EP0131740A2 - Undenatured virus-free biologically active protein derivatives - Google Patents
Undenatured virus-free biologically active protein derivatives Download PDFInfo
- Publication number
- EP0131740A2 EP0131740A2 EP84106557A EP84106557A EP0131740A2 EP 0131740 A2 EP0131740 A2 EP 0131740A2 EP 84106557 A EP84106557 A EP 84106557A EP 84106557 A EP84106557 A EP 84106557A EP 0131740 A2 EP0131740 A2 EP 0131740A2
- Authority
- EP
- European Patent Office
- Prior art keywords
- protein
- containing composition
- process according
- plasma
- factor
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Granted
Links
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2/00—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor
- A61L2/0005—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor for pharmaceuticals, biologicals or living parts
- A61L2/0011—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor for pharmaceuticals, biologicals or living parts using physical methods
- A61L2/0023—Heat
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/13—Amines
- A61K31/14—Quaternary ammonium compounds, e.g. edrophonium, choline
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K35/00—Medicinal preparations containing materials or reaction products thereof with undetermined constitution
- A61K35/12—Materials from mammals; Compositions comprising non-specified tissues or cells; Compositions comprising non-embryonic stem cells; Genetically modified cells
- A61K35/14—Blood; Artificial blood
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2/00—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor
- A61L2/0005—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor for pharmaceuticals, biologicals or living parts
- A61L2/0082—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor for pharmaceuticals, biologicals or living parts using chemical substances
- A61L2/0088—Liquid substances
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2/00—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor
- A61L2/16—Methods or apparatus for disinfecting or sterilising materials or objects other than foodstuffs or contact lenses; Accessories therefor using chemical substances
- A61L2/18—Liquid substances or solutions comprising solids or dissolved gases
-
- Y—GENERAL TAGGING OF NEW TECHNOLOGICAL DEVELOPMENTS; GENERAL TAGGING OF CROSS-SECTIONAL TECHNOLOGIES SPANNING OVER SEVERAL SECTIONS OF THE IPC; TECHNICAL SUBJECTS COVERED BY FORMER USPC CROSS-REFERENCE ART COLLECTIONS [XRACs] AND DIGESTS
- Y10—TECHNICAL SUBJECTS COVERED BY FORMER USPC
- Y10S—TECHNICAL SUBJECTS COVERED BY FORMER USPC CROSS-REFERENCE ART COLLECTIONS [XRACs] AND DIGESTS
- Y10S530/00—Chemistry: natural resins or derivatives; peptides or proteins; lignins or reaction products thereof
- Y10S530/827—Proteins from mammals or birds
- Y10S530/829—Blood
-
- Y—GENERAL TAGGING OF NEW TECHNOLOGICAL DEVELOPMENTS; GENERAL TAGGING OF CROSS-SECTIONAL TECHNOLOGIES SPANNING OVER SEVERAL SECTIONS OF THE IPC; TECHNICAL SUBJECTS COVERED BY FORMER USPC CROSS-REFERENCE ART COLLECTIONS [XRACs] AND DIGESTS
- Y10—TECHNICAL SUBJECTS COVERED BY FORMER USPC
- Y10S—TECHNICAL SUBJECTS COVERED BY FORMER USPC CROSS-REFERENCE ART COLLECTIONS [XRACs] AND DIGESTS
- Y10S530/00—Chemistry: natural resins or derivatives; peptides or proteins; lignins or reaction products thereof
- Y10S530/827—Proteins from mammals or birds
- Y10S530/829—Blood
- Y10S530/83—Plasma; serum
-
- Y—GENERAL TAGGING OF NEW TECHNOLOGICAL DEVELOPMENTS; GENERAL TAGGING OF CROSS-SECTIONAL TECHNOLOGIES SPANNING OVER SEVERAL SECTIONS OF THE IPC; TECHNICAL SUBJECTS COVERED BY FORMER USPC CROSS-REFERENCE ART COLLECTIONS [XRACs] AND DIGESTS
- Y10—TECHNICAL SUBJECTS COVERED BY FORMER USPC
- Y10S—TECHNICAL SUBJECTS COVERED BY FORMER USPC CROSS-REFERENCE ART COLLECTIONS [XRACs] AND DIGESTS
- Y10S530/00—Chemistry: natural resins or derivatives; peptides or proteins; lignins or reaction products thereof
- Y10S530/827—Proteins from mammals or birds
- Y10S530/829—Blood
- Y10S530/83—Plasma; serum
- Y10S530/831—Cohn fractions
Definitions
- This invention relates to undenatured virus-free biologically active protein-containing compositions. More especially, this invention relates to the inactivation of viruses, esspecially lipid canted viruses, e.g., hepatitis B in human blood, blood component, blood plasma or any fraction, concentrate or derivative thereof containing blood proteins or non-blood sources including normal or cancer cells, the exudate from cancer or normal cells grown in culture, hybridomas, in products from gene splicing (DNA), etc.,by the use of di- or trialkyl phosphates, and to the resultant products.
- viruses esspecially lipid canted viruses, e.g., hepatitis B in human blood, blood component, blood plasma or any fraction, concentrate or derivative thereof containing blood proteins or non-blood sources including normal or cancer cells, the exudate from cancer or normal cells grown in culture, hybridomas, in products from gene splicing (DNA), etc.,by the use of di- or trialkyl phosphates, and to the resultant products.
- this invention relates to blood plasma or other plasma protein-containing compositions which are to be rendered substantially free of hepatitis B and/or non-A and non-B hepatitis or other viral infectivity, such blood plasma or fractions thereof having valuable labile proteins, such as, for example, factor VIII.
- hepatitis B virus HBV
- HBV hepatitis B virus
- a viral inactivating agent of the type which crosslinks with the proteinaceous portion of hepatitis B virus, or which interacts with the nucleic acid of the virus.
- a viral inactivating agent of the type which crosslinks with the proteinaceous portion of hepatitis B virus, or which interacts with the nucleic acid of the virus.
- an aldehvde such as formaldehyde whereby crosslinking to the protein is effected and the hepatitis B virus is inactivated.
- BPL beta-propiolactone
- UV ultraviolet
- factor VIII one of the most labile of the valuable proteins in mammalian blood plasma. Similar protein denaturation is experienced in respect of the following other valuable plasma components: coagulation factors II, VII, IX, X; plasmin, fibrinogen (factor I) IgM, hemoglobin, interferon, etc.
- Factor VIII is denatured to a larger extent than many of the other valuable proteins present in blood plasma.
- BPL/UV inactivation procedure discussed above has not so far been adopted in the United States for numerous reasons, one of which lies in the fact that many researchers believe.that BPL is itself deleterious since it cannot be removed completely following the inactivation and thus may remain in plasma and plasma derivatives. BPL has been shown to be carcinogenic in animals and is dangerous even to personnel handling it.
- United States Patent 3,962,421 describes a method for the disruption of infectious lipid-containing viruses for preparing sub-unit vaccines by contacting the virus in an aqueous medium with a wetting agent and a trialkylphosphate.
- aqueous medium is defined as allantonic fluid, tissue culture fluid, aqueous extract or suspension of central nervous system tissue, blood cell eluate and an aqueous extract or suspension of fowl embryo.
- the patent does not describe hepatitis, nor is it concerned with preparation of blood derivatives containing labile blood protein substantially free of viral infectivity. It is only concerned with disrupting the envelope of lipid containing viruses for the production of vaccines and not with avoiding or reducing protein denaturation en route to a blood derivative.
- Non-blood sources include, but are not limited to, mammalian milk, ascitic fluid, saliva, placenta extracts, tissue culture cell lines and their extracts including transformed cells, and products of fermentation.
- sources include, but are not limited to, mammalian milk, ascitic fluid, saliva, placenta extracts, tissue culture cell lines and their extracts including transformed cells, and products of fermentation.
- the human lymphoblastoid cells have been isolated which produce alpha interferon.
- the cell line in commercial use today contains Epstein-Barr virus genes. It has been a major concern that the use of interferon produced by these cells would transmit viral infection or induce viral caused cancerous growth.
- the present invention is directed to achieving three goals, namely, (1) a safe, (2) viral inactivated protein-containing composition, (3),without incurring substantial protein denaturation.
- these three goals are not necessarily compatible since, for example, beta-propiolactone inactivates viral infectivity, but is unsafe and substances such as formaldehyde inactivate viruses, but also substantially denaturate the valuable plasma proteins, for example, factor VIII.
- a protein-containing composition such as whole blood, blood cell proteins, blood plasma, a blood plasma fractionation precipitate, a blood plasma fractionation supernatant, cryoprecipitate,,cryosupernatant, or portion or derivative thereof or serum or a non-blood product produced from normal or cancerous cells (e.g.
- hepatitis viruses via recombinant DNA technology
- a dialkylphosphateora trialkylphosphate that lipid contain ing viruses such as the hepatitis viruses present in the composition are virtually entirely inactivated without substantial denaturation of proteins therein.
- hepatitis viruses can be substantially inactivated, e.g., to an inactivation of greater than 4 logs, while realizing a yield of protein activity to total protein of at least 80%.
- a blood protein-containing composition such as mammalian whole blood, blood cell derivatives (e.g., hemoglobin, alpha-interferon, T-cell growth factor, platelet-derived growth factor, etc.), plasminogen activator, blood plasma, blood plasma fraction, blood plasma precipitate (e.g., cryoprecipitate, ethanol precipitate or polyethylene glycol precipitate), or supernatant (e.g., cryosupernatant, ethanol supernatant or polyethylene glycol supernatant), characterized by the presence of one or more blood proteins such as labile blood factor VIII having a total yield of protein activity to total protein of at least 80%, preferably at least 85%, more preferably 95% and most preferably 98% to 100%, said blood protein-containing composition having greatly reduced or virtually no hepatitis viruses.
- Virus in a serum is determined by infectivity titrations.
- the hepatitis virus is inactivated by treatment with the di- or trialkylphosphate 'described herein, and is not I inactivated because of inclusion in the plasma of antibodies which bind with the hepatitis viruses and form immune complexes
- Inactivation of virus is obtained to the extent of at least "4 logs", i.e., virus in a serum is totally inactivated to the extent determined by infectivity studies where that virus is present in the untreated serum in such a concentration that even after dilution to 10 4 , viral activity can be measured.
- Sindbis, Sendai and VSV viruses are typical lipid containing viruses and are used herein to determine the effect of di- or trialkylphosphate on lipid coated viruses generally.
- Blood is made up of solids (cells, i.e., erythrocytes, leucocytes, and thrombocytes) and liquid (plasma).
- the cells contain potentially valuable substances such as hemoglobin, and they can be induced to make other potentially valuable substances such as interferons, growth factors, and other biological response modifiers.
- the plasma is composed mainly of water, salts, lipids and proteins.
- the proteins are divided into groups called fibrinogens, serum globulins and serum albumins.
- Typical antibodies (immune globu lins) found in human blood plasma include those directed against infectious hepatitis, influenza H, etc.
- Blood transfusions are used to treat anemia resulting from disease or hemorrhage, shock resulting from loss of plasma proteins or loss of circulating volume, diseases where an adequate level of plasma protein is not maintained, for example, hemophilia, and to bestow passive immunization.
- Plasma whole blood must be carefully typed and cross matched prior to administration. Plasma, however, does not require prior testing. For certain applications, only a proper fraction of the plasma is required, such as factor VIII for treatment of hemophilia or von Willebrand's disease.
- the other components of blood may be lacking.
- the administration of the proper fraction will suffice, and the other components will not be "wasted” on the patient; the other fractions can be used for another patient.
- the separation of blood into components and their subsequent fractionation allows the pro- teins to be concentrated, thus permitting concentrates to be treated.
- the plasma fractions can be stored for much longer periods than whole blood and they can be distributed in the liquid, the frozen, or the dried state. Finally, it allows salvaging from blood banks the plasma portions of outdated whole blood that are unsafe for administration as whole blood.
- Proteins found in human plasma include prealbumin, retinol-binding protein, albumin, alpha-globulins, beta-globulins, gamma-globulins (immune serum globulins), the coagulation proteins (antithrombin III, prothrombin, plasminogen, antihemophilic factor-factor VIIII, fibrin-stabilizing factor-factor XIII, fibrinogen), immunoglobins(immunoglobulins G, A, M, D, and E). and the complement components.
- Plasma proteins There are currently more than 100 plasma proteins that have been described . A comprehensive listing can be found in "The Plasma Proteins", ed. Putnam, F.W., Academic Press, New York (1975).
- Proteins found in the blood cell fraction include hemoglobin, fibronectin, fibrinogen, enzymes of carbohydrate and protein metabolism, etc.
- the synthesis of other proteins can be induced, such as interferons and growth factors.
- Blood plasma fractionation generally involves the use of organic solvents such as ethanol, ether and polyethylene glycol at low temperatures and at controlled pH values to effect precipitation of a particular fraction con- taining one or more plasma proteins. The resultant supernatant can itself then be precipitated and so on until the desired degree of fractionation is attained. More recently, separations are based on chromatographic processes. An excellent survey of blood fractionation appears in Kirk-Othmer's Encylo- pedia of Chemical Technology, Third Edition, Interscience Publishers, Volume 4, pages 25 to 62, the entire contents of which are incorporated by reference herein.
- Fraction II and III can be further fractionated to obtain immune serum globulin (ISG).
- Another fractionation scheme involves use of frozen plasma which is thawed into a cryoprecipitate containing AHF (antihemophilic factor) and fibronectin and a cryosupernatant. The cryoprecipitate is then fractionated into fibronectin and AHF.
- AHF antihemophilic factor
- Polyethylene glycol has been used to prepare high purity AHF and non-aggregated ISG.
- hepatitis B and non-A, non-B are fibrinogen, AHF and prothrombin complex, and all other blood protein preparations except immune serum globulin and, because they are pasteurized, albumin solutions.
- Hepatitis tests presently available can indicate the presence of hepatitis B surface antigen, but there is presently no screening test for non-A, non-B hepatitis.
- the present invention is directed to contacting with di- or trialkylphosphate a blood protein-containing composition such as whole mammalian blood, blood cells thereof, blood cell proteins, blood plasma thereof, precipitate from any fractionation of such plasma, supernatant from any fractionation of such plasma, cryoprecipitate , cryosupernatant or any portions or derivatives of the above that contain blood proteins such as, for example, prothrombin complex (factors II, VII, IX and X) and cryoprecipitate (factors I and VIII).
- the present invention is also concerned with contacting di- or trialkylphosphate with a serum containing one or more blood proteins.
- the present invention is directed to contacting di- or trialkylphosphate with a blood protein-containing fraction containing at least one blood protein such as the following: factor II, factor VII, factor VIII, factor IX, factor X, fibrinogen and IgM. additionally, the present invention concerns contacting a cell lysate or proteins induced in blood cells with di- or trialkylphosphate.
- Such blood protein-containing composition is contacted with a dialkylphosphate or a trialkylphosphate having alkyl groups which contain 1 to 10 carbon atoms, especially 2 to 10 carbon atoms.
- Illustrative members of trialkylphosphates for use in the present invention include tri-(n-butyl) phosphate, tri-(t-butyl) phosphate, tri-(n-hexyl) phosphate, tri-(2-ethylhexyl) phosphate, tri-(n-decyl) phosphate, just to name a few.
- An especially preferred trialkylphosphate is tri-(n-butyl) phosphate.
- trialkylphosphates can also be employed as well as phosphates having alkyl groups of different alkyl chains, for example, ethyl, di(n-butyl) phosphate.
- dialkylphosphates can be employed including those of different alkyl group mixtures of dialkylphosphate.
- mixtures of di- and trialkyl phosphates can be employed.
- Di- or trialkylphosphates for use in the present invention are employed in an amount between about 0.01 mg/ml and about 100 mg/ml, and preferably between about 0.1 mg/ml and about 10 mg/ml.
- the di- or trialkylphosphate can be used with or without the addition of wetting agents. It is preferred, however, to use di-.or trialkylphosphate in conjunction with a wetting agent. Such wetting agent can be added either before, simultaneously with or after the di- or trialkylphosphate contacts the blood protein-containing composition. The function of the wetting agent is to enhance the contact of the virus in the blood protein-containing composition with the di- or trialkylphosphate. The wetting agent alone does not adequately inactivate the virus.
- Preferred wetting agents are non-toxic detergents.
- Contemplated nonionic detergents include those which disperse at the prevailing temperature at least 0.1% by weight of the fat in an aqueous solution containing the same when 1 gram detergent per 100 ml of solution is introduced therein.
- detergents which include polyoxyethylene derivatives of fatty acids, partial esters of sorbitol anhydrides, for example, those products known commercially as “Tween 80", “Tween 20” and polysorbate 80” and nonionic oil soluble water detergents such as that sold commercially under the trademark "Triton X 100" (oxyethylated alkylphenol).
- sodium deoxycholate as well as the "Zwitter- gents” which are synthetic zwitterionic detergents known as "sulfobetaines" such as N-dadccyl-N, N-dimetlyl-2-ammanio-1 ethane sulphonate and its congeners or nonionic detergents such as octyl-beta-D-glucopyranoside.
- Zwitter- gents synthetic zwitterionic detergents known as "sulfobetaines” such as N-dadccyl-N, N-dimetlyl-2-ammanio-1 ethane sulphonate and its congeners or nonionic detergents such as octyl-beta-D-glucopyranoside.
- Substances which might enhance the effectiveness of alkylphosphates include reducing agents such as mercaptoethanol, dithiothreitol, dithioerythritol, and dithiooctanoic acid.
- Suitable nonionic surfactants are oxyethylated alkyl phenols, polyoxyethylene sorbitan fatty acid esters, polyoxyethylene acids, polyoxyethylene alcohols, polyoxyethylene oils and polyoxyethylene oxypropylene fatty acids.
- the amount of wetting agent, if employed, is not crucial, for example, from about 0.001% to about 10%, preferably about 0.01 to 1.5%. can be used.
- Di- and trialkylphosphates may be used in conjunction with other inactivating agents such as alcohol or ethers with or without the copresence of wetting agents in accordance with copending application Serial No. 368,250 entitled “Sterilized Plzsma and Plasma Derivatives and Process Therefor", assigned to the assignee hereof.
- the ether or alcohol can be added in an amount of 1 to 50%, preferably 5 to 25% by weight, based on the volume of blood plasma, or-concentrate or other blood plasma protein-containing composition to be treated.
- ethers for inactivation use in accordance with the invention are those having the formula wherein
- R 3 is a C 1 to C 18 alkyl or alkenyl radical which can contain one or more oxygen or sulfur atoms in the chain and which can be substituted by one or more hydroxyl groups.
- Especially contemplated alcohols are those where the alkyl or allcenyl group is between 1 and 8 atoms.
- Particularly contemplated alcohols include methanal. ethanol, propanol, isopropanol, n-butanol, isobutanol, n-pentanol and the isopentanols.
- compounds such as ethylene glycol. 1.2-propylene glycol, 1,3-propane diol, 1, 4-butanediol, 2-hydroxy isobutanol (2-methy, 1,2-dihydroxypropane)
- Treatment of blood protein-containing compositions with trialkylphosphate is effected at a temperature between -5°C and 70°,preferably between 0°C and 60°C.
- the time of such treatment (contact) is for at least 1 minute, preferably at least 1 hour and generally 4 to 24 hours.
- the treatment is normally effective at atmospheric pressure, although subatmospheric and superatmospheric pressures can also be employed.
- trialkylphosphate and other inactivating agents for example, ether,are removed, although such is not necessary in all instances, depending upon the nature of the virus inactivating agents and the intended further processing of the blood plasma protein-containing composition.
- the plasma is generally subjected to a temperature of 4°C to 37°C with a slight vacuum imposed to draw off residual ether.
- Preferably means are provided to spread the plasma as a thin film to insure maximum contact and removal of the ether.
- Other methods for removal of other in activating agents include:
- Di- or trialkylphosphate can be removed as follows:
- any ether present is initially removed prior to removal of any detergent.
- the ether may be recovered for reuse by the use of suitable distillation/ condenser systems well known to the art.
- Alcohol is normally removed together with detergent. If the detergent includes both alcohol and ether, the ether is normally removed before the alcohol.
- a heating step can be effected in the presence of a protein stabilizer, e.g., an agent which stabilizes the labile protein (AHF) agalost inactivation by heat.
- the heating can be carried out using stabilizers which also tend to protect all protein, including components of the virus, against heat if the heating is carried out for a sufficient length of time, e.g., at least 5 hours and preferably at least 10 hours at a temperature of 50 - 70"C, especially 60°C.
- the virus is preferentially inactivated, nevertheless, while the protein retains a substantial amount, e.g., ⁇ 80% of its protein activity.
- the best treatment can also be carried out simultaneously with the alkyl phosphate treatment.
- the treatment of plasma or its concentrates, fractions or derivatives in accordance with the present invention can be effected using di- or trialkylphosphate immobilized on a solid substrate.
- the same can be fixed to a macro-molecular structure such as one of the type used as a backbone for ion exchange reactions, thereby permitting easy removal of the trialkylphosphate from the plasma or plasma concentrate.
- the phosphate can be insolubilized and immobilized on a solid support such as glass beads, etc., using silane or siloxane coupling agents.
- the method of the present invention permits the pooling of human blood plasma and the treatment of the pooled human blood plasma in the form of such pooled plasma. It also permits the realization of blood product derivatives such as factor VIII, gamma globulin, factor IX or the prothrombin complex (factors II , VII, IX, X), fibrinogen and any other blood derivative including HBsAg used for the preparation of HBV vaccine, all of which contain little or no residual infective hepatitis or other viruses.
- blood product derivatives such as factor VIII, gamma globulin, factor IX or the prothrombin complex (factors II , VII, IX, X), fibrinogen and any other blood derivative including HBsAg used for the preparation of HBV vaccine, all of which contain little or no residual infective hepatitis or other viruses.
- the present invention is directed, inter alia, 'to producing a blood plasma protein-containing composition such as blood, blood plasma blood plasma fractions, etc., Which is substantially free of infeetious virus, yet which contains a substantial amount of vviable (undenatured) protein. More particularly, the present invention is directed to inactivation of lipid-containing virus and preferentially inactivation of hepatitis B and non-B, non-A virus.
- viruses inactivated by the present invention include, for example, cytomegaloviruses, Epstein Barr viruses, lactic dehydrogenase viruses, herpes group viruses, rhabdoviruses, leukoviruses, myxoviruses, alphaviruses, Arboviruses (group B), paramyxoviruses, arenaviruses, and coronaviruses.
- a protein-containing composition - a product produced from normal or cancerous cells or by normal or cancerous cells e.g., via recombinant DNA technology
- mammalian blood, blood plasma, blood plasma fractions precipitates from blood fractionation and supernatants from blood fractionation having an extent of inactivation of virus greater than 4 logs of virus such as hepatitis B and non-A, non-B, and having a yield of protein activity to total protein of at least 80%, preferably at least 95% and most preferably 98% to 100%.
- composition containing factor VIII which is substantially free of hepatitis virus to the extent of having an inactivation of greater than 4 logs of the virus and a yield of protein activity to total protein of at least 80%, preferably at least 85%, more preferably at least 95% and most preferably 98% to 100%.
- the process of the present invention has been described in terms of treatment of plasma, plasma fractions, plasma concentrates or components thereof.
- the process is also useful in treating the solid components of blood, lysates or proteins secreted by cells.
- treatment of platelet concentrates, white cell (leukocyte) concentrates, and leukocyte-poor packed red cells as well as platelet rich plasma, platelet concentrates and platelet poor plasma including packed cell masses comprising the white buffy coat consisting of white blood cells above packed red cells.
- masses containing concentrates of granulocytes, monocytes, interferon, and transfer factor are also contemplated.
- virus present in products of normal or cancerous cells can be inactivated while retaining labile protein activity in such products.
- di- or trialkylphosphate treatment one can inactivate products produced using normal or cancer cells, the exudate from normal or cancerous cells, hybridomas and products produced by gene splicing.
- Such treatment docs not substantially adversely affect the desired protein.
- Cells used for production of desired protein can, of course, be mammalian as well as non-mammalian cells.
- Factor VIII and factor IX coagulant activities are assayed by determining the degree of correction in APTT time of factor VIII - and factor LX - deficient plasma, respectively. J.G. Lenahan, Phillips and Phillips, Clin. Chem., Vol. 12, page 269 (1966).
- the activity of proteins which are enzymes is determined by measuring their enzymatic activity.
- Factor IX's activity can be measured by that technique.
- Binding proteins can have their activities measured by determining their kinetics and affinity of binding to their natural substrates.
- Lymphokine activity is measured biologically in cell systems, typically by assaying their biological activity in cell cultures.
- Protein activity generally is determined by the known and standard modes for determining the activity of the protein or type of protein involved.
- AHF solutions were incubated with 0.1% TNPB plus 1% Tween 80 for 18 hours at 4°C. These solutions were initially contacted with VSV virus, Sindbis virus and Sendai virus and thereafter brought in contact with an aqueous solution containing 0.1 weight percent of tri(n-butyl) phosphate (TNBP) and 1.0 weight percent detergent (Tween 80), with the following resultant virus inactivations: 4.7 logs of vesicular stomatitis virus (VSV) , 5.8 logs of Sindbis virus, and 5.0 logs of Sendai virus. The virus was added just prior to the addition of the TNBP-Tween 80. The yield of AHF (labile protein/total protein) was found to be 86%.
- Example 1 the results of Example 1 are plotted and compared to virus inactivation with ether (20%)/Tween 80 (1%). It is seen that for VSV (Fig. 1). Sindbis (Fig. 2) and Sendai (Fig. 3), inactivation was greater (lower log titer value) for treatment according to the present invention (with TNBP) than with ether/Tween 80 treatment.
- Example 1 was repeated, but at 22°C.
- the results for Example 2 are summarized below in Table III:
Abstract
Description
- This invention relates to undenatured virus-free biologically active protein-containing compositions. More especially, this invention relates to the inactivation of viruses, esspecially lipid canted viruses, e.g., hepatitis B in human blood, blood component, blood plasma or any fraction, concentrate or derivative thereof containing blood proteins or non-blood sources including normal or cancer cells, the exudate from cancer or normal cells grown in culture, hybridomas, in products from gene splicing (DNA), etc.,by the use of di- or trialkyl phosphates, and to the resultant products. In particular, this invention relates to blood plasma or other plasma protein-containing compositions which are to be rendered substantially free of hepatitis B and/or non-A and non-B hepatitis or other viral infectivity, such blood plasma or fractions thereof having valuable labile proteins, such as, for example, factor VIII.
- Numerous attempts have been made to inactivate viruses such as hepatitis B virus (HBV) in mammalian, especially human, blood plasma. It is the practice in some countries to effect inactivation of the hepatitis B virus in the blood plasma by contacting the plasma with a viral inactivating agent of the type which crosslinks with the proteinaceous portion of hepatitis B virus, or which interacts with the nucleic acid of the virus. For instance, it is known to attempt to inactivate hepatitis B virus by contact with an aldehvde such as formaldehyde whereby crosslinking to the protein is effected and the hepatitis B virus is inactivated. It is also known to effect inactivation of the virus by contact with beta-propiolactone (BPL), an agent which acts on the nucleic acid of the virus. It is further known to use ultraviolet (UV) light, especially after a beta-propiolactone treatment.
- Unfortunately, these agents often alter, denature or destroy valuable protein components especially so-called "labile" blood coagulation factors of the plasma under conditions required for effective inactivation of,virus infectivity. For instance, in such inactivation procedures, factor VIII is inactivated or denatured to the extent of 50-90% or more of the factor VIII present in the untreated plasma. Because of the denaturing effects of these virus inactivating agents, it is necessary in the preparation of derivatives for administration to patients to concentrate large quantities of plasma so that the material to be administered to the patient once again has a sufficient concentration of'the undenatured protein for effective therapeutic treatment. This concentration, however, does not affect reduction of the amount of denatured protein. As a result, the patient not only receives the undenatured protein but a quantity of denatured protein often many times that of the undenatured protein.
- For instance, in the inactivation of hepatitis B virus in human blood plasma by beta-propiolactone, there is obtained as a result thereof, a plasma whose factor VIII has been 75% inactivated. The remaining 25% of the factor VIII is therefore present in such a small concentration, as a funecion of the plasma itself, that it is necessary to concentrate large quantities of the factor VIII to provide sufficient concentration to be of.therapeutic value. Since such separation techniques do not efficiently remove denatured factor VIII from undenatured factor VIII, the material administered to the patent may contain more denatured protein than undenatured protein. Obviously, such inactivation is valuable from a standpoint of diminishing the risk of hepatitis virus infection. However, it requires the processing of large quantities of plasma and represents significant loss of valuable protein components. Furthermore, administration of large amounts of denatured proteins may render these antigenic to the host and thus give rise to autoimmune diseases, or perhaps, rheumatoid arthritis.
- The loss of these valuable protein components is not limited to factor VIII, one of the most labile of the valuable proteins in mammalian blood plasma. Similar protein denaturation is experienced in respect of the following other valuable plasma components: coagulation factors II, VII, IX, X; plasmin, fibrinogen (factor I) IgM, hemoglobin, interferon, etc.
- Factor VIII, however, is denatured to a larger extent than many of the other valuable proteins present in blood plasma.
- As a result of the foregoing, except in the processing of serum albumin, a stable plasma protein solution which can withstand pasteurization, it is largely the practice in the United States in respect of the processing of blood proteins to take no step in respect of the sterilization for inactivation of viruses. As a result, recipients of factor VIII. gamma-globulin, factor IX, fibrinogen, etc., must accept the risk that the valuable protein components being administered may be contaminated with hepatitis viruses as well as other infectious viruses. As a result, these recipients face the danger of becoming infected by these viruses and having to endure the damage which the virus causes to the liver and other organ systems and consequent incapacitation and illness, which may lead to death.
- The BPL/UV inactivation procedure discussed above has not so far been adopted in the United States for numerous reasons, one of which lies in the fact that many researchers believe.that BPL is itself deleterious since it cannot be removed completely following the inactivation and thus may remain in plasma and plasma derivatives. BPL has been shown to be carcinogenic in animals and is dangerous even to personnel handling it.
- Other methods for the inactivation of hepatitis B virus in the plasma are known, but are usually impractical. One method involves the addition of antibodies to the plasma whereby an immune complex is formed. The expense of antibody formation and purification add significantly to the cost of the plasma production; furthermore, there is no assurance that a sufficient quantity of hepatitis B or non-A, non-B virus is inactivated. There is currently no test for non-A, non-B antibodies (although there is a test for the virus); hence, it is not possible to select plasma containing high titers of anti non-A, non-B antibody.
- It is to be understood that the problems of inactivation of the viruses in plasma are distinct from the problems of inactivation of the viruses themselves due to the copresence of the desirable proteinaceous components of the plasma. Thus, while it is known how to inactivate the hepatitis B virus, crosslinking agents, for example, glutaraldehyde, nucleic acid reacting chemicals, for example BPL or formaldehyde, or oxidizing agents, for example chlorox, etc., it has been believed that these methods are not suitable for the inactivation of the virus in plasma due to the observation that most of these activating agents (sodium hypochlorite, formaldehyde, beta-propiolactone) denatured the valuable proteinaceous components of the plasma.
- United States Patent 4,315,919 to Shanbrom de- scribes a method of depyrogenating a proteinaceous biological or pharmaceutical product by contacting such proteinaceous product with a non-denaturing amphiphile.
- United States Patent 4,314,997 to Shanbrom describes a method of reducing pyrogenicity, hepatitis infectivity and clotting activation of a plasma protein product by contacting the product with a non-denatured amphiphile.
- Both Shanbrom '919 and '997 contemplate the use of a non-ionic detergent, for example, "Tween 80" as the amphiphile. It will be shown hereinafter that treatment with "Tween 80" by itself is relatively ineffective as a viral inactivating agent.
- United States Patent 3,962,421 describes a method for the disruption of infectious lipid-containing viruses for preparing sub-unit vaccines by contacting the virus in an aqueous medium with a wetting agent and a trialkylphosphate. Such aqueous medium is defined as allantonic fluid, tissue culture fluid, aqueous extract or suspension of central nervous system tissue, blood cell eluate and an aqueous extract or suspension of fowl embryo. The patent does not describe hepatitis, nor is it concerned with preparation of blood derivatives containing labile blood protein substantially free of viral infectivity. It is only concerned with disrupting the envelope of lipid containing viruses for the production of vaccines and not with avoiding or reducing protein denaturation en route to a blood derivative.
- Problems may also exist in deriving valuable proteins from non-blood sources. These sources include, but are not limited to, mammalian milk, ascitic fluid, saliva, placenta extracts, tissue culture cell lines and their extracts including transformed cells, and products of fermentation. For in- stance, the human lymphoblastoid cells have been isolated which produce alpha interferon. However, the cell line in commercial use today contains Epstein-Barr virus genes. It has been a major concern that the use of interferon produced by these cells would transmit viral infection or induce viral caused cancerous growth.
- The present invention is directed to achieving three goals, namely, (1) a safe, (2) viral inactivated protein-containing composition, (3),without incurring substantial protein denaturation. As shown above, these three goals are not necessarily compatible since, for example, beta-propiolactone inactivates viral infectivity, but is unsafe and substances such as formaldehyde inactivate viruses, but also substantially denaturate the valuable plasma proteins, for example, factor VIII.
- It, therefore, became desirable to provide a process for obtaining protein-containing compositions which does not substantially denature the valuable protein components therein and which does not entail the use of a proven carcinogenic agent. More especiall, it is desirable to provide blood) protein-containing compositions in which substantially all of the hepatitis viruses and other viruses present are inactivated and in which denatured protein such as factor VIII account for only a small amount of the total amount of these proteins in the blood protein-containing composition.
- It is a further object to provide products.from cancer or normal cells or from fermentation processes following gene insertion which are substantially free of virus, especially lipid-containing viruses
- . It has now been discovered, quite surprisingly, that while most of the viral inactivating agents denature factor VIII and other valuable blood plasma proteins, that not all viral inactivating agents have such effect. It has been discovered that a protein-containing composition such as whole blood, blood cell proteins, blood plasma, a blood plasma fractionation precipitate, a blood plasma fractionation supernatant, cryoprecipitate,,cryosupernatant, or portion or derivative thereof or serum or a non-blood product produced from normal or cancerous cells (e.g. via recombinant DNA technology) is contacted for a sufficient period of time with a dialkylphosphateora trialkylphosphate that lipid contain ing viruses such as the hepatitis viruses present in the composition are virtually entirely inactivated without substantial denaturation of proteins therein. By contacting blood protein mixture or concentrate thereof or fraction thereof with a di or trialkylphosphate, followed by removal of the di- or trialkylphosphate, hepatitis viruses can be substantially inactivated, e.g., to an inactivation of greater than 4 logs, while realizing a yield of protein activity to total protein of at least 80%.
- By such procedures there is provided a blood protein-containing composition such as mammalian whole blood, blood cell derivatives (e.g., hemoglobin, alpha-interferon, T-cell growth factor, platelet-derived growth factor, etc.), plasminogen activator, blood plasma, blood plasma fraction, blood plasma precipitate (e.g., cryoprecipitate, ethanol precipitate or polyethylene glycol precipitate), or supernatant (e.g., cryosupernatant, ethanol supernatant or polyethylene glycol supernatant), characterized by the presence of one or more blood proteins such as labile blood factor VIII having a total yield of protein activity to total protein of at least 80%, preferably at least 85%, more preferably 95% and most preferably 98% to 100%, said blood protein-containing composition having greatly reduced or virtually no hepatitis viruses. Virus in a serum is determined by infectivity titrations.
- By the inactivation procedure of the invention, most if not virtually all of the hepatitis viruses contained therein would be inactivated. The method for determining infectivity levels by in vivo chimpanzees is discussed by Prince, A.M., Stephen, W., Brotman, B. and van den Ende, M.C., "Evaluation of the Effect of Beta-propiolactone/Ultraviolet Irradiation (BPL/UV) Treatment of Source Plasma on Hepatitis Transmission by factor IV Complex in Chimpanzees, Thrombosis and Haemostasis", 44: 138-142, 1980.
- The hepatitis virus is inactivated by treatment with the di- or trialkylphosphate 'described herein, and is not I inactivated because of inclusion in the plasma of antibodies which bind with the hepatitis viruses and form immune complexes
- Inactivation of virus is obtained to the extent of at least "4 logs", i.e., virus in a serum is totally inactivated to the extent determined by infectivity studies where that virus is present in the untreated serum in such a concentration that even after dilution to 104, viral activity can be measured.
-
- Fig. 1 shows virus inactivation as a function of log titer value versus time for VSV virus (vesicular stomatitis virus) treated according to the present invention and treated with ether/
Tween 80. The lower log titer for treatment according to the present invention indicates greater virus inactivation; - Fig. 2 shows virus inactivation as a function of log titer value versus time for Sindbis virus treated according to the present invention and treated with ether/
Tween 80; - Fig. 3 shows virus inactivation as a function of log titer value versus time for Sendai virus treated according to the present invention and treated with ether/
Tween 80; - Fig. 4 shows virus inactivation as a function of log titer value versus time for EMC virus (a non-lipid coated virus) treated according to the present invention and treated with ether/
Tween 80; - Fig. 5 is a plot of log titer value versus hours for VSV virus for TNBP/
Tween 80 at 0°C and at room temperature and TNBP alone (at room temperature); - Fig. 6 is a plot of log titer value versus hours for-Sindbis virus for TNBP/
Tween 80 at 0°C and at room temperature and TNBP alone (at room temperature); - Fig. 7 is a plot of log titer value versus hours for Sendai virus for TNBP /
Tween 80 at 0°C and at room temperature and TNBP alone (at room temperature); and - Fig. 8 is a plot of log titer value versus hours for EMC virus for TNBP/
Tween 80 at 0°C and at room temperature and TNBP alone (at room temperature). - The Sindbis, Sendai and VSV viruses are typical lipid containing viruses and are used herein to determine the effect of di- or trialkylphosphate on lipid coated viruses generally.
- Blood is made up of solids (cells, i.e., erythrocytes, leucocytes, and thrombocytes) and liquid (plasma). The cells contain potentially valuable substances such as hemoglobin, and they can be induced to make other potentially valuable substances such as interferons, growth factors, and other biological response modifiers. The plasma is composed mainly of water, salts, lipids and proteins. The proteins are divided into groups called fibrinogens, serum globulins and serum albumins. Typical antibodies (immune globu lins) found in human blood plasma include those directed against infectious hepatitis, influenza H, etc.
- Blood transfusions are used to treat anemia resulting from disease or hemorrhage, shock resulting from loss of plasma proteins or loss of circulating volume, diseases where an adequate level of plasma protein is not maintained, for example, hemophilia, and to bestow passive immunization.
- Whole blood must be carefully typed and cross matched prior to administration. Plasma, however, does not require prior testing. For certain applications, only a proper fraction of the plasma is required, such as factor VIII for treatment of hemophilia or von Willebrand's disease.
- With certain diseases one or several of the components of blood may be lacking. Thus the administration of the proper fraction will suffice, and the other components will not be "wasted" on the patient; the other fractions can be used for another patient. The separation of blood into components and their subsequent fractionation allows the pro- teins to be concentrated, thus permitting concentrates to be treated. Of great importance, too, is the fact that the plasma fractions can be stored for much longer periods than whole blood and they can be distributed in the liquid, the frozen, or the dried state. Finally, it allows salvaging from blood banks the plasma portions of outdated whole blood that are unsafe for administration as whole blood.
- Proteins found in human plasma include prealbumin, retinol-binding protein, albumin, alpha-globulins, beta-globulins, gamma-globulins (immune serum globulins), the coagulation proteins (antithrombin III, prothrombin, plasminogen, antihemophilic factor-factor VIIII, fibrin-stabilizing factor-factor XIII, fibrinogen), immunoglobins(immunoglobulins G, A, M, D, and E). and the complement components. There are currently more than 100 plasma proteins that have been described . A comprehensive listing can be found in "The Plasma Proteins", ed. Putnam, F.W., Academic Press, New York (1975).
- Proteins found in the blood cell fraction include hemoglobin, fibronectin, fibrinogen, enzymes of carbohydrate and protein metabolism, etc. In addition, the synthesis of other proteins can be induced, such as interferons and growth factors.
- A comprehensive list of inducible leukocyte proteins can be found in Stanley Cohen, Edgar Pick, J.J. Oppen- heim, "Biology of the Lymphokines", Academic Press, N.Y. (1979).
- Blood plasma fractionation generally involves the use of organic solvents such as ethanol, ether and polyethylene glycol at low temperatures and at controlled pH values to effect precipitation of a particular fraction con- taining one or more plasma proteins. The resultant supernatant can itself then be precipitated and so on until the desired degree of fractionation is attained. More recently, separations are based on chromatographic processes. An excellent survey of blood fractionation appears in Kirk-Othmer's Encylo- pedia of Chemical Technology, Third Edition, Interscience Publishers,
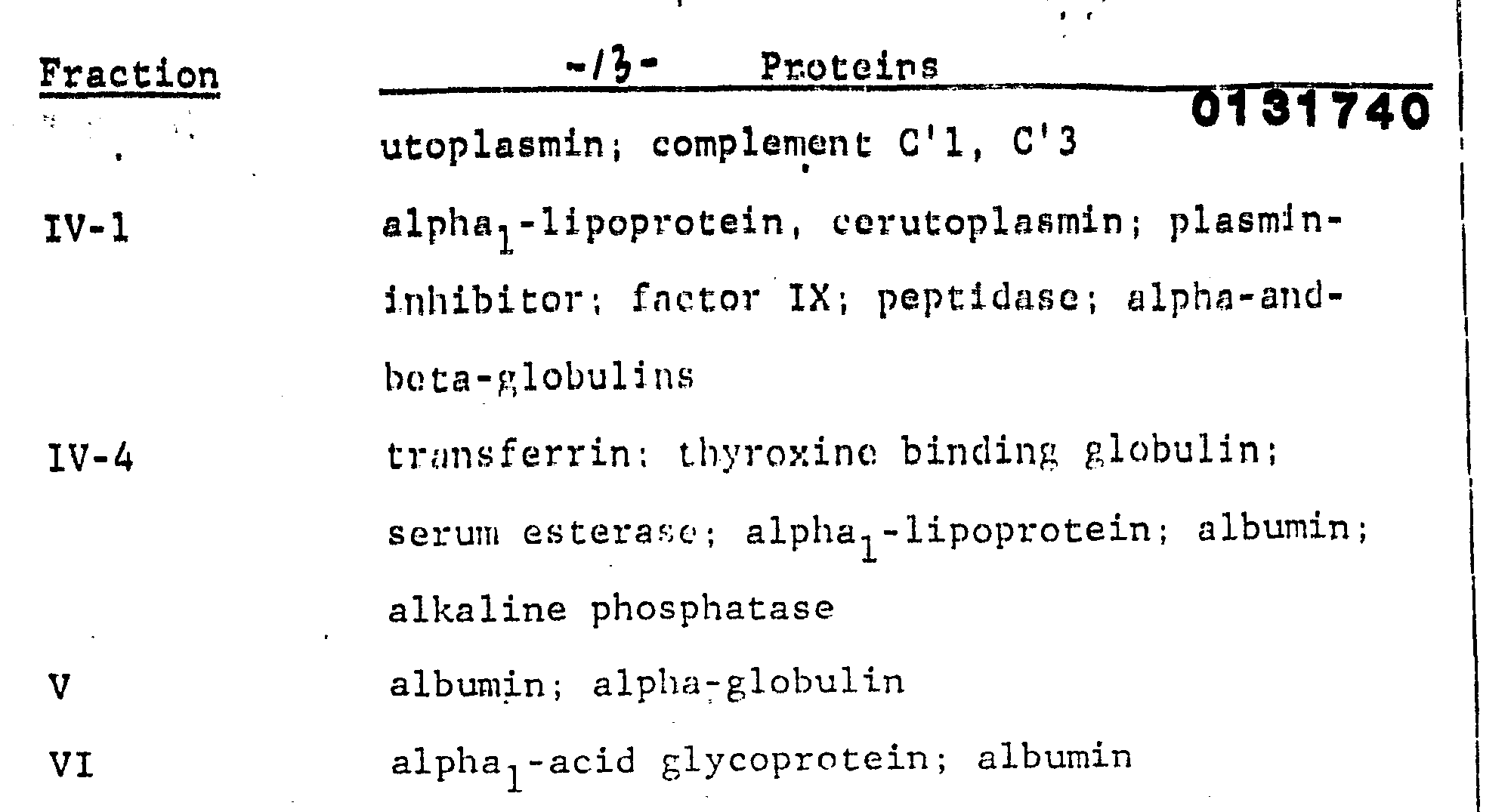
Volume 4, pages 25 to 62, the entire contents of which are incorporated by reference herein. - The major components of a cold ethanol fractionation are as follows:
-
- I fibrinogen; cold insoluble globulin;factor VIII;properdin
- II and III IgG; IgM: IgA; fibrinogen;beta-lipoprotein; prothrombin; plasminogen; plasmin inhibitor; factor V; factor VII; factor IX; factor X; thrombin; antithrombin: isoagglutinins; cer-
- The above fractionation scheme can serve as a basis for further fractionations. Fraction II and III, for example, can be further fractionated to obtain immune serum globulin (ISG).
- Another fractionation scheme involves use of frozen plasma which is thawed into a cryoprecipitate containing AHF (antihemophilic factor) and fibronectin and a cryosupernatant. The cryoprecipitate is then fractionated into fibronectin and AHF.
- Polyethylene glycol has been used to prepare high purity AHF and non-aggregated ISG.
- High risk products with respect to the transmission of hepatitis B and non-A, non-B are fibrinogen, AHF and prothrombin complex, and all other blood protein preparations except immune serum globulin and, because they are pasteurized, albumin solutions. Hepatitis tests presently available can indicate the presence of hepatitis B surface antigen, but there is presently no screening test for non-A, non-B hepatitis.
- The present invention is directed to contacting with di- or trialkylphosphate a blood protein-containing composition such as whole mammalian blood, blood cells thereof, blood cell proteins, blood plasma thereof, precipitate from any fractionation of such plasma, supernatant from any fractionation of such plasma, cryoprecipitate , cryosupernatant or any portions or derivatives of the above that contain blood proteins such as, for example, prothrombin complex (factors II, VII, IX and X) and cryoprecipitate (factors I and VIII). The present invention is also concerned with contacting di- or trialkylphosphate with a serum containing one or more blood proteins. Furthermore, the present invention is directed to contacting di- or trialkylphosphate with a blood protein-containing fraction containing at least one blood protein such as the following: factor II, factor VII, factor VIII, factor IX, factor X, fibrinogen and IgM. additionally, the present invention concerns contacting a cell lysate or proteins induced in blood cells with di- or trialkylphosphate.
- Such blood protein-containing composition is contacted with a dialkylphosphate or a trialkylphosphate having alkyl groups which contain 1 to 10 carbon atoms, especially 2 to 10 carbon atoms. Illustrative members of trialkylphosphates for use in the present invention include tri-(n-butyl) phosphate, tri-(t-butyl) phosphate, tri-(n-hexyl) phosphate, tri-(2-ethylhexyl) phosphate, tri-(n-decyl) phosphate, just to name a few. An especially preferred trialkylphosphate is tri-(n-butyl) phosphate. Mixtures of different trialkylphosphates can also be employed as well as phosphates having alkyl groups of different alkyl chains, for example, ethyl, di(n-butyl) phosphate. Similarly, the respective dialkylphosphates can be employed including those of different alkyl group mixtures of dialkylphosphate. Furthermore, mixtures of di- and trialkyl phosphates can be employed.
- Di- or trialkylphosphates for use in the present invention are employed in an amount between about 0.01 mg/ml and about 100 mg/ml, and preferably between about 0.1 mg/ml and about 10 mg/ml.
- The di- or trialkylphosphate can be used with or without the addition of wetting agents. It is preferred, however, to use di-.or trialkylphosphate in conjunction with a wetting agent. Such wetting agent can be added either before, simultaneously with or after the di- or trialkylphosphate contacts the blood protein-containing composition. The function of the wetting agent is to enhance the contact of the virus in the blood protein-containing composition with the di- or trialkylphosphate. The wetting agent alone does not adequately inactivate the virus.
- Preferred wetting agents are non-toxic detergents. Contemplated nonionic detergents include those which disperse at the prevailing temperature at least 0.1% by weight of the fat in an aqueous solution containing the same when 1 gram detergent per 100 ml of solution is introduced therein. In particular there is contemplated detergents which include polyoxyethylene derivatives of fatty acids, partial esters of sorbitol anhydrides, for example, those products known commercially as "
Tween 80", "Tween 20" andpolysorbate 80" and nonionic oil soluble water detergents such as that sold commercially under the trademark "Triton X 100" (oxyethylated alkylphenol). Also contemplated is sodium deoxycholate as well as the "Zwitter- gents" which are synthetic zwitterionic detergents known as "sulfobetaines" such as N-dadccyl-N, N-dimetlyl-2-ammanio-1 ethane sulphonate and its congeners or nonionic detergents such as octyl-beta-D-glucopyranoside. - Substances which might enhance the effectiveness of alkylphosphates include reducing agents such as mercaptoethanol, dithiothreitol, dithioerythritol, and dithiooctanoic acid. Suitable nonionic surfactants are oxyethylated alkyl phenols, polyoxyethylene sorbitan fatty acid esters, polyoxyethylene acids, polyoxyethylene alcohols, polyoxyethylene oils and polyoxyethylene oxypropylene fatty acids. Some spe- cific examples are the following:
- alkylphenoxypolyethoxy (30) ethanol
- polyoxyethylene(2) sorbitan monolaurate
- polyoxyethylene (20) sorbitan monopalmitate
- polyoxyethylene (20) sorbitan monostearate
- polyoxyethylene (20) sorbitan tristearate
- polyoxyethylene (20) sorbitan monooleate
- polyoxyethylene (20) sorbitan trioleate
- polyoxyethylene (20) palmitate
- polyoxyethylene (20) lauryl ether
- polyoxyethylene (20)cetyl ether
- polyoxyethylene (20) stearyl ether
- polyoxyethylene (20) oleyl ether
- polyoxyethylene (25) hydrogenated castor oil
- polyoxyethylene (25) oxypropylene monostearate
- The amount of wetting agent, if employed, is not crucial, for example, from about 0.001% to about 10%, preferably about 0.01 to 1.5%. can be used.
- Di- and trialkylphosphates may be used in conjunction with other inactivating agents such as alcohol or ethers with or without the copresence of wetting agents in accordance with copending application Serial No. 368,250 entitled "Sterilized Plzsma and Plasma Derivatives and Process Therefor", assigned to the assignee hereof.
- The ether or alcohol can be added in an amount of 1 to 50%, preferably 5 to 25% by weight, based on the volume of blood plasma, or-concentrate or other blood plasma protein-containing composition to be treated.
-
- R1 and R2 are independently C1-C18 alkyl or alkenyl which can contain an 0 or S atom in the chain, preferably C1-C8 alkyl or alkenyl. Especially contemplated ; ethers are dimethyl ether, diethyl ether, ethyl propyl ether, methyl-butyl ether, methyl isopropyl ether and methyl isobutyl ether.
-
- R3 is a C1 to C18 alkyl or alkenyl radical which can contain one or more oxygen or sulfur atoms in the chain and which can be substituted by one or more hydroxyl groups.
- Especially contemplated alcohols are those where the alkyl or allcenyl group is between 1 and 8 atoms. Particularly contemplated alcohols include methanal. ethanol, propanol, isopropanol, n-butanol, isobutanol, n-pentanol and the isopentanols. Also contemplated are compounds such as ethylene glycol. 1.2-propylene glycol, 1,3-propane diol, 1, 4-butanediol, 2-hydroxy isobutanol (2-methy, 1,2-dihydroxypropane)
- Treatment of blood protein-containing compositions with trialkylphosphate is effected at a temperature between -5°C and 70°,preferably between 0°C and 60°C. The time of such treatment (contact) is for at least 1 minute, preferably at least 1 hour and generally 4 to 24 hours. The treatment is normally effective at atmospheric pressure, although subatmospheric and superatmospheric pressures can also be employed.
- Normally, after the treatment, the trialkylphosphate and other inactivating agents, for example, ether,are removed, although such is not necessary in all instances, depending upon the nature of the virus inactivating agents and the intended further processing of the blood plasma protein-containing composition.
- To remove ether from plasma the plasma is generally subjected to a temperature of 4°C to 37°C with a slight vacuum imposed to draw off residual ether. Preferably means are provided to spread the plasma as a thin film to insure maximum contact and removal of the ether. Other methods for removal of other in activating agents include:
- (1) bubbling of nitrogen gas;
- (2) diafiltration using ether insoluble, e.g. "TEFLON", microporous membranes which retain the plasma proteins;
- (3) absorption of desired plasma components on chromatographic or affinity chromographic supports;
- (4) precipitation. for example, by salting out of plasma proteins;
- (5) lyophilization, etc.
- When alcohol or nonionic detergents are employed with the trialkylphosphate they are removed by (2) to (5) above.
- above. Di- or trialkylphosphate can be removed as follows:
- (a) Removal from AHF can be effected by precipitation of AHF with 2.2 molal glycine and 2.0 M sodium chloride
- (b) Removal from fibronectin can be effected by binding the fibronectin on a column of insolubilized gelatin and washing the bound fibronectin free of reagent.
- Generally speaking, any ether present is initially removed prior to removal of any detergent. The ether may be recovered for reuse by the use of suitable distillation/ condenser systems well known to the art.
- Alcohol is normally removed together with detergent. If the detergent includes both alcohol and ether, the ether is normally removed before the alcohol.
- The process of the invention can be combined with still other modes of inactivatins, viruses including those for non-lipid coated viruses. for instance, a heating step can be effected in the presence of a protein stabilizer, e.g., an agent which stabilizes the labile protein (AHF) agalost inactivation by heat. Moreover, the heating can be carried out using stabilizers which also tend to protect all protein, including components of the virus, against heat if the heating is carried out for a sufficient length of time, e.g., at least 5 hours and preferably at least 10 hours at a temperature of 50 - 70"C, especially 60°C. By such mode the virus is preferentially inactivated, nevertheless, while the protein retains a substantial amount, e.g.,≥80% of its protein activity. Of course, the best treatment can also be carried out simultaneously with the alkyl phosphate treatment.
- The treatment of plasma or its concentrates, fractions or derivatives in accordance with the present invention can be effected using di- or trialkylphosphate immobilized on a solid substrate. The same can be fixed to a macro-molecular structure such as one of the type used as a backbone for ion exchange reactions, thereby permitting easy removal of the trialkylphosphate from the plasma or plasma concentrate. Alternatively the phosphate can be insolubilized and immobilized on a solid support such as glass beads, etc., using silane or siloxane coupling agents.
- The method of the present invention permits the pooling of human blood plasma and the treatment of the pooled human blood plasma in the form of such pooled plasma. It also permits the realization of blood product derivatives such as factor VIII, gamma globulin, factor IX or the prothrombin complex (factors II , VII, IX, X), fibrinogen and any other blood derivative including HBsAg used for the preparation of HBV vaccine, all of which contain little or no residual infective hepatitis or other viruses.
- The present invention, is directed, inter alia, 'to producing a blood plasma protein-containing composition such as blood, blood plasma blood plasma fractions, etc., Which is substantially free of infeetious virus, yet which contains a substantial amount of vviable (undenatured) protein. More particularly, the present invention is directed to inactivation of lipid-containing virus and preferentially inactivation of hepatitis B and non-B, non-A virus. Other viruses inactivated by the present invention.include, for example, cytomegaloviruses, Epstein Barr viruses, lactic dehydrogenase viruses, herpes group viruses, rhabdoviruses, leukoviruses, myxoviruses, alphaviruses, Arboviruses (group B), paramyxoviruses, arenaviruses, and coronaviruses.
- According to the present invention, there is contemplated a protein-containing composition - a product produced from normal or cancerous cells or by normal or cancerous cells (e.g., via recombinant DNA technology), such as mammalian blood, blood plasma, blood plasma fractions, precipitates from blood fractionation and supernatants from blood fractionation having an extent of inactivation of virus greater than 4 logs of virus such as hepatitis B and non-A, non-B, and having a yield of protein activity to total protein of at least 80%, preferably at least 95% and most preferably 98% to 100%.
- Further contemplated by the present invention is a composition containing factor VIII which is substantially free of hepatitis virus to the extent of having an inactivation of greater than 4 logs of the virus and a yield of protein activity to total protein of at least 80%, preferably at least 85%, more preferably at least 95% and most preferably 98% to 100%.
- The process of the present invention has been described in terms of treatment of plasma, plasma fractions, plasma concentrates or components thereof. The process, however, is also useful in treating the solid components of blood, lysates or proteins secreted by cells. Thus, also contemplated are treatment of platelet concentrates, white cell (leukocyte) concentrates, and leukocyte-poor packed red cells as well as platelet rich plasma, platelet concentrates and platelet poor plasma including packed cell masses comprising the white buffy coat consisting of white blood cells above packed red cells. Also contemplated is the treatment of masses containing concentrates of granulocytes, monocytes, interferon, and transfer factor.
- One can treat plasma itself according to the present invention or fresh frozen plasma, thawed frozen plasma, cryoprecipitate. cryosupernatants or concentrates from frozen plasma as well as dilution products thereof.
- By the same manipulative steps discussed above, virus present in products of normal or cancerous cells can be inactivated while retaining labile protein activity in such products. For instance, by the same di- or trialkylphosphate treatment one can inactivate products produced using normal or cancer cells, the exudate from normal or cancerous cells, hybridomas and products produced by gene splicing. Such treatment docs not substantially adversely affect the desired protein. Cells used for production of desired protein can, of course, be mammalian as well as non-mammalian cells.
- Factor VIII and factor IX coagulant activities are assayed by determining the degree of correction in APTT time of factor VIII - and factor LX - deficient plasma, respectively. J.G. Lenahan, Phillips and Phillips, Clin. Chem., Vol. 12, page 269 (1966).
- The activity of proteins which are enzymes is determined by measuring their enzymatic activity. Factor IX's activity can be measured by that technique.
- Binding proteins can have their activities measured by determining their kinetics and affinity of binding to their natural substrates.
- Lymphokine activity is measured biologically in cell systems, typically by assaying their biological activity in cell cultures.
- Protein activity generally is determined by the known and standard modes for determining the activity of the protein or type of protein involved.
- In order to more fully illustrate the nature of the invention and the manner of practicing the same, the following non-limiting examples are presented:
- AHF solutions were incubated with 0.1% TNPB plus 1
% Tween 80 for 18 hours at 4°C. These solutions were initially contacted with VSV virus, Sindbis virus and Sendai virus and thereafter brought in contact with an aqueous solution containing 0.1 weight percent of tri(n-butyl) phosphate (TNBP) and 1.0 weight percent detergent (Tween 80), with the following resultant virus inactivations: 4.7 logs of vesicular stomatitis virus (VSV) , 5.8 logs of Sindbis virus, and 5.0 logs of Sendai virus. The virus was added just prior to the addition of the TNBP-Tween 80. The yield of AHF (labile protein/total protein) was found to be 86%. - Controls in which TNBP and
Tween 80 were omite showed little if any viral inactivation, -
- In Fig. 1, Fig. 2, and Fig. 3, the results of Example 1 are plotted and compared to virus inactivation with ether (20%)/Tween 80 (1%). It is seen that for VSV (Fig. 1). Sindbis (Fig. 2) and Sendai (Fig. 3), inactivation was greater (lower log titer value) for treatment according to the present invention (with TNBP) than with ether/
Tween 80 treatment. -
-
- The present invention may be embodied in other specific forms'without departing from the spirit or essential attributes thereof and, accordingly, reference should be had to the appended claims, rather than to the foregoing specification, as indicating the scope of the invention.
Claims (34)
Priority Applications (1)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| AT84106557T ATE57836T1 (en) | 1983-07-14 | 1984-06-08 | NON-DENATURED VIRUS-FREE BIOLOGICALLY ACTIVE PROTEIN DERIVATIVES. |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US06/514,375 US4540573A (en) | 1983-07-14 | 1983-07-14 | Undenatured virus-free biologically active protein derivatives |
| US514375 | 1983-07-14 |
Publications (4)
| Publication Number | Publication Date |
|---|---|
| EP0131740A2 true EP0131740A2 (en) | 1985-01-23 |
| EP0131740A3 EP0131740A3 (en) | 1985-08-07 |
| EP0131740B1 EP0131740B1 (en) | 1990-10-31 |
| EP0131740B2 EP0131740B2 (en) | 1994-09-28 |
Family
ID=24046877
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP84106557A Expired - Lifetime EP0131740B2 (en) | 1983-07-14 | 1984-06-08 | Undenatured virus-free biologically active protein derivatives |
Country Status (8)
| Country | Link |
|---|---|
| US (1) | US4540573A (en) |
| EP (1) | EP0131740B2 (en) |
| JP (1) | JPH06102627B2 (en) |
| AT (1) | ATE57836T1 (en) |
| AU (1) | AU563925B2 (en) |
| CA (1) | CA1221910A (en) |
| DE (1) | DE3483499D1 (en) |
| ZA (1) | ZA844596B (en) |
Cited By (44)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| EP0367840A1 (en) | 1988-11-05 | 1990-05-16 | Octapharma AG | Process for producing by chromatography a non-infectious antihemophilic factor with high purity |
| DE4001099A1 (en) * | 1990-01-17 | 1991-07-18 | Octapharma Ag | METHOD FOR REMOVING VIRUSES FROM BIOLOGICAL LIQUIDS |
| DE4001098A1 (en) * | 1990-01-17 | 1991-07-18 | Octapharma Ag | SUPPORTED DIALKOXYPHOSPHORIC COMPOUNDS, METHOD FOR THEIR PRODUCTION AND THEIR USE |
| DE4008852A1 (en) * | 1990-03-20 | 1991-09-26 | Octapharma Ag | METHOD FOR PRODUCING NON-INFECTIOUS BLOOD PLASMA |
| DE4142908A1 (en) * | 1991-12-24 | 1993-07-01 | Octapharma Ag | METHOD FOR PRODUCING A VIRUS-INACTIVATED PROTHROMINE COMPLEX CONCENTRATE (PPSB) |
| DE4318435A1 (en) * | 1993-02-09 | 1994-08-11 | Octapharma Ag | Method for inactivating viruses that are not provided with lipid envelopes |
| WO1994017834A1 (en) * | 1993-02-09 | 1994-08-18 | Octapharma Ag | Method for inactivating viruses devoid of lipid envelopes |
| US5410022A (en) * | 1992-04-24 | 1995-04-25 | Immuno Aktiengesellschaft | Method of producing a factor VIII preparation |
| EP0651054A1 (en) * | 1993-08-02 | 1995-05-03 | IMMUNO Aktiengesellschaft | Virus-inactivated factor Xa preparation |
| WO1995016030A1 (en) * | 1993-12-10 | 1995-06-15 | Octapharma Ag | Purification of vitamin-k dependent proteins by membrane chromatography |
| LT3333B (en) | 1988-06-07 | 1995-07-25 | Centre Regional De Transfusion | Chromatographic separation of plasma protein and concentrates obtained by this method |
| EP0692491A1 (en) | 1994-07-14 | 1996-01-17 | IMMUNO Aktiengesellschaft | Human virus-free monomeric immunoglobulin A and method for its production |
| WO1996002571A1 (en) * | 1994-07-14 | 1996-02-01 | Croix-Rouge De Belgique | Concentrate of fibrinogene obtained from blood plasma, process and plant for its preparation |
| WO1996027003A1 (en) | 1995-02-25 | 1996-09-06 | Octapharma Ag | A process for the preparation of factor ix from biological sources |
| WO1996035710A1 (en) * | 1995-05-08 | 1996-11-14 | Suomen Punainen Risti Veripalvelu | Preparation of immunoglobulin |
| DE19528221A1 (en) * | 1995-08-01 | 1997-02-06 | Blutspendedienst Der Drk Lande | Double virus-inactivated human blood plasma, blood plasma derivatives that can be produced therefrom and methods for their production |
| US5614493A (en) * | 1993-06-18 | 1997-03-25 | Immuno Ag | Use of human protein C for prevention and treatment of depositions of thrombocytes |
| US5614405A (en) * | 1991-06-20 | 1997-03-25 | Immuno Aktiengesellschaft | Method of determining the virus inactivation capacity of an inactivation treatment |
| US5639730A (en) * | 1992-12-16 | 1997-06-17 | Immuno Aktiengesellschaft | Method of producing a virus-safe biological preparation |
| AT405608B (en) * | 1997-04-08 | 1999-10-25 | Immuno Ag | METHOD FOR INACTIVATING PATHOGENS, ESPECIALLY VIRUSES, IN A BIOLOGICAL MATERIAL |
| US6068838A (en) * | 1996-04-29 | 2000-05-30 | Baxter Aktiengesellschaft | Purified multimerase |
| EP0934072A4 (en) * | 1996-06-26 | 2000-09-20 | Alpha Therapeutic Corp | Manufacturing process for the production of purified transferrin |
| US6649339B1 (en) | 1999-08-20 | 2003-11-18 | Baxter Aktiengesellschaft | Method for producing a quality assured biological sample and composition containing the same |
| WO2005054275A3 (en) * | 2003-12-01 | 2005-09-09 | Novo Nordisk Healthcare Ag | Nanofiltration of factor vii solutions to remove virus |
| US7005502B1 (en) | 1997-05-28 | 2006-02-28 | Baxter Aktiengesellschaft | Pharmaceutical preparation comprising vWF propeptide |
| US7091015B1 (en) | 1997-08-28 | 2006-08-15 | Baxter Aktiengesellschaft | Fibrinogen-based tissue adhesive |
| US7241603B2 (en) | 1999-02-12 | 2007-07-10 | Baxter Aktiengesellschaft | Method for producing a preparation based on fibrinogen and fibronectin as well as protein compositions obtainable according to this method |
| EP2277915A1 (en) | 2004-02-27 | 2011-01-26 | Octapharma AG | A purified, virus safe antibody preparation |
| WO2011061705A1 (en) | 2009-11-18 | 2011-05-26 | Lfb Biomedicaments | Method for treating blood plasma including a step of washing by means of dispersion |
| WO2011121020A1 (en) | 2010-03-30 | 2011-10-06 | Octapharma Ag | A process for purifying vitamin k dependent proteins such as coagulation factor ix |
| WO2011121031A1 (en) | 2010-03-30 | 2011-10-06 | Octapharma Ag | Process for the purification of a growth factor protein |
| US8058226B2 (en) | 1999-02-22 | 2011-11-15 | Baxter International Inc. | Albumin-free factor VIII formulations |
| WO2012038410A1 (en) | 2010-09-20 | 2012-03-29 | Octapharma Ag | Process for production of fibrinogen |
| WO2012066036A1 (en) | 2010-11-16 | 2012-05-24 | Octapharma Ag | A PROCESS FOR REDUCTION AND/OR REMOVAL OF FXI AND FXIa FROM SOLUTIONS CONTAINING SAID COAGULATION FACTORS |
| WO2012137199A1 (en) | 2011-04-07 | 2012-10-11 | Efranat Ltd. | Macrophage activating factor for pharmaceutical compositions |
| EP2537862A1 (en) | 2008-06-24 | 2012-12-26 | Octapharma AG | A process of purifying coagulation factor VIII |
| WO2013135684A1 (en) | 2012-03-13 | 2013-09-19 | Octapharma Ag | Improved process for production of fibrinogen and fibrinogen produced thereby |
| US8598319B2 (en) | 2005-06-29 | 2013-12-03 | Laboratoire Francais Du Fractionnement Et Des Biotechnologies | Process for separating proteins fibrinogen, factor XIII and biological glue from a solubilized plasma fraction and for preparing lyophilised concentrates of said proteins |
| US8871439B2 (en) | 2005-06-30 | 2014-10-28 | Octapharma Ag | Serum-free stable transfection and production of recombinant human proteins in human cell lines |
| AU2012201036B2 (en) * | 2003-12-01 | 2014-12-04 | Novo Nordisk Health Care Ag | Virus filtration of liquid factor VII compositions |
| US9145448B2 (en) | 2004-10-19 | 2015-09-29 | Bio Products Laboratory Limited | Method for the isolation of haptoglobin |
| WO2016071434A1 (en) * | 2014-11-05 | 2016-05-12 | Abbott Laboratories Gmbh | Processes for producing compositions with improved safety profile comprising pancreatin and compositions suitable for pharmaceutical use |
| US10512674B2 (en) | 2008-11-07 | 2019-12-24 | Baxalta Incorporated | Factor VIII formulations |
| EP3945095A1 (en) | 2020-07-28 | 2022-02-02 | Bia Separations D.O.O. | A process for the purification of prothrombin complex concentrate (pcc) and fix from complete plasma or cryo-poor plasma |
Families Citing this family (154)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4720385A (en) * | 1983-03-29 | 1988-01-19 | Miles Laboratories, Inc. | Protein compositions substantially free from infectious agents |
| US4820805A (en) * | 1983-07-14 | 1989-04-11 | New York Blood Center, Inc. | Undenatured virus-free trialkyl phosphate treated biologically active protein derivatives |
| US4831012A (en) * | 1984-03-23 | 1989-05-16 | Baxter International Inc. | Purified hemoglobin solutions and method for making same |
| US5281579A (en) * | 1984-03-23 | 1994-01-25 | Baxter International Inc. | Purified virus-free hemoglobin solutions and method for making same |
| US5185160A (en) * | 1984-06-21 | 1993-02-09 | Prp, Inc. | Platelet membrane microvesicles |
| JPS61103836A (en) * | 1984-10-24 | 1986-05-22 | Green Cross Corp:The | Fibronectin pharmaceutical preparation |
| US4670394A (en) * | 1984-11-16 | 1987-06-02 | The United States Of America As Represented By The Secretary Of The Department Of Health And Human Services | Isolation and culture of adrenal medullary endothelial cells producing blood clotting factor VIII:C |
| US4613501A (en) * | 1984-12-21 | 1986-09-23 | New York Blood Center, Inc. | Inactivation of viruses in labile blood derivatives |
| JPH0825902B2 (en) * | 1985-02-21 | 1996-03-13 | 株式会社ミドリ十字 | Method for heat treatment of γ-globulin |
| US4632980A (en) * | 1985-04-03 | 1986-12-30 | Immunologics | Ozone decontamination of blood and blood products |
| US4789545A (en) * | 1986-03-31 | 1988-12-06 | New York Blood Center, Inc. | Removal of lipid soluble process chemicals from biological materials by extraction with naturally occurring oils or synthetic substitutes thereof |
| US4841023A (en) * | 1986-06-25 | 1989-06-20 | New York Blood Center, Inc. | Inactivation of viruses in labile protein-containing compositions using fatty acids |
| US4952812A (en) * | 1986-08-26 | 1990-08-28 | Baxter International Inc. | Irradiation of blood products |
| FR2603805A1 (en) * | 1986-09-16 | 1988-03-18 | Transfusion Sanguine Assoc Rgl | PROCESS FOR THE INACTIVATION BY OZONOLYSIS OF CONTAMINANT MICROORGANISMS PRESENT IN ESSENTIALLY PROTECTED BIOLOGICAL MATERIALS, THE PRODUCTS OBTAINED AND THEIR BIOLOGICAL AND ANALYTICAL APPLICATIONS |
| DE3704550A1 (en) * | 1987-02-13 | 1988-08-25 | Behringwerke Ag | METHOD FOR INACTIVATING SUSTAINABLE VIRUSES IN A PROTEIN PREPARATION PRODUCED BY A CELL IN VITRO |
| CA1339946C (en) * | 1987-03-31 | 1998-07-07 | Michael J. Griffith | Ultrapurification process for polypeptides |
| FR2618784B1 (en) * | 1987-07-30 | 1990-04-06 | Lille Transfusion Sanguine | CONCENTRATE OF THROMBIN-COAGULABLE PROTEINS, PROCESS FOR OBTAINING SAME AND ITS USE AS A BIOLOGICAL GLUE |
| DE3730533A1 (en) * | 1987-09-11 | 1989-03-30 | Biotest Pharma Gmbh | METHOD FOR STERILIZING PLASMA OR PLASMA FACTIONS |
| DE3733181C1 (en) * | 1987-10-01 | 1989-01-19 | Biotest Pharma Gmbh | Process for the production of a high-purity, virus-safe, biologically active transferrin preparation |
| DE3877529T2 (en) * | 1987-10-23 | 1996-11-07 | Centre Regional De Transfusion | Production of highly purified human factor IX and other plasma protein concentrate and its therapeutic use. |
| EP0321835B1 (en) * | 1987-12-21 | 1994-09-28 | Miles Inc. | Gel filteration of factor VIII |
| US4909940A (en) * | 1987-12-30 | 1990-03-20 | New York Blood Center, Inc. | Extraction of process chemicals from labile biological mixtures with organic alcohols or with halogenated hydrocarbons |
| FR2630115B1 (en) * | 1988-04-14 | 1994-10-28 | Merieux Inst | PROCESS FOR STABILIZING HUMAN ALBUMIN SOLUTIONS AND SOLUTION OBTAINED |
| GB8809177D0 (en) * | 1988-04-19 | 1988-05-25 | Merrell Doe Pharmaceuticals In | Method of preventing aids transmission-resulting from blood transfusions |
| DE3825429C2 (en) * | 1988-07-27 | 1994-02-10 | Biotest Pharma Gmbh | Method for producing an intravenously administrable polyclonal immunoglobulin preparation with a high IgM content |
| US5094960A (en) * | 1988-10-07 | 1992-03-10 | New York Blood Center, Inc. | Removal of process chemicals from labile biological mixtures by hydrophobic interaction chromatography |
| JP2926728B2 (en) * | 1988-12-29 | 1999-07-28 | 吉富製薬株式会社 | Method for producing protein-containing composition |
| EP0378208B2 (en) * | 1989-01-13 | 2003-01-15 | Mitsubishi Pharma Corporation | Production method for protein-containing composition |
| JP3005979B2 (en) * | 1989-01-13 | 2000-02-07 | 吉富製薬株式会社 | Protein-containing composition |
| US5026686A (en) * | 1989-02-01 | 1991-06-25 | Washington University | Antiviral peptides |
| JP2852307B2 (en) * | 1989-02-09 | 1999-02-03 | 吉富製薬株式会社 | Method for producing protein preparation from which virus has been removed |
| US5332578A (en) * | 1989-04-14 | 1994-07-26 | Prp, Inc. | Platelet membrane microparticles |
| USH1509H (en) * | 1989-06-09 | 1995-12-05 | Eran; Harutyun | Heparin enhanced process for separating antihemophilic factor (Factor VIII) and fibronectin from cryoprecipitate |
| DE69027187T2 (en) * | 1989-06-15 | 1996-10-31 | Rorer Int Overseas | METHOD FOR INACTIVATING VIRUSES IN VIRUS POLLUTED PHARMACEUTICAL COMPOSITIONS |
| US5945098A (en) * | 1990-02-01 | 1999-08-31 | Baxter International Inc. | Stable intravenously-administrable immune globulin preparation |
| US5177194A (en) * | 1990-02-01 | 1993-01-05 | Baxter International, Inc. | Process for purifying immune serum globulins |
| US6187572B1 (en) | 1990-04-16 | 2001-02-13 | Baxter International Inc. | Method of inactivation of viral and bacterial blood contaminants |
| US5418130A (en) * | 1990-04-16 | 1995-05-23 | Cryopharm Corporation | Method of inactivation of viral and bacterial blood contaminants |
| JP3145696B2 (en) * | 1990-10-05 | 2001-03-12 | 日本ケミカルリサーチ株式会社 | Method for producing secretory immunoglobulin A preparation |
| AT395597B (en) * | 1991-01-25 | 1993-01-25 | Immuno Ag | REAGENT FOR DETERMINING FACTOR VIII ACTIVITY |
| US5110910A (en) * | 1991-03-25 | 1992-05-05 | Miles Inc. | Virucidal euglobulin precipitation |
| AT402262B (en) * | 1991-06-20 | 1997-03-25 | Immuno Ag | MEDICINAL ACTIVATED PROTEIN C |
| EP0523406B1 (en) * | 1991-07-05 | 1998-12-09 | Bayer Corporation | Use of tri(n-butyl) phosphate at low pH in solutions of biologically active proteins for enhanced virucidal activity |
| DE4125625C2 (en) * | 1991-08-02 | 1999-12-02 | Octapharma Ag Glarus | Process for the preparation of virus-inactivated immunoglobulin solutions |
| AT408191B (en) * | 1991-08-19 | 2001-09-25 | Haemosan Erzeugung Pharmazeuti | METHOD FOR INACTIVATING PRIONS |
| US5571166A (en) * | 1992-03-19 | 1996-11-05 | Medtronic, Inc. | Method of making an intraluminal stent |
| US5510077A (en) * | 1992-03-19 | 1996-04-23 | Dinh; Thomas Q. | Method of making an intraluminal stent |
| US5599352A (en) * | 1992-03-19 | 1997-02-04 | Medtronic, Inc. | Method of making a drug eluting stent |
| JPH06166634A (en) * | 1992-12-01 | 1994-06-14 | Green Cross Corp:The | Production of plasminogen-containing composition |
| US5403834A (en) * | 1992-12-07 | 1995-04-04 | Eukarion, Inc. | Synthetic catalytic free radical scavengers useful as antioxidants for prevention and therapy of disease |
| US20020055710A1 (en) * | 1998-04-30 | 2002-05-09 | Ronald J. Tuch | Medical device for delivering a therapeutic agent and method of preparation |
| SE9301582D0 (en) * | 1993-05-07 | 1993-05-07 | Kabi Pharmacia Ab | PURIFICATION OF PLASMA PROTEINS |
| CA2165065A1 (en) * | 1993-06-23 | 1995-01-05 | Henrietta Margolis-Nunno | System for viral inactivation of blood |
| PT710126E (en) | 1993-07-30 | 2004-09-30 | Aruba Internat Pty Ltd | PLASMA DISPIPING SYSTEM |
| DE4337573C1 (en) * | 1993-11-04 | 1995-05-18 | Octapharma Ag | Process for the preparation of a virus-inactivated factor VIII-containing fraction by means of chromatographic methods |
| US5486293A (en) * | 1994-03-21 | 1996-01-23 | Hemasure, Inc. | Removal of small exogenous molecules from biological fluids |
| US6372716B1 (en) * | 1994-04-26 | 2002-04-16 | Genetics Institute, Inc. | Formulations for factor IX |
| JPH07308190A (en) * | 1994-05-18 | 1995-11-28 | Green Cross Corp:The | Production of thrombin |
| US6284874B1 (en) * | 1994-06-17 | 2001-09-04 | Alpha Therapeutic Corporation | Process for separating α1-proteinase inhibitor from cohn fraction IV1 and IV4 paste |
| DE4431833C1 (en) * | 1994-09-07 | 1995-05-18 | Blutspendedienst Der Drk Lande | Prepn. of an anti-haemophilic factor from a cryo-precipitate |
| US5506127A (en) * | 1994-09-21 | 1996-04-09 | Proba; Zbigniew | Therapeutic grade thrombin produced by chromatography |
| DE4435485C1 (en) * | 1994-10-04 | 1996-03-21 | Immuno Ag | Process for obtaining high-purity von Willebrand factor |
| AUPN030794A0 (en) | 1994-12-22 | 1995-01-27 | Aruba International Pty Ltd | Discontinuous plasma or serum delipidation |
| US6034073A (en) * | 1995-04-24 | 2000-03-07 | Novavax, Inc. | Solvent detergent emulsions having antiviral activity |
| US20040053208A1 (en) * | 1995-08-29 | 2004-03-18 | V. I. TECHNOLOGIES, Inc. | Methods to selectively inactivate parasites in biological compositions |
| US6686191B1 (en) * | 1995-09-22 | 2004-02-03 | Bayer Healthcare Llc | Preparation of virally inactivated intravenously injectable immune serum globulin |
| US5741894A (en) * | 1995-09-22 | 1998-04-21 | Baxter International, Inc. | Preparation of pharmaceutical grade hemoglobins by heat treatment in partially oxygenated form |
| US6005077A (en) * | 1995-11-10 | 1999-12-21 | Immuno Aktiengesellschaft | Use of von willebrand factor and pharmaceutical formulation |
| DE19600939C1 (en) | 1996-01-12 | 1997-08-28 | Immuno Ag | Procedure for the separation of IgG and IgA |
| US5770700A (en) * | 1996-01-25 | 1998-06-23 | Genetics Institute, Inc. | Liquid factor IX formulations |
| US5616693A (en) * | 1996-07-01 | 1997-04-01 | Alpha Therapeutic Corporation | Process for seperating alpha-1-proteinase inhibitor from COHN IV1 +1V4 paste |
| US5833651A (en) * | 1996-11-08 | 1998-11-10 | Medtronic, Inc. | Therapeutic intraluminal stents |
| WO1998030230A1 (en) * | 1997-01-09 | 1998-07-16 | Yoshitomi Pharmaceutical Industries, Ltd. | Protein-containing compositions and process for producing the same |
| AT405135B (en) * | 1997-01-17 | 1999-05-25 | Immuno Ag | PREPARATION COMPREHENSIVE THIOL GROUP-PROTEINS |
| AT404358B (en) | 1997-02-04 | 1998-11-25 | Immuno Ag | METHOD FOR CHROMATOGRAPHIC CLEANING OR FRACTIONATION OF VON WILLEBRAND FACTOR FROM A VWF-CONTAINING MATERIAL |
| AT406373B (en) | 1997-02-27 | 2000-04-25 | Immuno Ag | METHOD FOR CLEANING FACTOR VIII / VWF COMPLEX BY CATION EXCHANGER CHROMATOGRAPHY |
| TW541179B (en) * | 1997-03-19 | 2003-07-11 | Green Cross Corp | Process for preparing immunoglobulin preparation |
| US6126259A (en) * | 1997-03-25 | 2000-10-03 | Trident International, Inc. | Method for increasing the throw distance and velocity for an impulse ink jet |
| CA2285935C (en) | 1997-04-08 | 2011-01-18 | Baxter Aktiengesellschaft | An immunotolerant prothrombin complex preparation |
| GB9711927D0 (en) * | 1997-06-09 | 1997-08-06 | Bristol Myers Squibb Co | Compositions useful as fibrin sealants |
| AT407159B (en) † | 1997-06-13 | 2001-01-25 | Immuno Ag | METHOD FOR DEPOSITING VIRALS AND MOLECULAR PATHOGENS FROM A BIOLOGICAL MATERIAL |
| US6203536B1 (en) | 1997-06-17 | 2001-03-20 | Medtronic, Inc. | Medical device for delivering a therapeutic substance and method therefor |
| US6106454A (en) * | 1997-06-17 | 2000-08-22 | Medtronic, Inc. | Medical device for delivering localized radiation |
| US5886154A (en) | 1997-06-20 | 1999-03-23 | Lebing; Wytold R. | Chromatographic method for high yield purification and viral inactivation of antibodies |
| US6955917B2 (en) * | 1997-06-20 | 2005-10-18 | Bayer Healthcare Llc | Chromatographic method for high yield purification and viral inactivation of antibodies |
| AT405739B (en) | 1997-09-19 | 1999-11-25 | Immuno Ag | METHOD FOR PURIFYING ANTITHROMBIN III |
| AT407117B (en) | 1997-09-19 | 2000-12-27 | Immuno Ag | FIBRINE SPONGE |
| US6015832A (en) * | 1997-12-31 | 2000-01-18 | The Regents Of The University Of Michigan | Methods of inactivating bacteria including bacterial spores |
| US6369048B1 (en) | 1998-01-12 | 2002-04-09 | V.I. Technologies, Inc. | Methods and compositions for inactivating viruses |
| US6013099A (en) * | 1998-04-29 | 2000-01-11 | Medtronic, Inc. | Medical device for delivering a water-insoluble therapeutic salt or substance |
| US6206914B1 (en) * | 1998-04-30 | 2001-03-27 | Medtronic, Inc. | Implantable system with drug-eluting cells for on-demand local drug delivery |
| US6429192B1 (en) * | 1998-06-10 | 2002-08-06 | Statens Serum Institut | Purification process for production of mannan-binding lectin and an MBL medicinal product |
| US6270672B1 (en) | 1999-08-06 | 2001-08-07 | Baxter Aktiengesellschaft | Devices and methods for removing pathogens from biological fluids |
| US6436344B1 (en) * | 1999-11-02 | 2002-08-20 | American National Red Cross | Method of inactivating pathogens |
| WO2001045719A1 (en) * | 1999-12-20 | 2001-06-28 | Mitsubishi Pharma Corporation | Virus-free plasma protein compositions treated with porous membrane and process for producing the same |
| IL150358A0 (en) * | 1999-12-22 | 2002-12-01 | Univ Pennsylvania | Cosmid dna constructs and methods of making the same |
| AUPQ486699A0 (en) * | 1999-12-23 | 2000-02-03 | Aruba International Pty Ltd | A method of treating infectious diseases |
| DE10012732A1 (en) * | 2000-03-18 | 2001-09-20 | Aventis Behring Gmbh | Thrombin composition, for use as hemostatic or as a component of fibrin glues, comprises non-covalently bonded inhibitor for stabilization |
| IL136552A (en) | 2000-06-05 | 2005-05-17 | Omrix Biopharmaceuticals Ltd | Method for the inactivation of viruses by a solvent - detergent combination and by nanofiltration |
| US20020176796A1 (en) * | 2000-06-20 | 2002-11-28 | Purepulse Technologies, Inc. | Inactivation of microbes in biological fluids |
| US7439052B2 (en) | 2000-06-29 | 2008-10-21 | Lipid Sciences | Method of making modified immunodeficiency virus particles |
| US7407662B2 (en) * | 2000-06-29 | 2008-08-05 | Lipid Sciences, Inc. | Modified viral particles with immunogenic properties and reduced lipid content |
| US20090017069A1 (en) | 2000-06-29 | 2009-01-15 | Lipid Sciences, Inc. | SARS Vaccine Compositions and Methods of Making and Using Them |
| US7407663B2 (en) * | 2000-06-29 | 2008-08-05 | Lipid Sciences, Inc. | Modified immunodeficiency virus particles |
| FI1343809T4 (en) | 2000-12-14 | 2023-09-04 | Method of preparing alpha-1 proteinase inhibitor | |
| US20020146409A1 (en) * | 2001-01-30 | 2002-10-10 | Herring Steven W. | Methods for stabilizing lyophilized blood proteins |
| US20030124616A1 (en) * | 2001-06-21 | 2003-07-03 | Jacobsen Donald W. | Homocysteinylated transthyretin |
| AU2002322284A1 (en) * | 2001-06-25 | 2003-01-08 | Lipid Sciences, Inc. | Systems and methods using multiple solvents for the removal of lipids from fluids |
| US6991727B2 (en) | 2001-06-25 | 2006-01-31 | Lipid Sciences, Inc. | Hollow fiber contactor systems for removal of lipids from fluids |
| EP1412045A4 (en) * | 2001-06-25 | 2007-05-02 | Lipid Sciences Inc | Systems and methods using a solvent for the removal of lipids from fluids |
| US20060060520A1 (en) | 2001-06-25 | 2006-03-23 | Bomberger David C | Systems and methods using a solvent for the removal of lipids from fluids |
| EP1409108A4 (en) * | 2001-06-25 | 2007-11-14 | Lipid Sciences Inc | Hollow fiber contactor systems for removal of lipids from fluids |
| US20030133829A1 (en) * | 2001-12-21 | 2003-07-17 | Baxter Healthcare Corporation | Process for inactivating pathogens in a biological material |
| US20040106556A1 (en) * | 2002-08-26 | 2004-06-03 | Yanhong Zhu | Method of treating and preventing alzheimer disease through administration of delipidated protein and lipoprotein particles |
| WO2004075931A2 (en) | 2003-02-27 | 2004-09-10 | Baxter International Inc. | Method for the validatable inactivation of pathogens in a biological fluid by irradiation |
| EP1614424B1 (en) * | 2003-04-09 | 2015-07-22 | The Chemo-Sero-Therapeutic Research Institute | Process for producing albumin preparation |
| US20050208083A1 (en) | 2003-06-04 | 2005-09-22 | Nanobio Corporation | Compositions for inactivating pathogenic microorganisms, methods of making the compositons, and methods of use thereof |
| US7393826B2 (en) * | 2003-07-03 | 2008-07-01 | Lipid Sciences, Inc. | Methods and apparatus for creating particle derivatives of HDL with reduced lipid content |
| PT2368565E (en) * | 2003-07-03 | 2015-10-19 | Hdl Therapeutics Inc | Enrichment of pre-beta high density lipoproteins |
| US20060034943A1 (en) * | 2003-10-31 | 2006-02-16 | Technology Innovations Llc | Process for treating a biological organism |
| WO2005072778A2 (en) * | 2004-01-29 | 2005-08-11 | Biosynexus, Inc. | Use of amino-oxy functional groups in the preparation of vaccines conjugates |
| KR101209162B1 (en) * | 2004-06-29 | 2012-12-06 | 리라이언스 라이프 사이언시스 프라이빗. 리미티드 | Process for improvement of virus-safe biological fluids |
| US7993580B2 (en) * | 2004-08-24 | 2011-08-09 | Baxter International Inc. | Methods for the inactivation of microorganisms in biological fluids, flow through reactors and methods of controlling the light sum dose to effectively inactivate microorganisms in batch reactors |
| AU2005229674B2 (en) * | 2004-11-18 | 2010-11-04 | Kedrion Melville Inc. | Low concentration solvent/detergent process of immuneglobulin with pre-treatment |
| EP1685852A1 (en) | 2005-02-01 | 2006-08-02 | Fondation pour la Recherche Diagnostique | Set of disposable bags for viral inactivation of biological fluids |
| US20070054834A1 (en) * | 2005-04-11 | 2007-03-08 | Nanobio Corporation | Quaternary ammonium halides for treatment of infectious conditions |
| WO2006116899A1 (en) * | 2005-04-29 | 2006-11-09 | Chengdu Kuachang Medical Industrial Limited | The system, solid phase medium, device and method for bio-fluid treatment |
| WO2006122476A1 (en) * | 2005-04-29 | 2006-11-23 | Chengdu Kuachang Medical Industrial Limited | A method of inactivating virus, treatment system and device used thereof |
| US20070036831A1 (en) * | 2005-08-09 | 2007-02-15 | Nanobio Corporation | Nanoemulsion compositions having anti-inflammatory activity |
| US20070128693A1 (en) * | 2005-12-06 | 2007-06-07 | Advantek Serum Laboratories Limited3/F | Method for the inactivation and removal of dengue virus from biological samples |
| EP1964579A1 (en) * | 2007-02-14 | 2008-09-03 | Fondation pour la Recherche Diagnostique | Preparation of virally inactivated biological fluids having high alpha-2-antiplasmin activity |
| US8222015B2 (en) * | 2007-05-11 | 2012-07-17 | Toyota Motor Engineering & Manufacturing North America, Inc. | Heat resistant bioactive composition |
| GB0710321D0 (en) * | 2007-05-30 | 2007-07-11 | Nhs Blood & Transplant | Method |
| US9956272B2 (en) | 2007-05-30 | 2018-05-01 | Bio Products Laboratory Limited | Methods for preparing factor X, activated factor X, inactivated factor X and inactivated factor Xa, and pharmaceutical compositions comprising same |
| EP2077118A1 (en) * | 2008-01-07 | 2009-07-08 | Gwo Rei Biomedical Technology Corp. | Clottable concentrate of platelet growth factors and preparation method thereof |
| JP2011515170A (en) * | 2008-03-28 | 2011-05-19 | リサーチ ファンデーション フォー メディカル デバイシズ | Method for inactivating virus in biological fluid by solvent / surfactant treatment |
| WO2010059232A1 (en) | 2008-11-20 | 2010-05-27 | Biogen Idec Ma Inc. | Arginine inactivation of viruses |
| US20100150942A1 (en) * | 2008-12-03 | 2010-06-17 | Cantor Thomas L | Affinity purified human polyclonal antibodies and methods of making and using them |
| US8647621B2 (en) | 2009-07-27 | 2014-02-11 | Fina Biosolutions, Llc | Method of producing protein-carbohydrate vaccines reduced in free carbohydrate |
| US8945895B2 (en) * | 2009-07-31 | 2015-02-03 | Baxter International Inc. | Methods of purifying recombinant ADAMTS13 and other proteins and compositions thereof |
| JP5892944B2 (en) | 2009-12-17 | 2016-03-23 | フィナ バイオソリューションズ リミテッド ライアビリティ カンパニー | Chemical reagents for the activation of polysaccharides in the manufacture of conjugate vaccines |
| DK2560738T3 (en) * | 2010-04-23 | 2019-08-26 | Serum Inst India Ltd | SIMPLE PROCEDURE FOR SIMULTANEOUS REMOVAL OF CULTURAL POLLUTANTS FROM ULTRALA LEVELS |
| EP2399613A1 (en) | 2010-06-22 | 2011-12-28 | Research Foundation For Medical Devices | Fractionation of plasma using caprylic acid |
| US8512942B2 (en) | 2010-11-29 | 2013-08-20 | New York Blood Center, Inc. | Method of blood pooling and storage |
| US20130109807A1 (en) * | 2011-10-26 | 2013-05-02 | Bio-Rad Laboratories, Inc. | Removal of virucidal agents in mixed mode chromatography |
| ES2381828B1 (en) | 2012-03-20 | 2012-11-16 | Grifols, S.A. | PROCEDURE TO OBTAIN A COMPOSITION OF IgG THROUGH THERMAL TREATMENT |
| US9534029B2 (en) | 2012-10-03 | 2017-01-03 | Csl Behring Ag | Method of purifying proteins |
| KR102231613B1 (en) | 2012-10-03 | 2021-03-25 | 체에스엘 베링 아게 | A method of purifying proteins |
| US20140154233A1 (en) | 2012-12-05 | 2014-06-05 | Csl Limited | Method of purifying therapeutic proteins |
| US10188965B2 (en) | 2012-12-05 | 2019-01-29 | Csl Behring Gmbh | Hydrophobic charge induction chromatographic depletion of a protein from a solution |
| WO2015166072A1 (en) | 2014-04-30 | 2015-11-05 | Novo Nordisk A/S | Methods for the purification of proteins using caprylic acid |
| BR112020001363A2 (en) | 2017-08-08 | 2020-08-11 | Csl Behring Ag | hemopexin formulations |
| CA3083194A1 (en) | 2017-11-22 | 2019-05-31 | Hdl Therapeutics, Inc. | Systems and methods for priming fluid circuits of a plasma processing system |
| CA3087207A1 (en) | 2017-12-28 | 2019-07-04 | Hdl Therapeutics, Inc. | Methods for preserving and administering pre-beta high density lipoprotein extracted from human plasma |
Citations (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3962421A (en) * | 1973-06-18 | 1976-06-08 | American Home Products Corporation | Method for the disruption of lipid-containing viruses |
| US4315919A (en) * | 1980-10-06 | 1982-02-16 | Edward Shanbrom | Depyrogenation process |
Family Cites Families (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| DE3033932C2 (en) * | 1980-09-10 | 1984-05-24 | Biotest-Serum-Institut Gmbh, 6000 Frankfurt | Process for the cold sterilization of preparations containing blood coagulation factor VIII |
| US4314997A (en) * | 1980-10-06 | 1982-02-09 | Edward Shanbrom | Purification of plasma protein products |
-
1983
- 1983-07-14 US US06/514,375 patent/US4540573A/en not_active Expired - Lifetime
-
1984
- 1984-06-08 AT AT84106557T patent/ATE57836T1/en not_active IP Right Cessation
- 1984-06-08 DE DE8484106557T patent/DE3483499D1/en not_active Expired - Lifetime
- 1984-06-08 EP EP84106557A patent/EP0131740B2/en not_active Expired - Lifetime
- 1984-06-18 ZA ZA844596A patent/ZA844596B/en unknown
- 1984-07-05 CA CA000458166A patent/CA1221910A/en not_active Expired
- 1984-07-11 AU AU30503/84A patent/AU563925B2/en not_active Expired
- 1984-07-12 JP JP59143386A patent/JPH06102627B2/en not_active Expired - Lifetime
Patent Citations (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3962421A (en) * | 1973-06-18 | 1976-06-08 | American Home Products Corporation | Method for the disruption of lipid-containing viruses |
| US4315919A (en) * | 1980-10-06 | 1982-02-16 | Edward Shanbrom | Depyrogenation process |
Cited By (82)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| LT3333B (en) | 1988-06-07 | 1995-07-25 | Centre Regional De Transfusion | Chromatographic separation of plasma protein and concentrates obtained by this method |
| EP0367840A1 (en) | 1988-11-05 | 1990-05-16 | Octapharma AG | Process for producing by chromatography a non-infectious antihemophilic factor with high purity |
| DE4001099A1 (en) * | 1990-01-17 | 1991-07-18 | Octapharma Ag | METHOD FOR REMOVING VIRUSES FROM BIOLOGICAL LIQUIDS |
| DE4001098A1 (en) * | 1990-01-17 | 1991-07-18 | Octapharma Ag | SUPPORTED DIALKOXYPHOSPHORIC COMPOUNDS, METHOD FOR THEIR PRODUCTION AND THEIR USE |
| DE4008852A1 (en) * | 1990-03-20 | 1991-09-26 | Octapharma Ag | METHOD FOR PRODUCING NON-INFECTIOUS BLOOD PLASMA |
| US5864016A (en) * | 1991-06-20 | 1999-01-26 | Immuno Aktiengesellschaft | Blood product, a method of producing the same and a method of determining the virus inactivation capacity of an inactivation treatment |
| AT402891B (en) * | 1991-06-20 | 1997-09-25 | Immuno Ag | METHOD FOR PRODUCING AN INACTIVATED BLOOD PRODUCT |
| US5614405A (en) * | 1991-06-20 | 1997-03-25 | Immuno Aktiengesellschaft | Method of determining the virus inactivation capacity of an inactivation treatment |
| DE4142908A1 (en) * | 1991-12-24 | 1993-07-01 | Octapharma Ag | METHOD FOR PRODUCING A VIRUS-INACTIVATED PROTHROMINE COMPLEX CONCENTRATE (PPSB) |
| US5410022A (en) * | 1992-04-24 | 1995-04-25 | Immuno Aktiengesellschaft | Method of producing a factor VIII preparation |
| US5639730A (en) * | 1992-12-16 | 1997-06-17 | Immuno Aktiengesellschaft | Method of producing a virus-safe biological preparation |
| DE4318435A1 (en) * | 1993-02-09 | 1994-08-11 | Octapharma Ag | Method for inactivating viruses that are not provided with lipid envelopes |
| WO1994017834A1 (en) * | 1993-02-09 | 1994-08-18 | Octapharma Ag | Method for inactivating viruses devoid of lipid envelopes |
| US5614493A (en) * | 1993-06-18 | 1997-03-25 | Immuno Ag | Use of human protein C for prevention and treatment of depositions of thrombocytes |
| AT407705B (en) * | 1993-08-02 | 2001-05-25 | Immuno Ag | VIRUS INACTIVATED FACTOR XA PREPARATION |
| EP0651054A1 (en) * | 1993-08-02 | 1995-05-03 | IMMUNO Aktiengesellschaft | Virus-inactivated factor Xa preparation |
| US6893856B2 (en) | 1993-12-10 | 2005-05-17 | Octapharma Ag | Process for preparing virus-inactivated factors 1X and X by membrane chromatography |
| WO1995016030A1 (en) * | 1993-12-10 | 1995-06-15 | Octapharma Ag | Purification of vitamin-k dependent proteins by membrane chromatography |
| WO1996002571A1 (en) * | 1994-07-14 | 1996-02-01 | Croix-Rouge De Belgique | Concentrate of fibrinogene obtained from blood plasma, process and plant for its preparation |
| EP0692491A1 (en) | 1994-07-14 | 1996-01-17 | IMMUNO Aktiengesellschaft | Human virus-free monomeric immunoglobulin A and method for its production |
| US5834420A (en) * | 1994-07-14 | 1998-11-10 | Croix-Rouge De Belgique | Fibrinogen concentrate obtained from blood plasma, process and plant for its preparation |
| CN1105779C (en) * | 1995-02-25 | 2003-04-16 | 奥克塔法马有限公司 | Process for the prepn. of factor IX from biological sources |
| WO1996027003A1 (en) | 1995-02-25 | 1996-09-06 | Octapharma Ag | A process for the preparation of factor ix from biological sources |
| WO1996035710A1 (en) * | 1995-05-08 | 1996-11-14 | Suomen Punainen Risti Veripalvelu | Preparation of immunoglobulin |
| DE19528221A1 (en) * | 1995-08-01 | 1997-02-06 | Blutspendedienst Der Drk Lande | Double virus-inactivated human blood plasma, blood plasma derivatives that can be produced therefrom and methods for their production |
| DE19528221C2 (en) * | 1995-08-01 | 1998-10-22 | Blutspendedienst Der Drk Lande | Process for the production of a virus-safe, therapeutic preparation from human plasma |
| US6068838A (en) * | 1996-04-29 | 2000-05-30 | Baxter Aktiengesellschaft | Purified multimerase |
| EP0934072A4 (en) * | 1996-06-26 | 2000-09-20 | Alpha Therapeutic Corp | Manufacturing process for the production of purified transferrin |
| AT405608B (en) * | 1997-04-08 | 1999-10-25 | Immuno Ag | METHOD FOR INACTIVATING PATHOGENS, ESPECIALLY VIRUSES, IN A BIOLOGICAL MATERIAL |
| US7005502B1 (en) | 1997-05-28 | 2006-02-28 | Baxter Aktiengesellschaft | Pharmaceutical preparation comprising vWF propeptide |
| US7557188B2 (en) | 1997-05-28 | 2009-07-07 | Baxter Innovations Gmbh | Methods of treating blood coagulation disorders using a pharmaceutical preparation comprising vWF propeptide |
| US7892802B2 (en) | 1997-08-28 | 2011-02-22 | Baxter Aktiengesellschaft | Fibrinogen-based tissue adhesive containing an elastase inhibitor |
| US8425947B2 (en) | 1997-08-28 | 2013-04-23 | Baxter Aktiengesellschaft | Fibrinogen-based tissue adhesive containing an elastase inhibitor |
| US7091015B1 (en) | 1997-08-28 | 2006-08-15 | Baxter Aktiengesellschaft | Fibrinogen-based tissue adhesive |
| US7459295B2 (en) | 1997-08-28 | 2008-12-02 | Baxter Aktiengesellschaft | Fibrinogen-based tissue adhesive containing an elastase inhibitor |
| US7241603B2 (en) | 1999-02-12 | 2007-07-10 | Baxter Aktiengesellschaft | Method for producing a preparation based on fibrinogen and fibronectin as well as protein compositions obtainable according to this method |
| US8765665B2 (en) | 1999-02-22 | 2014-07-01 | Baxter International Inc. | Albumin-free factor VIII formulations |
| US8372800B2 (en) | 1999-02-22 | 2013-02-12 | Baxter International Inc. | Albumin-free factor VIII formulations |
| US8058226B2 (en) | 1999-02-22 | 2011-11-15 | Baxter International Inc. | Albumin-free factor VIII formulations |
| US9352027B2 (en) | 1999-02-22 | 2016-05-31 | Baxalta Incorporated | Albumin-free factor VIII formulations |
| US9669076B2 (en) | 1999-02-22 | 2017-06-06 | Baxalta Incorporated | Albumin-free factor VIII formulations |
| US6649339B1 (en) | 1999-08-20 | 2003-11-18 | Baxter Aktiengesellschaft | Method for producing a quality assured biological sample and composition containing the same |
| WO2005054275A3 (en) * | 2003-12-01 | 2005-09-09 | Novo Nordisk Healthcare Ag | Nanofiltration of factor vii solutions to remove virus |
| CN106916802A (en) * | 2003-12-01 | 2017-07-04 | 诺和诺德医疗保健公司 | The virus filtration of liquid factor VII compositions |
| EP3594222A1 (en) * | 2003-12-01 | 2020-01-15 | Novo Nordisk Health Care AG | Virus filtration of liquid factor vii compositions |
| RU2472804C2 (en) * | 2003-12-01 | 2013-01-20 | Ново Нордиск Хелс Кеа Аг | Method of removing viruses from liquid composition containing factor vii |
| EP2275432A1 (en) * | 2003-12-01 | 2011-01-19 | Novo Nordisk Health Care AG | Nanofiltration of factor VII solutions to remove virus |
| US9102762B2 (en) | 2003-12-01 | 2015-08-11 | Novo Nordisk Healthcare Ag | Virus filtration of liquid factor VII compositions |
| AU2012201036B2 (en) * | 2003-12-01 | 2014-12-04 | Novo Nordisk Health Care Ag | Virus filtration of liquid factor VII compositions |
| EP2277915A1 (en) | 2004-02-27 | 2011-01-26 | Octapharma AG | A purified, virus safe antibody preparation |
| US9145448B2 (en) | 2004-10-19 | 2015-09-29 | Bio Products Laboratory Limited | Method for the isolation of haptoglobin |
| US9320779B2 (en) | 2005-06-29 | 2016-04-26 | Laboratoire Francais Du Fractionnement Et Des Biotechnologies | Process for separating proteins fibrinogen, factor XIII and biological glue from a solubilized plasma fraction and for preparing lyophilised concentrates of said proteins |
| US8598319B2 (en) | 2005-06-29 | 2013-12-03 | Laboratoire Francais Du Fractionnement Et Des Biotechnologies | Process for separating proteins fibrinogen, factor XIII and biological glue from a solubilized plasma fraction and for preparing lyophilised concentrates of said proteins |
| EP2772499A1 (en) | 2005-06-29 | 2014-09-03 | Laboratoire Français du Fractionnement et des Biotechnologies | Separation of plasma proteins |
| US9273325B2 (en) | 2005-06-30 | 2016-03-01 | Carola Schroeder | Serum-free stable transfection and production of recombinant human proteins in human cell lines |
| US8871439B2 (en) | 2005-06-30 | 2014-10-28 | Octapharma Ag | Serum-free stable transfection and production of recombinant human proteins in human cell lines |
| US9512457B2 (en) | 2005-06-30 | 2016-12-06 | Octapharma Ag | Serum-free stable transfection and production of recombinant human proteins in human cell lines |
| US9796986B2 (en) | 2005-06-30 | 2017-10-24 | Octapharma Ag | Serum-free stable transfection and production of recombinant human proteins in human cell lines |
| EP2537862A1 (en) | 2008-06-24 | 2012-12-26 | Octapharma AG | A process of purifying coagulation factor VIII |
| US10512674B2 (en) | 2008-11-07 | 2019-12-24 | Baxalta Incorporated | Factor VIII formulations |
| US11020459B2 (en) | 2008-11-07 | 2021-06-01 | Baxalta Incorporated | Factor VIII formulations |
| WO2011061705A1 (en) | 2009-11-18 | 2011-05-26 | Lfb Biomedicaments | Method for treating blood plasma including a step of washing by means of dispersion |
| US10214575B2 (en) | 2010-03-30 | 2019-02-26 | Octapharma Ag | Process for the purification of a growth factor protein |
| EP3133157A1 (en) | 2010-03-30 | 2017-02-22 | Octapharma AG | A process for purifying vitamin k dependent proteins |
| WO2011121020A1 (en) | 2010-03-30 | 2011-10-06 | Octapharma Ag | A process for purifying vitamin k dependent proteins such as coagulation factor ix |
| EP3040346A1 (en) | 2010-03-30 | 2016-07-06 | Octapharma AG | Process for the purification of granulocyte colony stimulating factor, g-csf |
| WO2011121031A1 (en) | 2010-03-30 | 2011-10-06 | Octapharma Ag | Process for the purification of a growth factor protein |
| US9453045B2 (en) | 2010-03-30 | 2016-09-27 | Octapharma Ag | Process for the purification of a growth factor protein |
| US9938318B2 (en) | 2010-09-20 | 2018-04-10 | Octapharma Ag | Process for production of fibrinogen |
| CN103328503A (en) * | 2010-09-20 | 2013-09-25 | 欧克塔医药公司 | Process for production of fibrinogen |
| US9371355B2 (en) | 2010-09-20 | 2016-06-21 | Octapharma Ag | Process for production of fibrinogen |
| WO2012038410A1 (en) | 2010-09-20 | 2012-03-29 | Octapharma Ag | Process for production of fibrinogen |
| CN103328503B (en) * | 2010-09-20 | 2016-08-24 | 欧克塔医药公司 | Fibrinogen production method |
| RU2649363C2 (en) * | 2010-11-16 | 2018-04-02 | Октафарма Аг | Methods for reducing and/or removing fxi and fxia from solutions containing said clotting factors |
| WO2012066036A1 (en) | 2010-11-16 | 2012-05-24 | Octapharma Ag | A PROCESS FOR REDUCTION AND/OR REMOVAL OF FXI AND FXIa FROM SOLUTIONS CONTAINING SAID COAGULATION FACTORS |
| WO2012137199A1 (en) | 2011-04-07 | 2012-10-11 | Efranat Ltd. | Macrophage activating factor for pharmaceutical compositions |
| US11401300B2 (en) | 2012-03-12 | 2022-08-02 | Octapharma Ag | Process for production of fibrinogen and fibrinogen produced thereby |
| US10112972B2 (en) | 2012-03-13 | 2018-10-30 | Octapharma Ag | Process for production of fibrinogen and fibrinogen produced thereby |
| WO2013135684A1 (en) | 2012-03-13 | 2013-09-19 | Octapharma Ag | Improved process for production of fibrinogen and fibrinogen produced thereby |
| WO2016071434A1 (en) * | 2014-11-05 | 2016-05-12 | Abbott Laboratories Gmbh | Processes for producing compositions with improved safety profile comprising pancreatin and compositions suitable for pharmaceutical use |
| EP3945095A1 (en) | 2020-07-28 | 2022-02-02 | Bia Separations D.O.O. | A process for the purification of prothrombin complex concentrate (pcc) and fix from complete plasma or cryo-poor plasma |
| WO2022023431A1 (en) | 2020-07-28 | 2022-02-03 | Bia Separations D.O.O. | A process for the purification of prothrombin complex concentrate (pcc) and fix from complete plasma or cryo-poor plasma |
Also Published As
| Publication number | Publication date |
|---|---|
| AU3050384A (en) | 1985-01-17 |
| AU563925B2 (en) | 1987-07-30 |
| EP0131740B1 (en) | 1990-10-31 |
| JPS6051116A (en) | 1985-03-22 |
| ZA844596B (en) | 1985-02-27 |
| CA1221910A (en) | 1987-05-19 |
| EP0131740A3 (en) | 1985-08-07 |
| EP0131740B2 (en) | 1994-09-28 |
| DE3483499D1 (en) | 1990-12-06 |
| US4540573A (en) | 1985-09-10 |
| JPH06102627B2 (en) | 1994-12-14 |
| ATE57836T1 (en) | 1990-11-15 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| EP0131740B1 (en) | Undenatured virus-free biologically active protein derivatives | |
| US4764369A (en) | Undenatured virus-free biologically active protein derivatives | |
| US4613501A (en) | Inactivation of viruses in labile blood derivatives | |
| US4841023A (en) | Inactivation of viruses in labile protein-containing compositions using fatty acids | |
| US4820805A (en) | Undenatured virus-free trialkyl phosphate treated biologically active protein derivatives | |
| US5094960A (en) | Removal of process chemicals from labile biological mixtures by hydrophobic interaction chromatography | |
| US4370264A (en) | Method for the cold sterilization of preparations containing blood coagulation factor VIII | |
| US4591505A (en) | Process for inactivating hepatitis B virus | |
| EP0099445B1 (en) | Sterilized plasma and plasma derivatives and process therefor | |
| US4876241A (en) | Stabilization of biological and pharmaceutical products during thermal inactivation of viral and bacterial contaminants | |
| EP0197554B1 (en) | Treatment of biological and pharmaceutical products adsorbed on a solid phase with virus and pyrogen inactivating agents | |
| US5118794A (en) | Process for stabilizing human albumin solutions and the solution obtained | |
| EP0322786B1 (en) | Extraction of process chemicals from labile biological mixtures with halogenated hydrocarbons | |
| EP0315968B1 (en) | Plasma and recombinant protein formulations in low ionic strength media | |
| JP2544619B2 (en) | Method for removing lipid soluble treatment chemicals from biological material | |
| CA2034489C (en) | Methods for the inactivation of viruses in viral-contaminated pharmaceutical compositions | |
| US5639730A (en) | Method of producing a virus-safe biological preparation | |
| US5055485A (en) | Inactivation of viruses in cell- and protein-containing compositions using aryl diol epoxides | |
| US4579735A (en) | Process for the pasteurization of human residual plasma | |
| EP0292003B1 (en) | Stabilzation of biological and pharmaceutical products during inactivation of viral and bacterial contaminants | |
| KR100696897B1 (en) | Process for the inactivation of viruses | |
| US20020018777A1 (en) | Sterilization of virus infected plasma | |
| Mozen | HIV inactivation in plasma products |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| PUAI | Public reference made under article 153(3) epc to a published international application that has entered the european phase |
Free format text: ORIGINAL CODE: 0009012 |
|
| AK | Designated contracting states |
Designated state(s): AT BE CH DE FR GB IT LI NL SE |
|
| PUAL | Search report despatched |
Free format text: ORIGINAL CODE: 0009013 |
|
| AK | Designated contracting states |
Designated state(s): AT BE CH DE FR GB IT LI NL SE |
|
| 17P | Request for examination filed |
Effective date: 19850710 |
|
| 17Q | First examination report despatched |
Effective date: 19880119 |
|
| GRAA | (expected) grant |
Free format text: ORIGINAL CODE: 0009210 |
|
| AK | Designated contracting states |
Kind code of ref document: B1 Designated state(s): AT BE CH DE FR GB IT LI NL SE |
|
| REF | Corresponds to: |
Ref document number: 57836 Country of ref document: AT Date of ref document: 19901115 Kind code of ref document: T |
|
| REF | Corresponds to: |
Ref document number: 3483499 Country of ref document: DE Date of ref document: 19901206 |
|
| ET | Fr: translation filed | ||
| ITF | It: translation for a ep patent filed |
Owner name: SOCIETA' ITALIANA BREVETTI S.P.A. |
|
| PLBI | Opposition filed |
Free format text: ORIGINAL CODE: 0009260 |
|
| 26 | Opposition filed |
Opponent name: IMMUNO AKTIENGESELLSCHAFT Effective date: 19910713 |
|
| NLR1 | Nl: opposition has been filed with the epo |
Opponent name: IMMUNO AKTIENGESELLSCHAFT |
|
| ITTA | It: last paid annual fee | ||
| PUAA | Information related to the publication of a b2 document modified |
Free format text: ORIGINAL CODE: 0009299PMAP |
|
| PUAH | Patent maintained in amended form |
Free format text: ORIGINAL CODE: 0009272 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: PATENT MAINTAINED AS AMENDED |
|
| ITF | It: translation for a ep patent filed |
Owner name: SOCIETA' ITALIANA BREVETTI S.P.A. |
|
| 27A | Patent maintained in amended form |
Effective date: 19940928 |
|
| AK | Designated contracting states |
Kind code of ref document: B2 Designated state(s): SE |
|
| R27A | Patent maintained in amended form (corrected) |
Effective date: 19940928 |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: AEN |
|
| NLR2 | Nl: decision of opposition | ||
| ET3 | Fr: translation filed ** decision concerning opposition | ||
| EAL | Se: european patent in force in sweden |
Ref document number: 84106557.6 |
|
| NLR3 | Nl: receipt of modified translations in the netherlands language after an opposition procedure | ||
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: NV Representative=s name: BUGNION S.A. |
|
| ET3 | Fr: translation filed ** decision concerning opposition | ||
| REG | Reference to a national code |
Ref country code: GB Ref legal event code: IF02 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: AT Payment date: 20030521 Year of fee payment: 20 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: NL Payment date: 20030522 Year of fee payment: 20 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: GB Payment date: 20030604 Year of fee payment: 20 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: SE Payment date: 20030619 Year of fee payment: 20 Ref country code: FR Payment date: 20030619 Year of fee payment: 20 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: CH Payment date: 20030623 Year of fee payment: 20 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: DE Payment date: 20030630 Year of fee payment: 20 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: BE Payment date: 20030711 Year of fee payment: 20 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LI Free format text: LAPSE BECAUSE OF EXPIRATION OF PROTECTION Effective date: 20040607 Ref country code: GB Free format text: LAPSE BECAUSE OF EXPIRATION OF PROTECTION Effective date: 20040607 Ref country code: CH Free format text: LAPSE BECAUSE OF EXPIRATION OF PROTECTION Effective date: 20040607 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: NL Free format text: LAPSE BECAUSE OF EXPIRATION OF PROTECTION Effective date: 20040608 Ref country code: AT Free format text: LAPSE BECAUSE OF EXPIRATION OF PROTECTION Effective date: 20040608 |
|
| BE20 | Be: patent expired |
Owner name: *NEW YORK BLOOD CENTER INC. Effective date: 20040608 |
|
| REG | Reference to a national code |
Ref country code: GB Ref legal event code: PE20 |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: PL |
|
| NLV7 | Nl: ceased due to reaching the maximum lifetime of a patent |
Effective date: 20040608 |
|
| EUG | Se: european patent has lapsed |