US20040030356A1 - Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values - Google Patents
Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values Download PDFInfo
- Publication number
- US20040030356A1 US20040030356A1 US10/402,230 US40223003A US2004030356A1 US 20040030356 A1 US20040030356 A1 US 20040030356A1 US 40223003 A US40223003 A US 40223003A US 2004030356 A1 US2004030356 A1 US 2004030356A1
- Authority
- US
- United States
- Prior art keywords
- pacing
- pacemaker
- parameter values
- cardiac
- pacing parameter
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Abandoned
Links
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61N—ELECTROTHERAPY; MAGNETOTHERAPY; RADIATION THERAPY; ULTRASOUND THERAPY
- A61N1/00—Electrotherapy; Circuits therefor
- A61N1/18—Applying electric currents by contact electrodes
- A61N1/32—Applying electric currents by contact electrodes alternating or intermittent currents
- A61N1/36—Applying electric currents by contact electrodes alternating or intermittent currents for stimulation
- A61N1/362—Heart stimulators
- A61N1/365—Heart stimulators controlled by a physiological parameter, e.g. heart potential
- A61N1/368—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61N—ELECTROTHERAPY; MAGNETOTHERAPY; RADIATION THERAPY; ULTRASOUND THERAPY
- A61N1/00—Electrotherapy; Circuits therefor
- A61N1/18—Applying electric currents by contact electrodes
- A61N1/32—Applying electric currents by contact electrodes alternating or intermittent currents
- A61N1/36—Applying electric currents by contact electrodes alternating or intermittent currents for stimulation
- A61N1/362—Heart stimulators
- A61N1/365—Heart stimulators controlled by a physiological parameter, e.g. heart potential
- A61N1/368—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions
- A61N1/3684—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions for stimulating the heart at multiple sites of the ventricle or the atrium
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61N—ELECTROTHERAPY; MAGNETOTHERAPY; RADIATION THERAPY; ULTRASOUND THERAPY
- A61N1/00—Electrotherapy; Circuits therefor
- A61N1/18—Applying electric currents by contact electrodes
- A61N1/32—Applying electric currents by contact electrodes alternating or intermittent currents
- A61N1/36—Applying electric currents by contact electrodes alternating or intermittent currents for stimulation
- A61N1/362—Heart stimulators
- A61N1/3627—Heart stimulators for treating a mechanical deficiency of the heart, e.g. congestive heart failure or cardiomyopathy
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61N—ELECTROTHERAPY; MAGNETOTHERAPY; RADIATION THERAPY; ULTRASOUND THERAPY
- A61N1/00—Electrotherapy; Circuits therefor
- A61N1/18—Applying electric currents by contact electrodes
- A61N1/32—Applying electric currents by contact electrodes alternating or intermittent currents
- A61N1/36—Applying electric currents by contact electrodes alternating or intermittent currents for stimulation
- A61N1/362—Heart stimulators
- A61N1/365—Heart stimulators controlled by a physiological parameter, e.g. heart potential
- A61N1/368—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions
- A61N1/3682—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions with a variable atrioventricular delay
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61N—ELECTROTHERAPY; MAGNETOTHERAPY; RADIATION THERAPY; ULTRASOUND THERAPY
- A61N1/00—Electrotherapy; Circuits therefor
- A61N1/18—Applying electric currents by contact electrodes
- A61N1/32—Applying electric currents by contact electrodes alternating or intermittent currents
- A61N1/36—Applying electric currents by contact electrodes alternating or intermittent currents for stimulation
- A61N1/362—Heart stimulators
- A61N1/365—Heart stimulators controlled by a physiological parameter, e.g. heart potential
- A61N1/368—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions
- A61N1/3684—Heart stimulators controlled by a physiological parameter, e.g. heart potential comprising more than one electrode co-operating with different heart regions for stimulating the heart at multiple sites of the ventricle or the atrium
- A61N1/36843—Bi-ventricular stimulation
Definitions
- the invention relates generally to cardiac rhythm management, and more particularly to a combination of cardiac pacing and optimizing pacing parameter values.
- Dual-Chamber pacemakers are used increasingly in patients with varying degrees of heart block, symptomatic bradydysrhythmias, and drug-refractory cardiomyopathy.
- Clinical benefits of the dual-chamber pacemaker include enhancement of forward blood flow, a feature that can alleviate symptoms of congestive heart failure (CHF), and prevention of atrial fibrillation caused by the atria contracting against a closed valve (Gadler F, Linde C, Darpo B. Modification of atrioventricular conduction as adjunct therapy for pacemaker-treated patients with hypertrophic obstructive cardiomyopathy. Eur Heart J 1998; 19:132-138).
- CHF congestive heart failure
- atrial fibrillation caused by the atria contracting against a closed valve
- Dual-chamber pacing can improve hemodynamics in some patients with dilated cardiomyopathy, likely by abolishing diastolic mitral regurgitation through the establishment of mechanical atrial and ventricular synchrony (Nishimura R, Hayes D, Holmes D, Tajik A. Mechanism of hemodynamic improvement by dual-chamber pacing for severe left ventricular dysfunction: An acute Doppler and catheterization hemodynamic study. J Am Coil Cardiol 1995; 25:281-288).
- AV atrioventricular
- dual-chamber pacemakers often are left at the default value, which the manufacturer sets to approximately 170 milliseconds (Kindermann M, Frohlig G, Doerr T, Schieffer H.
- the goal of AV optimization is the synchronization of the completion of end-diastolic filling exactly at the onset of left ventricular contraction. Obviously, to accomplish this objective, precise physiological measurements of the events of the cardiac cycle must be obtained. Because of a wide range of cardiac conditions, status of the ventricles, and cardioactive medications, each and every patient is unique. Leonelli et al. (Leonelli F, Wang K, Youssef M, Brown D. Systolic and diastolic effects of variable atrioventricular delay in patients with pacemakers. Eur Heart J 1995; 15:1431-1440) observed that an optimal setting of the AV delay value improved stroke volume up to 42%.
- biventricular pacing may offer some important options in the treatment of patients with congestive heart failure (CHF).
- CHF congestive heart failure
- a significant percentage of patients with CHF have conduction abnormalities on EGG. These conduction abnormalities result in abnormal activation of ventricular myocardium and asynchronous activation of the atrial and ventricular chambers.
- Biventricular pacing attempts to activate the right and left ventricles simultaneously, producing what is termed “ventricular resynchronization”.
- TEB thoracic electrical bioimpedance
- Rate-responsive cardiac pacemakers address the adaptation of the pacing rate according to the physiological demands related to the activity of the pacemaker patient. Sensors determine, for example, posture and movement of the patient, or respiration, characterized by respiration rate and tidal volume, and even stroke volume by measurement of thoracic electrical bioimpedance.
- the pacemaker adapts the pacing rate depending on the information obtained by the sensors and processed usually by the pacemaker.
- the pacemaker's rate adapted to the patient's activity is not within the scope of the aforementioned optimization techniques, and the invention.
- the new method and apparatus defined in the appended claims incorporate a cardiac pacemaker and thoracic electrical bioimpedance (TEB) measuring approach.
- TEB diagnostic
- pacemaker therapeutic method and apparatus
- a specific optimization cycle triggered by an operator or upon the expiration of a preset time interval, automatically permutates the values of one or more pacing parameters, such as AV delays, inter-atrial delay, inter-ventricular delay, or heart rate, within operator-defined ranges, and determines at each permutation of parameter values hemodynamic parameters, such as stroke volume (SV), cardiac output (CO), ejection fraction (EF), and other indices of ventricular performance.
- pacing parameters such as AV delays, inter-atrial delay, inter-ventricular delay, or heart rate
- the operator defines one or more pacing parameters, such as atrioventricular delays, inter-atrial delay, inter-ventricular delay, or heart rate, which are subject to variation during an optimization cycle. Furthermore, the operator defines a variation range for values of each pacing parameter and a variation step width for stepping through the variation range during the optimization cycle. The number of pacing parameters subject to variation and the number of applicable variation steps for each parameter determine the number of permutations of pacing parameter values and, thus, the sequence of the optimization cycle. Each permutation of pacing parameter values is applied, for example, for a pre-defined period in the range of 30 to 120 seconds.
- the pacing parameter value which results in the maximum value of a hemodynamic parameter, or a combination thereof, is the output of the optimization cycle and adapted by the cardiac pacemaker for further stimulation.
- the optimization cycle automatically executed for a number of permutations of pacing parameter values to obtain maximal left-ventricular function enhances significantly the time-efficacy of an otherwise cumbersome and time-consuming, but nevertheless beneficial method.
- This automatic optimization method can be applied during pacing system analysis (PSA) prior to permanent pacemaker implantation, during temporary pacing following cardiothoracic surgery, during follow-up of a patient with an implantable pacemaker, or during the investigation of efficacy of pacing algorithms for patients undergoing treatment for congestive heart failure (CHF).
- PSA pacing system analysis
- CHF congestive heart failure
- FIG. 1 illustrates a first preferred embodiment where the optimization apparatus and the cardiac pacemaker are integrated into one system.
- FIG. 2 illustrates a second preferred embodiment where the optimization apparatus and the cardiac pacemaker are separate units.
- FIG. 3 illustrates a flowchart about the various steps of the automatic optimization process.
- FIG. 4 illustrates schematically the sensing and pacing sequence of the AVV-Mode.
- FIG. 5 illustrates the sensing and pacing sequence of the AVAV-Mode.
- FIG. 1 illustrates a first preferred embodiment which is employed, for example, but not limited to, in a Pacing System Analyzer (PSA) or external cardiac pulse generator (temporary cardiac pacemaker).
- PSA Pacing System Analyzer
- external cardiac pulse generator temporary cardiac pacemaker
- FIG. 1 shows a patient 10 and his stylized heart containing four chambers: right atrium 12 , right ventricle 14 , left atrium 16 and left ventricle 18 .
- surface ECG-type electrodes as part of an electrode array are attached to the patient's right side of neck and the left side of lower thorax.
- the outer surface electrodes 20 , 22 are connected to the alternating current (AC) source 122 of the heart monitor 120 , which is part of the optimization apparatus 100 .
- the inner surface electrodes 24 , 26 are connected to the voltmeter 124 of the heart monitor 120 .
- the heart monitor 120 determines from the ratio of the AC applied by 122 and the voltage measured by 124 the thoracic electrical bioimpedance.
- the heart monitor 120 determines from the reciprocal ratio of the AG applied by 122 and the voltage measured by 124 the thoracic electrical bioadmittance. This method is described in the above-mentioned Osypka EP application No. 02007310.2 which is herein incorporated by reference, which describes how the continuous measurement of thoracic electrical bioimpedance is used to determine stroke volume and cardiac output.
- the thoracic electrical bioimpedance can be measured using different electrode configurations, including a second electrode array, and electrodes located on an esophageal catheter/probe, all described in Osypka EP Application No. 02007310.2.
- a cardiac pacemaker 130 integrated into 100 is connected to at least two heart chambers of right atrium (RA) 12 , right ventricle (RV) 14 , left atrium (LA) 16 and left ventricle (LV) 18 .
- the connection of the heart chambers and the apparatus is accomplished by permanent pacing leads (indicated by the dashed part of the connection 30 to the right atrium 12 , the dashed part of the connection 32 to the right ventricle 14 , the dashed part of the connection 34 to the left atrium 16 , and the dashed part of the connection 36 to the left ventricle 18 ), all of which are later connected to an implantable pacemaker, and extension cables (indicated by the solid part of the connection 30 to the right atrium 12 , the solid part of the connection 32 to the right ventricle 14 , the solid part of the connection 34 to the left atrium 16 , and the solid part of the connection 36 to the left ventricle 18
- the processing unit 110 of the optimization apparatus 100 processes the permutations of the pacing parameter values, such as heart rate, and atrioventricular (AV), inter-atrial (AA) and inter-ventricular (VV) delays, and records the corresponding measurements of stroke volume, cardiac output, ejection fraction (EF) and other indices of ventricular performance.
- the pacing parameter values such as heart rate, and atrioventricular (AV), inter-atrial (AA) and inter-ventricular (VV) delays
- a specific optimization cycle triggered by an operator or upon the expiration of a preset time interval, automatically varies one or more pacing parameters, such as AV delays, inter-atrial delay, inter-ventricular delay, or heart rate, within operator-defined ranges, and determines at each parameter setting hemodynamic parameters, such as stroke volume (SV), cardiac output (GO), and other indices of ventricular performance.
- pacing parameters such as AV delays, inter-atrial delay, inter-ventricular delay, or heart rate
- hemodynamic parameters such as stroke volume (SV), cardiac output (GO), and other indices of ventricular performance.
- Each application of set pacing parameters is applied, for example, but not limited to, for a period in the range of 30 to 120 seconds.
- the processing unit records the hemodynamic parameters with each permutation of pacing parameter values, and, upon completion of the optimization cycle, indicates the permutation of pacing parameter values leading to optimal stroke volume, cardiac output and other indices of ventricular performance.
- results are numerically of graphically shown on a display 140 .
- patient demographic parameters such as name, age, and weight
- the optimization apparatus 100 features an interface 150 to a keyboard or a port allowing communication with peripheral devices.
- Typical applications for the aforementioned preferred embodiment are, but not limited to, Pacing System Analysis (PSA) with permanent pacing leads connected to the apparatus, Temporary Pacing (T.P.) after cardiac surgery using temporary myocardial pacing leads (heart wires), and temporary pacing treatment of congestive heart failure (CHF Pacing).
- PSA Pacing System Analysis
- T.P. Temporary Pacing
- CHF Pacing temporary pacing treatment of congestive heart failure
- FIG. 2 illustrates a second preferred embodiment which employs, for example, but not limited to, in a combination of a permanent cardiac pacemaker and a corresponding external programmer for permanent pacemakers, with or without an Pacing System Analyzer (PSA) integrated into the programmer.
- PSA Pacing System Analyzer
- this embodiment is employed, for example, but not limited to, in a combination of a temporary cardiac pulse generator (temporary cardiac pacemaker) and a hemodynamic measurement unit interfacing with the pulse generator.
- FIG. 2 shows the patient 10 after implantation of a permanent cardiac pacemaker 170 .
- the cardiac pacemaker 170 is connected to at least two heart chambers of right atrium (RA) 12 via a permanent pacing lead 172 , right ventricle (RV) 14 via a permanent pacing lead 174 , left atrium (LA) 16 via a permanent pacing lead 176 , and left ventricle (LV) 18 via a permanent pacing lead 178 .
- FIG. 2 shows the connections from the permanent cardiac pacemaker to the heart chambers, i.e. the pacing leads, by dashed lines to indicate that these pacemaker leads are implanted into the patient and, thus, not part of the optimization apparatus.
- the optimization apparatus 100 incorporates a heart monitor 120 , a display 140 , an interface 150 , all controlled by a processing unit 110 .
- the optimization apparatus communicates with the permanent cardiac pacemaker through the interface 150 and an external pacemaker telemetry unit 160 , which, for example, is provided by the manufacturer of the permanent cardiac pacemaker 170 .
- the telemetry unit 160 is integrated into the optimization apparatus, which is indicated by the dashed lines 162 extending the apparatus 100 .
- the communication between the optimization apparatus 100 and the permanent pacemaker 170 is important to synchronize any new permutation of pacing parameter values with the corresponding hemodynamic parameter measurements performed by the optimization apparatus 100 . If no communication can be established, then, at least, the physician programming the cardiac pacemaker 170 and operating the optimization apparatus 100 must know and record the related set pacing and measured hemodynamic parameters.
- surface ECG-type electrodes as part of an electrode array are attached to the patient's right side of neck and the left side of lower thorax.
- the outer surface electrodes 20 , 22 are connected to the alternating current (AC) source 122 of the heart monitor 120 , which is part of the optimization apparatus 100 .
- the inner surface electrodes 24 , 26 are connected to the voltmeter 124 of the heart monitor 120 .
- the heart monitor 120 determines from the ratio of the AC applied by 122 and the voltage measured by 124 the thoracic electrical bioimpedance.
- the heart monitor 120 determines from the reciprocal ratio of the AC applied by 122 and the voltage measured by 124 the thoracic electrical bioadmittance.
- the above-mentioned Osypka EP application No. 02007310.2 which is herein incorporated by reference, describes how the continuous measurement of thoracic electrical bioimpedance is used to determine stroke volume and cardiac output.
- the thoracic electrical bioimpedance can be measured using different electrode configurations, including a second electrode array, and electrodes located on an esophageal catheter/probe, all described in the above-mentioned Osypka EP application No. 02007310.2.
- Typical applications for the aforementioned preferred embodiment are, but not limited to, the examination of a pacemaker patient upon a follow-up visit, and hemodynamic optimization during temporary pacing after cardiothoracic surgery.
- FIG. 3 illustrates a flowchart about the various steps of the optimization process.
- FIG. 3 illustrates a generalized flowchart about the preparation steps of the optimization cycle, i.e. the process which executes the defined number of permutations of pacing parameter values and leads to a permutation of pacing parameter values providing the patient with maximum stroke volume, cardiac output, and other indices of ventricular performance, or any combination thereof.
- the pacemaker which mayor may not be an integral part of the optimization apparatus, is connected to the pacing leads.
- the pacing leads are already part of the implanted pacemaker system.
- the cardiac pacemaker is stimulating on demand, or, asynchronously to the heart rhythm, with a fixed pacing rate 302 .
- the physician decides whether the heart monitor integrated into the optimization apparatus utilizes the transthoracic electrical bioimpedance approach, where the alternating current is applied, and the resulting voltage measured, through surface electrodes 304 .
- the esophageal approach is utilized, where the alternating current is applied, and the resulting voltage measured, through electrodes located on an esophageal catheteprobe 306 .
- the operator defines the pacing parameter, namely the heart rate 310 , defines or determines the variation range for the value of the pacing parameter, and the variation step width for stepping through the variation range of the heart rate 310 .
- the heart rate can be set to a fixed value, with no range to vary.
- the operator determines the variation range, and the variation step width, for the atrioventricular (AV) delay 312 .
- AV-Delay meant to be the right-sided AV-Delay
- the AV-Delay can be set to a fixed value, with no range to vary.
- the operator determines the variation range, and the variation step width, for the inter-atrial (M) delay 314 .
- M-Delay meant to be the time delay applied between sensing or stimulation in the right atrium and stimulation in the left atrium.
- the M-Delay can be set to a fixed value, for example to 0 ms, with no range to vary .
- LAV-Delay is meant to be the left-sided AV-Delay, the time delay applied between sensing or stimulation in the left atrium and stimulation in the left ventricle.
- the LAV-Delay can be set to a fixed value, with no range to vary.
- VV-Delay meant to be the time delay applied between sensing or stimulation in the right ventricle and stimulation in the left ventricle.
- the VV-Delay can be set to a fixed value, for example to 0 ms, with no range to vary .
- the operator determines the time interval between a variation of pacing parameter values 320 .
- the patient's hemodynamic response may take several cardiac cycles to establish. Consequently, the measurement of hemodynamic parameters immediately after the application of a new permutation of pacing parameter values may not reflect the actual hemodynamic changes induced by the changed pacing therapy. For example, within the later optimization cycle, each permutation of pacing parameters shall be held constant for 30 seconds, and measurements of the first cardiac cycles upon each permutation applied may be ignored.
- the order of setting the variation ranges and variation step width for heart rate 310 , M-Delay 314 , AV-Delay 316 , VV-Delay 318 and time interval 320 is arbitrary and can be changed.
- the physician When setting the variation ranges and variation step widths, as well as the time interval, the physician must take into account that there is a compromise between wide ranges and close step widths of pacing parameters values, and the time the automatic optimization cycle will take, that is, the time the patient can be exposed to the measurements.
- the optimization apparatus Upon set pacing parameter variation ranges and variation step widths, the optimization apparatus calculates and displays the time required for the automatic optimization cycle or scan 330 . Depending on the calculated time and the time restrictions the patient's state of heath or situation mandates, the physician is able to readjust the previously set ranges and step widths. In the event the time required for the automatic optimization cycle is acceptable, the physician confirms the start of the automatic optimization cycle through the predefined pacing parameter variation ranges with the predefined variation step widths. The optimization apparatus stores the default set of pacing parameters prior to the start of the automatic optimization cycle, which can be reset upon termination of the automatic optimization cycle.
- the hemodynamic parameter values obtained are displayed with the corresponding permutations of pacing parameter values.
- the results are displayed in form of a table, with the permutation of pacing parameter values leading to maximum stroke volume, cardiac output, ejection fraction and other indices of ventricular performance, marked.
- two- or three-dimensional graphs are utilized to display a spectrum of pacing parameter value sets and their therapeutical impact on this particular patient.
- the physician then has the choice of applying a preferred permutation of pacing parameter values parameter set, or a modification of it, for therapy, or return to the previously used and stored default set of pacing parameter values 350 .
- any new placement of permanent pacing leads may suggest the execution of a new automatic optimization cycle 360 .
- the physician has the option to reprogram the previously set pacing parameter value ranges and variation step widths 362 , or initiate a new automatic optimization cycle with the pacing parameter ranges and step widths previously used 364 .
- the pacemaker optimization is ended 370 .
- FIG. 4 illustrates schematically the sensing and pacing sequence of the AVV-Mode.
- FIG. 4 illustrates schematically the four heart chambers, and their respective sensing and pacing channels, right atrium (RA) 200 , right ventricle (RV) 202 , left atrium (LA) 204 , and left ventricle (LV) 206 , and a preferred operating mode (AVV Mode) of the cardiac pacemaker integrated into the optimization apparatus of FIG. 1.
- the pacemaker provides the functions to measure (sense) in each heart chamber the intrinsic activity, if extant, and to deliver a pacing stimulus.
- the AV-Delay 210 is the programmed atrioventricular pacing interval, initiated by an atrial stimulus.
- the M Delay 212 is the programmed inter-atrial pacing interval, initiated by an atrial stimulus.
- the W-Delay 214 is the programmed inter-ventricular pacing interval, initiated by a ventricular stimulus.
- FIG. 4 illustrates the most complex sensing and pacing therapy the AVV Mode provides.
- the function of the complex cardiac is reduced to known and established pacing modes.
- the left-atrial channel is disabled.
- the three heart chambers remaining, and their respective sensing and pacing channels 216 , right atrium (RA) 200 , right ventricle (RV) 202 , and left ventricle (LV) 206 are of particular interest in pacing therapy addressing congestive heart failure, known as biventricular, or CHF, pacing.
- RA right atrium
- RV right ventricle
- LV left ventricle
- FIG. 5 illustrates schematically the sensing and pacing sequence of the AVAV-Mode.
- FIG. 5 illustrates schematically the 4 heart chambers, and their respective sensing and pacing channels, right atrium (RA) 200 , right ventricle (RV) 202 , left atrium (LA) 204 , and left ventricle (LV) 206 , and another preferred operating mode (AVAV Mode) of the cardiac pacemaker integrated into the optimization apparatus of FIG. 1.
- the pacemaker provides the functions to measure (sense) in each heart chamber the intrinsic activity, if extant, and to deliver a pacing stimulus.
- the AV-Delay 210 is the programmed right-sided atrioventricular pacing interval, initiated by an atrial stimulus.
- the AA Delay 212 is the programmed inter-atrial pacing interval, initiated by an atrial stimulus.
- the LAV-Delay 220 is the programmed left-sided atrioventricular pacing interval, initiated by a left-atrial stimulus.
- CO Cardiac Output measured in liters/minute
- HR Heart rate measured in beats/minute
- V EFF Volume of electrically participating tissue
- T RR R-R interval
- T LVE Left-ventricular ejection time
- FT C Corrected flow time
- V EFF is a factor, which is typical for a particular patient, as it is derived, among other factors, from the patient's weight. V EFF is considered quasi-constant, because, according to the afore-mentioned Osypka EP application No. 02007310.2, V EFF depends also on the basic impedance Z 0 . Considering the scope of possible applications, which require only several minutes for the optimization process, Z 0 varies, if at all, only by a small margin, and has practically no measurable influence on the SV or CO measured. If Z 0 and, consequently, V EFF being constant during the entire application for a particular patient, optimization without compromising accuracy can be achieved without knowledge of the patient's weight and, thus, VEFF.
- SI 1 ( ⁇ ( ⁇ Z ⁇ ( t ) ⁇ t ) MIN ⁇ Z 0 ) n ⁇ ( 1 T RR ) m ⁇ T LVE
- SI 2 ⁇ ( ⁇ Z ⁇ ( t ) ⁇ t ) MIN ⁇ ⁇ ⁇ FT C
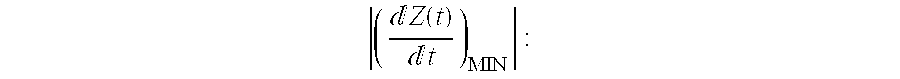
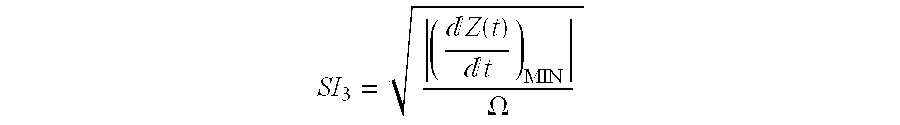
- a “Stroke Index” SI 4 is determined by normalizing ⁇ ( ⁇ Z ⁇ ( t ) ⁇ t ) MIN ⁇
- T LVE omitting corrected flow time FT C or left-ventricular ejection time (known also as systolic flow time) T LVE is a simplification that compromises accuracy and may be suitable only within a narrow range of applicable heart rates.
- Stroke volume, cardiac output and the aforementioned “Stroke Indices” are, within their constraints, suitable hemodynamic parameters for determination of the optimal setting of pacing parameters.
- Ejection Fraction EF is an at least as suitable hemodynamic index for pacing parameter optimization.
Abstract
For cardiac rhythm management a combination of cardiac pacing and a noninvasive heart monitoring is proposed for the determination of a set of programmable pacing parameters hemodynamically most beneficial to the patient. The apparatus incorporates a cardiac pacemaker (130) and a thoracic electrical bioimpedance (TEB) heart monitor (120). This combination allows the creation of a closed-loop system that conveniently and effectively obtains pacing parameter settings providing hemodynamically optimal pacing therapy to the patient as determined by measuring and recording of stroke volume (SV), cardiac output (GO), and other indices of ventricular performance by the heart monitor during an optimization cycle automatically employing different permutations of values of pacing parameters such as atrioventricular delays, inter-atrial delay, inter-ventricular delay, or heart rate, that are sequentially programmed to the pacemaker. The hemodynamically optimal permutation of pacing parameter values is determined from all recordings and programmed to the pacemaker for permanent or temporary pacing therapy.
Description
- The invention relates generally to cardiac rhythm management, and more particularly to a combination of cardiac pacing and optimizing pacing parameter values.
- Dual-Chamber Pacemakers
- Dual-Chamber pacemakers are used increasingly in patients with varying degrees of heart block, symptomatic bradydysrhythmias, and drug-refractory cardiomyopathy. Clinical benefits of the dual-chamber pacemaker include enhancement of forward blood flow, a feature that can alleviate symptoms of congestive heart failure (CHF), and prevention of atrial fibrillation caused by the atria contracting against a closed valve (Gadler F, Linde C, Darpo B. Modification of atrioventricular conduction as adjunct therapy for pacemaker-treated patients with hypertrophic obstructive cardiomyopathy. Eur Heart J 1998; 19:132-138).
- Dual-chamber pacing can improve hemodynamics in some patients with dilated cardiomyopathy, likely by abolishing diastolic mitral regurgitation through the establishment of mechanical atrial and ventricular synchrony (Nishimura R, Hayes D, Holmes D, Tajik A. Mechanism of hemodynamic improvement by dual-chamber pacing for severe left ventricular dysfunction: An acute Doppler and catheterization hemodynamic study. J Am Coil Cardiol 1995; 25:281-288). Despite the benefit of optimization of atrioventricular (AV) delay, dual-chamber pacemakers often are left at the default value, which the manufacturer sets to approximately 170 milliseconds (Kindermann M, Frohlig G, Doerr T, Schieffer H. Optimizing the AV delay in DDD pacemakers with high degree AVE block: Mitral valve Doppler versus impedance cardiography. Pacing Clin Electrophysiol 1997; 20: 2453-2462). It is the consensus of independent researchers that optimization of AV interval is not routinely performed. Procedures for pacemaker optimization, specifically obtaining stroke volume measurements at different AV intervals by aortic Doppler echocardiography , traditionally have been observer-dependent, time-consuming, and costly.
- The goal of AV optimization is the synchronization of the completion of end-diastolic filling exactly at the onset of left ventricular contraction. Obviously, to accomplish this objective, precise physiological measurements of the events of the cardiac cycle must be obtained. Because of a wide range of cardiac conditions, status of the ventricles, and cardioactive medications, each and every patient is unique. Leonelli et al. (Leonelli F, Wang K, Youssef M, Brown D. Systolic and diastolic effects of variable atrioventricular delay in patients with pacemakers. Eur Heart J 1995; 15:1431-1440) observed that an optimal setting of the AV delay value improved stroke volume up to 42%.
- Another application of cardiac pacemakers has recently been discovered: Recent reports are suggesting that biventricular pacing may offer some important options in the treatment of patients with congestive heart failure (CHF). A significant percentage of patients with CHF have conduction abnormalities on EGG. These conduction abnormalities result in abnormal activation of ventricular myocardium and asynchronous activation of the atrial and ventricular chambers. Biventricular pacing attempts to activate the right and left ventricles simultaneously, producing what is termed “ventricular resynchronization”.
- Studies have confirmed acute and short-term hemodynamic benefits of biventricular pacing. In addition, studies have documented improvement in the functional status of patients with CHF. Larger, prospective studies investigating the beneficial effects of biventricular pacing and its clinical implications are currently underway.
- In addition to the symptomatic and functional improvements, other important changes have been noted in CHF patients treated with biventricular pacing. Parameters of cardiac function such as left ventricular dimensions and myocardial performance index have improved markedly. Elevated plasma norepinephrine levels, which are associated with increased mortality in CHF, improve in biventricular pacing. Decreased heart rate variability, also associated with increased risk of sudden death in CHF, has been shown to improve. These findings have lead investigators to hypothesize the potential for biventricular pacing to improve survival. This being said, no trial to date has demonstrated a survival benefit to biventricular pacing. Furthermore, no studies are known that investigate the effects, and potential benefits, of biventricular pacing forcing a small delay between right ventricular and left ventricular contraction, or vice versa.
- Optimization Techniques
- When optimizing the AV delay, or any other delay such as a delay between the contraction of right and left ventricles, it must be tailored to the individual patient. For almost two decades, stroke volume measurements by means of thoracic electrical bioimpedance (TEB) have been favorably considered for optimal determination of pacemaker settings. More recently, Hayes et al. (Hayes D, Hayes S, Hyberger L. Atrioventricular interval optimization technique: Impedance measurements vs Echo/Doppler. Presented at the North American Society for Pacing & Electrophysiology's 19th Annual Scientific Sessions, San Diego, Calif., May 9, 1998) reported that the noninvasive hemodynamic monitoring with TEB permits determination of optimal AV delay within 15 minutes in any clinical settings.
- Despite promising benefits to the patient, the utilization of thoracic electrical bioimpedance (TEB), as with any other aforementioned method, has not been established as a standard optimization procedure for the setting of parameter values of dual-chamber pacemakers. Apparently, the TEB procedure, applied during pacemaker follow-up, is time-consuming and requires active involvement of the physician during the entire optimization period.
- Rate-responsive cardiac pacemakers address the adaptation of the pacing rate according to the physiological demands related to the activity of the pacemaker patient. Sensors determine, for example, posture and movement of the patient, or respiration, characterized by respiration rate and tidal volume, and even stroke volume by measurement of thoracic electrical bioimpedance. The pacemaker adapts the pacing rate depending on the information obtained by the sensors and processed usually by the pacemaker. The pacemaker's rate adapted to the patient's activity is not within the scope of the aforementioned optimization techniques, and the invention.
- The new method and apparatus defined in the appended claims incorporate a cardiac pacemaker and thoracic electrical bioimpedance (TEB) measuring approach. With this combination of a diagnostic (TEB) and therapeutic method and apparatus (pacemaker) a closed-loop system is created to obtain, within its confines, an optimal setting of pacing parameter values.
- In a preferred embodiment, a specific optimization cycle, triggered by an operator or upon the expiration of a preset time interval, automatically permutates the values of one or more pacing parameters, such as AV delays, inter-atrial delay, inter-ventricular delay, or heart rate, within operator-defined ranges, and determines at each permutation of parameter values hemodynamic parameters, such as stroke volume (SV), cardiac output (CO), ejection fraction (EF), and other indices of ventricular performance.
- The operator defines one or more pacing parameters, such as atrioventricular delays, inter-atrial delay, inter-ventricular delay, or heart rate, which are subject to variation during an optimization cycle. Furthermore, the operator defines a variation range for values of each pacing parameter and a variation step width for stepping through the variation range during the optimization cycle. The number of pacing parameters subject to variation and the number of applicable variation steps for each parameter determine the number of permutations of pacing parameter values and, thus, the sequence of the optimization cycle. Each permutation of pacing parameter values is applied, for example, for a pre-defined period in the range of 30 to 120 seconds. The pacing parameter value, which results in the maximum value of a hemodynamic parameter, or a combination thereof, is the output of the optimization cycle and adapted by the cardiac pacemaker for further stimulation.
- The hemodynamic measurements are performed utilizing the apparatus and method of Bernstein and Osypka as described in detail in European patent application No. 02007310.2 of the present applicant, Osypka Medical GmbH, Berlin, for APPARATUS AND METHOD FOR DETERMINING AN APPROXIMATE VALUE OF THE STROKE VOLUME AND THE CARDIAC OUTPUT OF THE HEART, filed concurrently herewith (in the following referred to as the Osypka EP application No. 02007310.2), the disclosure of which is incorporated herein by reference.
- The optimization cycle automatically executed for a number of permutations of pacing parameter values to obtain maximal left-ventricular function enhances significantly the time-efficacy of an otherwise cumbersome and time-consuming, but nevertheless beneficial method. This automatic optimization method can be applied during pacing system analysis (PSA) prior to permanent pacemaker implantation, during temporary pacing following cardiothoracic surgery, during follow-up of a patient with an implantable pacemaker, or during the investigation of efficacy of pacing algorithms for patients undergoing treatment for congestive heart failure (CHF).
- Other objects, features and advantages of the invention will become apparent from the following description of a preferred embodiment of the invention.
- FIG. 1 illustrates a first preferred embodiment where the optimization apparatus and the cardiac pacemaker are integrated into one system.
- FIG. 2 illustrates a second preferred embodiment where the optimization apparatus and the cardiac pacemaker are separate units.
- FIG. 3 illustrates a flowchart about the various steps of the automatic optimization process.
- FIG. 4 illustrates schematically the sensing and pacing sequence of the AVV-Mode.
- FIG. 5 illustrates the sensing and pacing sequence of the AVAV-Mode.
- FIG. 1 illustrates a first preferred embodiment which is employed, for example, but not limited to, in a Pacing System Analyzer (PSA) or external cardiac pulse generator (temporary cardiac pacemaker).
- FIG. 1 shows a
patient 10 and his stylized heart containing four chambers:right atrium 12,right ventricle 14,left atrium 16 andleft ventricle 18. In the preferred embodiment shown, surface ECG-type electrodes as part of an electrode array are attached to the patient's right side of neck and the left side of lower thorax. Theouter surface electrodes source 122 of theheart monitor 120, which is part of theoptimization apparatus 100. Theinner surface electrodes voltmeter 124 of theheart monitor 120. Theheart monitor 120 determines from the ratio of the AC applied by 122 and the voltage measured by 124 the thoracic electrical bioimpedance. - Alternatively, the
heart monitor 120 determines from the reciprocal ratio of the AG applied by 122 and the voltage measured by 124 the thoracic electrical bioadmittance. This method is described in the above-mentioned Osypka EP application No. 02007310.2 which is herein incorporated by reference, which describes how the continuous measurement of thoracic electrical bioimpedance is used to determine stroke volume and cardiac output. - Alternatively, the thoracic electrical bioimpedance (or bioadmittance) can be measured using different electrode configurations, including a second electrode array, and electrodes located on an esophageal catheter/probe, all described in Osypka EP Application No. 02007310.2.
- Furthermore, a
cardiac pacemaker 130 integrated into 100 is connected to at least two heart chambers of right atrium (RA) 12, right ventricle (RV) 14, left atrium (LA) 16 and left ventricle (LV) 18. In the event theoptimization apparatus 100 is used for pacing system analysis, the connection of the heart chambers and the apparatus is accomplished by permanent pacing leads (indicated by the dashed part of theconnection 30 to theright atrium 12, the dashed part of theconnection 32 to theright ventricle 14, the dashed part of theconnection 34 to theleft atrium 16, and the dashed part of theconnection 36 to the left ventricle 18), all of which are later connected to an implantable pacemaker, and extension cables (indicated by the solid part of theconnection 30 to theright atrium 12, the solid part of theconnection 32 to theright ventricle 14, the solid part of theconnection 34 to theleft atrium 16, and the solid part of theconnection 36 to the left ventricle 18). - The
processing unit 110 of theoptimization apparatus 100 processes the permutations of the pacing parameter values, such as heart rate, and atrioventricular (AV), inter-atrial (AA) and inter-ventricular (VV) delays, and records the corresponding measurements of stroke volume, cardiac output, ejection fraction (EF) and other indices of ventricular performance. - According to the invention, a specific optimization cycle, triggered by an operator or upon the expiration of a preset time interval, automatically varies one or more pacing parameters, such as AV delays, inter-atrial delay, inter-ventricular delay, or heart rate, within operator-defined ranges, and determines at each parameter setting hemodynamic parameters, such as stroke volume (SV), cardiac output (GO), and other indices of ventricular performance. Each application of set pacing parameters is applied, for example, but not limited to, for a period in the range of 30 to 120 seconds. The processing unit records the hemodynamic parameters with each permutation of pacing parameter values, and, upon completion of the optimization cycle, indicates the permutation of pacing parameter values leading to optimal stroke volume, cardiac output and other indices of ventricular performance.
- The results are numerically of graphically shown on a
display 140. In the event thedisplay 140 features a touch screen, patient demographic parameters, such as name, age, and weight, can be entered via the touch screen. Alternatively, theoptimization apparatus 100 features aninterface 150 to a keyboard or a port allowing communication with peripheral devices. - Typical applications for the aforementioned preferred embodiment are, but not limited to, Pacing System Analysis (PSA) with permanent pacing leads connected to the apparatus, Temporary Pacing (T.P.) after cardiac surgery using temporary myocardial pacing leads (heart wires), and temporary pacing treatment of congestive heart failure (CHF Pacing).
- FIG. 2 illustrates a second preferred embodiment which employs, for example, but not limited to, in a combination of a permanent cardiac pacemaker and a corresponding external programmer for permanent pacemakers, with or without an Pacing System Analyzer (PSA) integrated into the programmer. With regards to temporary pacing, this embodiment is employed, for example, but not limited to, in a combination of a temporary cardiac pulse generator (temporary cardiac pacemaker) and a hemodynamic measurement unit interfacing with the pulse generator.
- FIG. 2 shows the patient 10 after implantation of a permanent
cardiac pacemaker 170. Thecardiac pacemaker 170 is connected to at least two heart chambers of right atrium (RA) 12 via apermanent pacing lead 172, right ventricle (RV) 14 via apermanent pacing lead 174, left atrium (LA) 16 via apermanent pacing lead 176, and left ventricle (LV) 18 via apermanent pacing lead 178. FIG. 2 shows the connections from the permanent cardiac pacemaker to the heart chambers, i.e. the pacing leads, by dashed lines to indicate that these pacemaker leads are implanted into the patient and, thus, not part of the optimization apparatus. - The
optimization apparatus 100 incorporates aheart monitor 120, adisplay 140, aninterface 150, all controlled by aprocessing unit 110. The optimization apparatus communicates with the permanent cardiac pacemaker through theinterface 150 and an externalpacemaker telemetry unit 160, which, for example, is provided by the manufacturer of the permanentcardiac pacemaker 170. Alternatively, thetelemetry unit 160 is integrated into the optimization apparatus, which is indicated by the dashedlines 162 extending theapparatus 100. - The communication between the
optimization apparatus 100 and thepermanent pacemaker 170 is important to synchronize any new permutation of pacing parameter values with the corresponding hemodynamic parameter measurements performed by theoptimization apparatus 100. If no communication can be established, then, at least, the physician programming thecardiac pacemaker 170 and operating theoptimization apparatus 100 must know and record the related set pacing and measured hemodynamic parameters. - In the preferred embodiment shown, surface ECG-type electrodes as part of an electrode array are attached to the patient's right side of neck and the left side of lower thorax. The
outer surface electrodes source 122 of theheart monitor 120, which is part of theoptimization apparatus 100. Theinner surface electrodes voltmeter 124 of theheart monitor 120. Theheart monitor 120 determines from the ratio of the AC applied by 122 and the voltage measured by 124 the thoracic electrical bioimpedance. - Alternatively, the
heart monitor 120 determines from the reciprocal ratio of the AC applied by 122 and the voltage measured by 124 the thoracic electrical bioadmittance. The above-mentioned Osypka EP application No. 02007310.2, which is herein incorporated by reference, describes how the continuous measurement of thoracic electrical bioimpedance is used to determine stroke volume and cardiac output. - Alternatively, the thoracic electrical bioimpedance (or bioadmittance) can be measured using different electrode configurations, including a second electrode array, and electrodes located on an esophageal catheter/probe, all described in the above-mentioned Osypka EP application No. 02007310.2.
- Typical applications for the aforementioned preferred embodiment are, but not limited to, the examination of a pacemaker patient upon a follow-up visit, and hemodynamic optimization during temporary pacing after cardiothoracic surgery.
- FIG. 3 illustrates a flowchart about the various steps of the optimization process.
- FIG. 3 illustrates a generalized flowchart about the preparation steps of the optimization cycle, i.e. the process which executes the defined number of permutations of pacing parameter values and leads to a permutation of pacing parameter values providing the patient with maximum stroke volume, cardiac output, and other indices of ventricular performance, or any combination thereof.
- Upon
Start 300 of the procedure, the patient is at rest. In order to provide immediate pacing therapy, if required, the pacemaker, which mayor may not be an integral part of the optimization apparatus, is connected to the pacing leads. In the event of pacemaker patient follow-up, the pacing leads are already part of the implanted pacemaker system. The cardiac pacemaker is stimulating on demand, or, asynchronously to the heart rhythm, with a fixedpacing rate 302. The physician decides whether the heart monitor integrated into the optimization apparatus utilizes the transthoracic electrical bioimpedance approach, where the alternating current is applied, and the resulting voltage measured, throughsurface electrodes 304. Alternatively, in patients who are already intubated, the esophageal approach is utilized, where the alternating current is applied, and the resulting voltage measured, through electrodes located on anesophageal catheteprobe 306. - The operator defines the pacing parameter, namely the
heart rate 310, defines or determines the variation range for the value of the pacing parameter, and the variation step width for stepping through the variation range of theheart rate 310. For example, the later optimization cycle for the heart rate shall begin with a heart rate of 70, then increase the heart rate by 5 beats per minute (variation step width=5), until a heart rate of 80 beats per minute. Alternatively, the heart rate can be set to a fixed value, with no range to vary. - The operator determines the variation range, and the variation step width, for the atrioventricular (AV)
delay 312. In this context, with AV-Delay meant to be the right-sided AV-Delay, the time delay applied between sensing or stimulation in the right atrium and stimulation in the right ventricle. For example, the later optimization cycle of the optimization cycle shall begin with an AV-Delay of 150 ms, then increase the AV-Delay by 50 ms (variation step width =50 ms), until an AV-Delay of 250 ms is reached. Alternatively, the AV-Delay can be set to a fixed value, with no range to vary. - The operator determines the variation range, and the variation step width, for the inter-atrial (M)
delay 314. In this context, with M-Delay meant to be the time delay applied between sensing or stimulation in the right atrium and stimulation in the left atrium. For example, the later optimization cycle shall begins with an M-Delay of 0 ms, then increase the M-Delay by 5 ms (variation step width =5 ms), until an M-Delay of 10 ms is reached. Alternatively, the M-Delay can be set to a fixed value, for example to 0 ms, with no range to vary . - The operator determines the variation range, and the variation step width, for the left-sided atrioventricular (LAV)
delay 316. In this context, LAV-Delay is meant to be the left-sided AV-Delay, the time delay applied between sensing or stimulation in the left atrium and stimulation in the left ventricle. For example, the later optimization cycle shall begin with an LAV-Delay of 150 ms, then increase the LAV-Delay by 50 ms (variation step width=50 ms), until an LAV-Delay of 250 ms is reached. Alternatively, the LAV-Delay can be set to a fixed value, with no range to vary. - The operator determines the variation range, and the variation step width, for the inter-ventricular (VV)
delay 314. In this context, with VV-Delay meant to be the time delay applied between sensing or stimulation in the right ventricle and stimulation in the left ventricle. For example, the later optimization cycle shall begin with an W-Delay of 0 ms, then increase the W-Delay by 5 ms (variation step width=5 ms), until a VV-Delay of 10 ms is reached. Alternatively, the VV-Delay can be set to a fixed value, for example to 0 ms, with no range to vary . - The operator determines the time interval between a variation of pacing parameter values 320. Upon a new permutation of pacing parameter values applied for therapy, the patient's hemodynamic response may take several cardiac cycles to establish. Consequently, the measurement of hemodynamic parameters immediately after the application of a new permutation of pacing parameter values may not reflect the actual hemodynamic changes induced by the changed pacing therapy. For example, within the later optimization cycle, each permutation of pacing parameters shall be held constant for 30 seconds, and measurements of the first cardiac cycles upon each permutation applied may be ignored.
- The order of setting the variation ranges and variation step width for
heart rate 310, M-Delay 314, AV-Delay 316, VV-Delay 318 andtime interval 320 is arbitrary and can be changed. When setting the variation ranges and variation step widths, as well as the time interval, the physician must take into account that there is a compromise between wide ranges and close step widths of pacing parameters values, and the time the automatic optimization cycle will take, that is, the time the patient can be exposed to the measurements. - Upon set pacing parameter variation ranges and variation step widths, the optimization apparatus calculates and displays the time required for the automatic optimization cycle or scan 330. Depending on the calculated time and the time restrictions the patient's state of heath or situation mandates, the physician is able to readjust the previously set ranges and step widths. In the event the time required for the automatic optimization cycle is acceptable, the physician confirms the start of the automatic optimization cycle through the predefined pacing parameter variation ranges with the predefined variation step widths. The optimization apparatus stores the default set of pacing parameters prior to the start of the automatic optimization cycle, which can be reset upon termination of the automatic optimization cycle.
- Upon termination of the
optimization cycle 340, the hemodynamic parameter values obtained are displayed with the corresponding permutations of pacing parameter values. The results are displayed in form of a table, with the permutation of pacing parameter values leading to maximum stroke volume, cardiac output, ejection fraction and other indices of ventricular performance, marked. Alternatively, two- or three-dimensional graphs are utilized to display a spectrum of pacing parameter value sets and their therapeutical impact on this particular patient. - The physician then has the choice of applying a preferred permutation of pacing parameter values parameter set, or a modification of it, for therapy, or return to the previously used and stored default set of pacing parameter values 350.
- During pacing system analysis, any new placement of permanent pacing leads may suggest the execution of a new
automatic optimization cycle 360. The physician has the option to reprogram the previously set pacing parameter value ranges andvariation step widths 362, or initiate a new automatic optimization cycle with the pacing parameter ranges and step widths previously used 364. Alternatively, the pacemaker optimization is ended 370. - FIG. 4 illustrates schematically the sensing and pacing sequence of the AVV-Mode.
- FIG. 4 illustrates schematically the four heart chambers, and their respective sensing and pacing channels, right atrium (RA) 200, right ventricle (RV) 202, left atrium (LA) 204, and left ventricle (LV) 206, and a preferred operating mode (AVV Mode) of the cardiac pacemaker integrated into the optimization apparatus of FIG. 1. The pacemaker provides the functions to measure (sense) in each heart chamber the intrinsic activity, if extant, and to deliver a pacing stimulus.
- In this context, the AV-
Delay 210 is the programmed atrioventricular pacing interval, initiated by an atrial stimulus. TheM Delay 212 is the programmed inter-atrial pacing interval, initiated by an atrial stimulus. The W-Delay 214 is the programmed inter-ventricular pacing interval, initiated by a ventricular stimulus. - FIG. 4 illustrates the most complex sensing and pacing therapy the AVV Mode provides. By disabling the pacing and sensing in specific heart chambers, the function of the complex cardiac is reduced to known and established pacing modes. In the event that no left-atrial sensing and stimulation is required, or applicable, the left-atrial channel is disabled. The three heart chambers remaining, and their respective sensing and
pacing channels 216, right atrium (RA) 200, right ventricle (RV) 202, and left ventricle (LV) 206, are of particular interest in pacing therapy addressing congestive heart failure, known as biventricular, or CHF, pacing. To our knowledge, the application of a VV-Delay, which can assume a positive or negative value, has neither been published nor investigated. - Upon disabling pacing and sensing in the left ventricle, the two heart chambers remaining, and their respective sensing and
pacing channels 218, right atrium (RA) 200, and right ventricle (RV) 202, are of particular interest in classical physiological pacing therapy, known as dual-chamber, or DDD, pacing. - FIG. 5 illustrates schematically the sensing and pacing sequence of the AVAV-Mode.
- FIG. 5 illustrates schematically the 4 heart chambers, and their respective sensing and pacing channels, right atrium (RA) 200, right ventricle (RV) 202, left atrium (LA) 204, and left ventricle (LV) 206, and another preferred operating mode (AVAV Mode) of the cardiac pacemaker integrated into the optimization apparatus of FIG. 1. The pacemaker provides the functions to measure (sense) in each heart chamber the intrinsic activity, if extant, and to deliver a pacing stimulus.
- In this context, the AV-
Delay 210 is the programmed right-sided atrioventricular pacing interval, initiated by an atrial stimulus. TheAA Delay 212 is the programmed inter-atrial pacing interval, initiated by an atrial stimulus. The LAV-Delay 220 is the programmed left-sided atrioventricular pacing interval, initiated by a left-atrial stimulus. - Upon disabling pacing and sensing in the left atrium (LA) 204 and ventricle (L V) 206, the 2 heart chambers remaining, and their respective sensing and
pacing channels 218, right atrium (RA) 200, and right ventricle (RV) 202, are of particular interest in classical physiological pacing therapy, known as dual-chamber, or DDD, pacing. - As indicated above, it is not only the stroke volume (SV) that can be used in order to optimize the pacing parameters to be programmed onto the pacemaker. In general, most indices of left-ventricular cardiac performance may be suitable measures for optimization. The optimization apparatus measures in any event the heart rate (HR). Therefore, cardiac output (CO), instead of stroke volume SV may be used for the optimization process:
- where
- SV: Stroke Volume measured in milliliters (mL)
- CO: Cardiac Output measured in liters/minute
- HR: Heart rate measured in beats/minute
-
-
- where V EFF: Volume of electrically participating tissue
-
- Maximum rate of change of impedance
- Z 0: Base impedance
- T RR: R-R interval
- T LVE: Left-ventricular ejection time
-
- V EFF is a factor, which is typical for a particular patient, as it is derived, among other factors, from the patient's weight. VEFF is considered quasi-constant, because, according to the afore-mentioned Osypka EP application No. 02007310.2, VEFF depends also on the basic impedance Z0. Considering the scope of possible applications, which require only several minutes for the optimization process, Z0 varies, if at all, only by a small margin, and has practically no measurable influence on the SV or CO measured. If Z0 and, consequently, VEFF being constant during the entire application for a particular patient, optimization without compromising accuracy can be achieved without knowledge of the patient's weight and, thus, VEFF. For example, a “Stroke Index” SI1 can be determined:
- with 0.15<n<0.8 and 0≦m≦1.5 according to the aforementioned Osypka EP application.
-
- The only shortcoming of such processing is that the user does not obtain (simple) absolute indication of the range in which patient's stroke volume is determined while the patient is undergoing the various permutations of pacing parameter values. The user, however, obtains relative values of “Stroke Indices” to compare.
-
-
-
-
-
- Again, omitting corrected flow time FT C or left-ventricular ejection time (known also as systolic flow time) TLVE is a simplification that compromises accuracy and may be suitable only within a narrow range of applicable heart rates.
- Stroke volume, cardiac output and the aforementioned “Stroke Indices” are, within their constraints, suitable hemodynamic parameters for determination of the optimal setting of pacing parameters. Alternatively, (left-ventricular) Ejection Fraction (EF) is an at least as suitable hemodynamic index for pacing parameter optimization.
Claims (11)
1. Method of automatic determination of a multi-chamber cardiac pacemaker's programmable pacing parameter values providing hemodynamically optimal pacing therapy, comprising
defining one or more pacing parameters, such as atrioventricular delays, inter-atrial delay, inter-ventricular delay, or heart rate, which are subject to variation during an optimization cycle,
defining a variation range for values of each pacing parameter and a variation step width for stepping through the variation range during the optimization cycle,
with the number of pacing parameters subject to variation and the number of applicable variation steps for each parameter defining the number of permutations of pacing parameter values and, thus, the sequence of the optimization cycle,
within an optimization cycle sequentially programming the pacemaker with one permutation of pacing parameter values after the other and taking, with each permutation applied, hemodynamic measurements of the stroke volume (SV), cardiac output (CO) or ejection fraction (EF) and other indices of ventricular performance for a predefined time period, and recording each of the measurements taken,
determining the hemodynamically optimal permutation of pacing parameter values from all recordings, and
programming the pacemaker with this hemodynamically optimal permutation of pacing parameter values for pacing therapy.
2. Method according to claim 1 , characterized in that non-invasive measurements of thoracic electrical bioimpedance (or bioadmittance) are performed to determine stroke volume (SV), cardiac output (CO) or ejection fraction (EF) and other indices of ventricular performance in combination with the cardiac pacemaker.
3. Method according to claim 2 , characterized in that the non-invasive measurements of thoracic electrical bioimpedance (or bioadmittance) are performed using an array of surface electrodes, especially ECG-type electrodes, attached to a patient's right side of his neck and the left side of the lower thorax, or electrodes located on an esophagus catheter/probe.
4. Method according to claim 2 , characterized in that the non-invasive measurements of thoracic electrical bioimpedance (or bioadmittance) are performed using a first array of surface electrodes, especially EGG-type electrodes, attached to a patient's left side of his neck and the left side of the lower thorax and a second array of surface electrodes, especially EGG-type electrodes, attached to a patient's right side of his neck and the right side of the lower thorax, or electrodes located on an esophagus catheter/probe.
5. Method according to any of claims 1 to 4 , characterized in that each permutation of pacing parameter values is applied for a period of about 30 to 120 seconds.
6. Apparatus for automatic determination of a multi-chamber cardiac pacemaker's pacing parameter values providing optimal pacing therapy (optimization apparatus), comprising
a programmable processing unit (110) for storing an operator defined set of one or more programmable pacing parameters subject to variation and operator defined parameter specific variation ranges and step widths of values for pacing parameters, such as atrioventricular delays, inter-atrial delay, inter-ventricular delay, or heart rate, thus defining the number of permutations of pacing parameter values and the sequence of the optimization cycle,
means for programming one permutation of pacing parameter values at a time to a pacemaker (130, 170) in accordance with the defined sequence of the optimization cycle,
a heart monitor (120) for communication with the pacemaker for taking hemodynamic measurements of the stroke volume (SV), cardiac output (GO) or ejection fraction (EF) and other indices of ventricular performance in accordance with the defined sequence of the optimization cycle,
means (110) for recording the measurements for each permutation of applied pacing parameter values,
means (110) for determining the optimal permutation of pacing parameter values from all recordings, and
means (110) for permanently programming the pacemaker with the so found optimal pacing parameter values.
7. Apparatus of claim 6 , characterized in that the cardiac pacemaker (130) is integrated in the optimization apparatus (100).
8. Apparatus of claim 6 , characterized by display means (140) for numerically or graphically displaying the results of the measurements and/or the optimal permutation of pacing parameter values.
9. Any communicate with the cardiac pacemaker (170) through which the pacemaker is programmable by the processing unit (110).
10. Apparatus of claim 6 , characterized in that the pacemaker (170) is programmable in such a way that the optimization cycle is automatically performed according to a program sequence built into the pacemaker, which can be activated, especially by the processing unit (110), in such a way that the hemodynamic measurements obtained by the heart monitor (120) can be related (synchronized) to the various permutations of pacing parameters values.
11. Apparatus of claims 9 or 10, characterized in that the interface (150) is adapted to communicate with the pacemaker (170) a set of pacing parameter values through a telemetry means (160).
Priority Applications (1)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US11/956,669 US8219195B2 (en) | 2002-04-03 | 2007-12-14 | Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| EP02007574.3 | 2002-04-03 | ||
| EP02007574A EP1350539B1 (en) | 2002-04-03 | 2002-04-03 | Apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values |
Related Child Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/956,669 Division US8219195B2 (en) | 2002-04-03 | 2007-12-14 | Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values |
Publications (1)
| Publication Number | Publication Date |
|---|---|
| US20040030356A1 true US20040030356A1 (en) | 2004-02-12 |
Family
ID=27838064
Family Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US10/402,230 Abandoned US20040030356A1 (en) | 2002-04-03 | 2003-03-27 | Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values |
| US11/956,669 Active 2025-12-24 US8219195B2 (en) | 2002-04-03 | 2007-12-14 | Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values |
Family Applications After (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/956,669 Active 2025-12-24 US8219195B2 (en) | 2002-04-03 | 2007-12-14 | Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values |
Country Status (4)
| Country | Link |
|---|---|
| US (2) | US20040030356A1 (en) |
| EP (1) | EP1350539B1 (en) |
| AT (1) | ATE342752T1 (en) |
| DE (1) | DE60215458T2 (en) |
Cited By (19)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20040243192A1 (en) * | 2003-06-02 | 2004-12-02 | Hepp Dennis G. | Physiologic stimulator tuning apparatus and method |
| US20050043895A1 (en) * | 2003-08-20 | 2005-02-24 | Schechter Stuart O. | Method and apparatus for automatically programming CRT devices |
| US20050182447A1 (en) * | 2004-02-14 | 2005-08-18 | Schecter Stuart O. | Optimization of impedance signals for closed loop programming of cardiac resynchronization therapy devices |
| US20060047320A1 (en) * | 2003-12-22 | 2006-03-02 | Cardiac Pacemakers, Inc. | Method and system for delivering cardiac resynchronization therapy with variable atrio-ventricular delay |
| US20060235481A1 (en) * | 2005-04-19 | 2006-10-19 | Cardiac Pacemakers, Inc. | Selective resynchronization therapy optimization based on user preference |
| US20070150013A1 (en) * | 2003-12-22 | 2007-06-28 | Cardiac Pacemakers, Inc.. | Method and system for setting cardiac resynchronization therapy parameters |
| US20070179390A1 (en) * | 2003-08-20 | 2007-08-02 | Pacesettler, Inc. | Global cardiac performance |
| US20070191901A1 (en) * | 2004-06-04 | 2007-08-16 | Pacesetter, Inc. | Quantifying systolic and diastolic cardiac performance from dynamic impedance waveforms |
| US20080091244A1 (en) * | 2006-10-13 | 2008-04-17 | Lifescience Solutions, Llc | Pacemaker |
| US7363077B1 (en) | 2004-11-09 | 2008-04-22 | Pacesetters, Inc. | Adaptive timing interval control method for treating congestive heart failure |
| US20080103539A1 (en) * | 2006-10-30 | 2008-05-01 | Berthold Stegemann | Method, Apparatus and System to Identify Optimal Pacing Parameters Using Sensor Data |
| WO2006061822A3 (en) * | 2004-12-12 | 2009-04-30 | Ai Semi Ltd | Optimizing and monitoring adaptive cardiac resynchronization therapy devices |
| US7627374B1 (en) | 2006-06-02 | 2009-12-01 | Pacesetter, Inc. | System and method for evaluating and optimizing the contribution of particular heart chambers to the overall efficacy of cardiac pacing therapy |
| US20100042173A1 (en) * | 2006-01-11 | 2010-02-18 | Taraneh Ghaffari Farazi | System and method for evaluating and optimizing the contribution of particular heart chambers to the overall efficacy of cardiac pacing therapy |
| US20100125305A1 (en) * | 2008-11-18 | 2010-05-20 | Pacesetter, Inc. | Use of impedance to assess electrode locations |
| EP2241348A2 (en) | 2009-04-15 | 2010-10-20 | Biotronik CRM Patent AG | Heart monitor |
| US20130053918A1 (en) * | 2011-08-30 | 2013-02-28 | Aleksandre T. Sambelashvili | Left-ventricular pacing site selection guided by electrogram morphology analysis |
| JP2013080493A (en) * | 2004-11-09 | 2013-05-02 | Thomson Licensing | Binding of content on separate storage media |
| US9089709B2 (en) | 2004-12-12 | 2015-07-28 | Sorin Crm Sas | System and method for the visualization and optimization of cardiac resynchronization therapy |
Families Citing this family (20)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US7228174B2 (en) | 2002-04-29 | 2007-06-05 | Medtronics, Inc. | Algorithm for the automatic determination of optimal AV an VV intervals |
| EP1703946A2 (en) * | 2003-12-03 | 2006-09-27 | Medtronic, Inc. | Method and apparatus for determining an efficacious atrioventricular delay interval |
| US7239915B2 (en) * | 2003-12-16 | 2007-07-03 | Medtronic, Inc. | Hemodynamic optimization system for biventricular implants |
| EP1768743B1 (en) * | 2004-06-14 | 2012-04-11 | Medtronic, Inc. | Algorithm for the automatic determination of optimal pacing intervals |
| US7917196B2 (en) | 2005-05-09 | 2011-03-29 | Cardiac Pacemakers, Inc. | Arrhythmia discrimination using electrocardiograms sensed from multiple implanted electrodes |
| US7890159B2 (en) | 2004-09-30 | 2011-02-15 | Cardiac Pacemakers, Inc. | Cardiac activation sequence monitoring and tracking |
| US8175703B2 (en) | 2006-01-25 | 2012-05-08 | Cardiac Pacemakers, Inc. | Cardiac resynchronization therapy parameter optimization |
| US8527048B2 (en) | 2006-06-29 | 2013-09-03 | Cardiac Pacemakers, Inc. | Local and non-local sensing for cardiac pacing |
| US8868183B2 (en) | 2006-12-21 | 2014-10-21 | Cardiac Pacemakers, Inc. | Method and apparatus to implement multiple parameter sets in an implantable device |
| WO2008079347A1 (en) * | 2006-12-21 | 2008-07-03 | Cardiac Pacemakers, Inc. | Implantable device with multiple parameter sets |
| US8768466B2 (en) | 2007-10-12 | 2014-07-01 | Cardiac Pacemakers, Inc. | Method and apparatus to trend and optimize an implantable medical device using a patient management system |
| US8321014B2 (en) | 2008-10-06 | 2012-11-27 | Cardiac Pacemakers, Inc. | Dynamic cardiac resynchronization therapy by tracking intrinsic conduction |
| US20100249860A1 (en) * | 2009-03-24 | 2010-09-30 | Shuros Allan C | External cardiac stimulation patch |
| DE102009031232A1 (en) | 2009-06-26 | 2010-12-30 | Universitätsklinikum Jena | Method for implementing e.g. atrium synchronous biventricular stimulation in patient having pacemaker, involves correcting cardiogram based on distance between left atrial excitation and beginning of ventricular excitation |
| US9026209B2 (en) | 2009-07-28 | 2015-05-05 | Biotronik Crm Patent Ag | Ventricular cardiac stimulator |
| US20130211472A1 (en) * | 2010-10-27 | 2013-08-15 | St. Jude Medical Ab | Cardiac resynchronization therapy optimization |
| EP2712549B1 (en) * | 2012-10-01 | 2015-03-11 | Sorin CRM SAS | Device for assessing temporal ventricular dyssynchrony |
| DE102013015074A1 (en) * | 2013-05-15 | 2014-11-20 | Osypka Ag | External pacemaker and method for determining threshold with an external pacemaker |
| EP3368148B1 (en) * | 2015-10-26 | 2022-09-14 | Cardiac Pacemakers, Inc. | Multi-sensor based cardiac stimulation |
| CN110464326B (en) * | 2019-08-19 | 2022-05-10 | 上海联影医疗科技股份有限公司 | Scanning parameter recommendation method, system, device and storage medium |
Citations (8)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US5431691A (en) * | 1992-03-02 | 1995-07-11 | Siemens Pacesetter, Inc. | Method and system for recording and displaying a sequential series of pacing events |
| US5540724A (en) * | 1995-02-03 | 1996-07-30 | Intermedics, Inc. | Cardiac cardioverter/defibrillator with in vivo impedance estimation |
| US5549650A (en) * | 1994-06-13 | 1996-08-27 | Pacesetter, Inc. | System and method for providing hemodynamically optimal pacing therapy |
| US5584868A (en) * | 1992-11-03 | 1996-12-17 | Cardiac Pacemakers, Inc. | Cardiac stimulating apparatus and method for heart failure therapy |
| US5891176A (en) * | 1996-05-09 | 1999-04-06 | Pacesetter, Inc. | System and method for providing hemodynamically optimal pacing |
| US6095987A (en) * | 1996-04-17 | 2000-08-01 | Imagyn Medical Techonologies California, Inc. | Apparatus and methods of bioelectrical impedance analysis of blood flow |
| US6511438B2 (en) * | 2001-04-03 | 2003-01-28 | Osypka Medical Gmbh | Apparatus and method for determining an approximation of the stroke volume and the cardiac output of the heart |
| US6522923B1 (en) * | 2001-02-09 | 2003-02-18 | Pacesetter, Inc. | Methods, systems and devices for optimizing cardiac pacing parameters using evolutionary algorithms |
Family Cites Families (5)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US5540727A (en) * | 1994-11-15 | 1996-07-30 | Cardiac Pacemakers, Inc. | Method and apparatus to automatically optimize the pacing mode and pacing cycle parameters of a dual chamber pacemaker |
| US5685316A (en) * | 1996-04-08 | 1997-11-11 | Rheo-Graphic Pte Ltd. | Non-invasive monitoring of hemodynamic parameters using impedance cardiography |
| US6070100A (en) * | 1997-12-15 | 2000-05-30 | Medtronic Inc. | Pacing system for optimizing cardiac output and determining heart condition |
| WO2001087410A2 (en) * | 2000-05-15 | 2001-11-22 | Pacesetter, Inc. | Cardiac stimulation devices and methods for measuring impedances associated with the left side of the heart |
| US6561986B2 (en) * | 2001-01-17 | 2003-05-13 | Cardiodynamics International Corporation | Method and apparatus for hemodynamic assessment including fiducial point detection |
-
2002
- 2002-04-03 EP EP02007574A patent/EP1350539B1/en not_active Expired - Lifetime
- 2002-04-03 AT AT02007574T patent/ATE342752T1/en active
- 2002-04-03 DE DE60215458T patent/DE60215458T2/en not_active Expired - Lifetime
-
2003
- 2003-03-27 US US10/402,230 patent/US20040030356A1/en not_active Abandoned
-
2007
- 2007-12-14 US US11/956,669 patent/US8219195B2/en active Active
Patent Citations (8)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US5431691A (en) * | 1992-03-02 | 1995-07-11 | Siemens Pacesetter, Inc. | Method and system for recording and displaying a sequential series of pacing events |
| US5584868A (en) * | 1992-11-03 | 1996-12-17 | Cardiac Pacemakers, Inc. | Cardiac stimulating apparatus and method for heart failure therapy |
| US5549650A (en) * | 1994-06-13 | 1996-08-27 | Pacesetter, Inc. | System and method for providing hemodynamically optimal pacing therapy |
| US5540724A (en) * | 1995-02-03 | 1996-07-30 | Intermedics, Inc. | Cardiac cardioverter/defibrillator with in vivo impedance estimation |
| US6095987A (en) * | 1996-04-17 | 2000-08-01 | Imagyn Medical Techonologies California, Inc. | Apparatus and methods of bioelectrical impedance analysis of blood flow |
| US5891176A (en) * | 1996-05-09 | 1999-04-06 | Pacesetter, Inc. | System and method for providing hemodynamically optimal pacing |
| US6522923B1 (en) * | 2001-02-09 | 2003-02-18 | Pacesetter, Inc. | Methods, systems and devices for optimizing cardiac pacing parameters using evolutionary algorithms |
| US6511438B2 (en) * | 2001-04-03 | 2003-01-28 | Osypka Medical Gmbh | Apparatus and method for determining an approximation of the stroke volume and the cardiac output of the heart |
Cited By (41)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20040243192A1 (en) * | 2003-06-02 | 2004-12-02 | Hepp Dennis G. | Physiologic stimulator tuning apparatus and method |
| US20060235480A1 (en) * | 2003-08-20 | 2006-10-19 | Schecter Stuart O | Method and apparatus for automatically programming CRT devices |
| US20050043895A1 (en) * | 2003-08-20 | 2005-02-24 | Schechter Stuart O. | Method and apparatus for automatically programming CRT devices |
| US7653436B2 (en) | 2003-08-20 | 2010-01-26 | Pacesetter, Inc. | Global cardiac performance |
| US20070179390A1 (en) * | 2003-08-20 | 2007-08-02 | Pacesettler, Inc. | Global cardiac performance |
| US7065400B2 (en) | 2003-08-20 | 2006-06-20 | Pacesetter, Inc. | Method and apparatus for automatically programming CRT devices |
| US8121685B2 (en) | 2003-12-22 | 2012-02-21 | Cardiac Pacemakers, Inc. | Method and system for delivering cardiac resynchronization therapy with variable atrio-ventricular delay |
| US20110106202A1 (en) * | 2003-12-22 | 2011-05-05 | Jiang Ding | Method and system for setting cardiac resynchronization therapy parameters |
| US20070150013A1 (en) * | 2003-12-22 | 2007-06-28 | Cardiac Pacemakers, Inc.. | Method and system for setting cardiac resynchronization therapy parameters |
| US20060047320A1 (en) * | 2003-12-22 | 2006-03-02 | Cardiac Pacemakers, Inc. | Method and system for delivering cardiac resynchronization therapy with variable atrio-ventricular delay |
| US8483827B2 (en) | 2003-12-22 | 2013-07-09 | Cardiac Pacemakers, Inc. | Method and system for delivering cardiac resynchronization therapy with variable atrio-ventricular delay |
| US20100069988A1 (en) * | 2003-12-22 | 2010-03-18 | Jiang Ding | Method and system for delivering cardiac resynchronization therapy with variable atrio-ventricular delay |
| US7869873B2 (en) | 2003-12-22 | 2011-01-11 | Cardiac Pacemakers, Inc. | Method and system for setting cardiac resynchronization therapy parameters |
| US8626289B2 (en) | 2003-12-22 | 2014-01-07 | Cardiac Pacemakers, Inc. | Method and system for delivering cardiac resynchronization therapy with variable atrio-ventricular delay |
| US8731660B2 (en) | 2003-12-22 | 2014-05-20 | Cardiac Pacemakers, Inc. | Method and system for setting cardiac resynchronization therapy parameters |
| US7010347B2 (en) | 2004-02-14 | 2006-03-07 | Pacesetter, Inc. | Optimization of impedance signals for closed loop programming of cardiac resynchronization therapy devices |
| US20050182447A1 (en) * | 2004-02-14 | 2005-08-18 | Schecter Stuart O. | Optimization of impedance signals for closed loop programming of cardiac resynchronization therapy devices |
| US20070191901A1 (en) * | 2004-06-04 | 2007-08-16 | Pacesetter, Inc. | Quantifying systolic and diastolic cardiac performance from dynamic impedance waveforms |
| JP2013080493A (en) * | 2004-11-09 | 2013-05-02 | Thomson Licensing | Binding of content on separate storage media |
| US7363077B1 (en) | 2004-11-09 | 2008-04-22 | Pacesetters, Inc. | Adaptive timing interval control method for treating congestive heart failure |
| WO2006061822A3 (en) * | 2004-12-12 | 2009-04-30 | Ai Semi Ltd | Optimizing and monitoring adaptive cardiac resynchronization therapy devices |
| US9089709B2 (en) | 2004-12-12 | 2015-07-28 | Sorin Crm Sas | System and method for the visualization and optimization of cardiac resynchronization therapy |
| US20090292334A1 (en) * | 2004-12-12 | 2009-11-26 | Rami Rom | Optimizing and monitoring adaptive cardiac resynchronization therapy devices |
| US8041426B2 (en) | 2005-04-19 | 2011-10-18 | Cardiac Pacemakers, Inc. | Selective resynchronization therapy optimization based on user preference |
| US20100010557A1 (en) * | 2005-04-19 | 2010-01-14 | Richard Fogoros | Selective resynchronization therapy optimization based on user preference |
| US20060235481A1 (en) * | 2005-04-19 | 2006-10-19 | Cardiac Pacemakers, Inc. | Selective resynchronization therapy optimization based on user preference |
| US7613514B2 (en) * | 2005-04-19 | 2009-11-03 | Cardiac Pacemakers, Inc. | Selective resynchronization therapy optimization based on user preference |
| US20100042173A1 (en) * | 2006-01-11 | 2010-02-18 | Taraneh Ghaffari Farazi | System and method for evaluating and optimizing the contribution of particular heart chambers to the overall efficacy of cardiac pacing therapy |
| US7627374B1 (en) | 2006-06-02 | 2009-12-01 | Pacesetter, Inc. | System and method for evaluating and optimizing the contribution of particular heart chambers to the overall efficacy of cardiac pacing therapy |
| EP2073891A4 (en) * | 2006-10-13 | 2011-02-02 | Lifescience Solutions Llc | Pacemaker |
| EP2073891A2 (en) * | 2006-10-13 | 2009-07-01 | Lifescience Solutions, LLC | Pacemaker |
| US8588904B2 (en) | 2006-10-13 | 2013-11-19 | Lifescience Solutions Llc | Pacemaker |
| US20080091244A1 (en) * | 2006-10-13 | 2008-04-17 | Lifescience Solutions, Llc | Pacemaker |
| US9604063B2 (en) | 2006-10-30 | 2017-03-28 | Medtronic, Inc. | Method, apparatus and system to identify optimal pacing parameters using sensor data |
| US20080103539A1 (en) * | 2006-10-30 | 2008-05-01 | Berthold Stegemann | Method, Apparatus and System to Identify Optimal Pacing Parameters Using Sensor Data |
| US20100125305A1 (en) * | 2008-11-18 | 2010-05-20 | Pacesetter, Inc. | Use of impedance to assess electrode locations |
| US8150512B2 (en) | 2008-11-18 | 2012-04-03 | Pacesetter, Inc. | Use of impedance to assess electrode locations |
| US8521265B2 (en) | 2009-04-15 | 2013-08-27 | Biotronik Crm Patent Ag | Heart monitor |
| DE102009002397A1 (en) | 2009-04-15 | 2010-10-21 | Biotronik Crm Patent Ag | heart monitor |
| EP2241348A2 (en) | 2009-04-15 | 2010-10-20 | Biotronik CRM Patent AG | Heart monitor |
| US20130053918A1 (en) * | 2011-08-30 | 2013-02-28 | Aleksandre T. Sambelashvili | Left-ventricular pacing site selection guided by electrogram morphology analysis |
Also Published As
| Publication number | Publication date |
|---|---|
| US20080103541A1 (en) | 2008-05-01 |
| ATE342752T1 (en) | 2006-11-15 |
| US8219195B2 (en) | 2012-07-10 |
| EP1350539A1 (en) | 2003-10-08 |
| DE60215458D1 (en) | 2006-11-30 |
| DE60215458T2 (en) | 2007-08-23 |
| EP1350539B1 (en) | 2006-10-18 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US8219195B2 (en) | Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values | |
| US9066662B2 (en) | System and method for estimating cardiac pressure based on cardiac electrical conduction delays using an implantable medical device | |
| US8202224B2 (en) | System and method for calibrating cardiac pressure measurements derived from signals detected by an implantable medical device | |
| EP1341439B1 (en) | Apparatus for measurement of mean pulmonary artery pressure from a ventricle in an ambulatory monitor | |
| US7794404B1 (en) | System and method for estimating cardiac pressure using parameters derived from impedance signals detected by an implantable medical device | |
| US9113789B2 (en) | System and method for estimating electrical conduction delays from immittance values measured using an implantable medical device | |
| US7366569B2 (en) | Non-invasive method and apparatus for cardiac pacemaker pacing parameter optimization and monitoring of cardiac dysfunction | |
| US8155739B2 (en) | Cardiac resynchronization therapy optimization using mechanical dyssynchrony and shortening parameters from realtime electrode motion tracking | |
| EP1079893B1 (en) | Cardiac pacing using adjustable atrio-ventricular delays | |
| CN109475741B (en) | Electrogram-based control of cardiac resynchronization therapy | |
| US20060235480A1 (en) | Method and apparatus for automatically programming CRT devices | |
| WO2005063333A1 (en) | Adjustment of sequential biventricular pacing parameters | |
| EP1703944A1 (en) | Adjustment of sequential biventricular pacing parameters | |
| US20130226258A1 (en) | System and method for decompensation detection and treatment based on patient hemodynamics | |
| EP2429394B1 (en) | Medical device for determining a dyssynchronicity measure | |
| US11707628B2 (en) | Rate responsive pacing | |
| WO2020263966A1 (en) | Heart rate recovery assessment |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| AS | Assignment |
Owner name: OSYPKA MEDICAL GMBH, GERMANY Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNOR:OSYPKA, MARKUS;REEL/FRAME:014305/0008 Effective date: 20030708 |
|
| STCB | Information on status: application discontinuation |
Free format text: ABANDONED -- FAILURE TO RESPOND TO AN OFFICE ACTION |