GLP-2 Analogue (SEQ ID NO:52) Conjugate
-
The first GLP-2 analogue is GLP-2 (1-33) Gly2 Lys34 (ε-MPA)-CONH2 and has the following sequence:
-
| |
HGDGSFSDEMNTILDNLAARDFINWLIQTKITDK(MPA)-CONH2 |
|
-
The purification of a conjugate made from reacting 2 ml 25% 250 mg/ml HSA (Cortex-Biochem, San Leandro, Calif.) with 1 mM first GLP-2 analogue diluted into 14 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 75 the purified conjugate fraction appears in fraction F2.
Example 76
Purification of RSA:First GLP-2 Analogue (SEQ ID NO:52) Conjugate
-
The first GLP-2 analogue is GLP-2 (1-33) Gly2 Lys34 (ε-MPA)-CONH2 and his sequence is shown in Example 75.
-
The purification of a conjugate made from reacting 9 ml 25% 250 mg/ml RSA (rat serum albumin) with 1 mM first GLP-2 analogue diluted into 14 ml of buffer made of 20 mM sodium phosphate buffer pH 7.0, 5 mM sodium caprylate and 750 mM (NH4)2SO4, was performed on a column of Butyl sepharose using the gradient #1 described above. In FIG. 76 the purified conjugate fraction appears in fraction F2.
-
While the invention has been described in connection with specific embodiments thereof, it will be understood that it is capable of further modifications and this application is intended to cover any variations, uses, or adaptations of the invention following, in general, the principles of the invention and including such departures from the present disclosure as come within known or customary practice within the art to which the invention pertains and as may be applied to the essential features hereinbefore set forth, and as follows in the scope of the appended claims.